Abstract
Objectives Gestational diabetes mellitus (GDM) substantially increases a woman’s lifetime risk of developing type 2 diabetes mellitus (DM). Lifestyle modification interventions have been effective in preventing DM in high-risk populations but present challenges in diverse, postpartum women. We systematically reviewed the literature to synthesize current knowledge and practices around tailoring multimodal, primarily home-based interventions for situational and cultural relevance to reduce DM risk in women with prior GDM. Methods We identified original research articles published from January 2000 through July 2015 describing randomized controlled trials testing multimodal interventions to reduce DM risk in women with prior GDM. We compared articles by study objective, delivery modes, intervention components, degree of individualization, theoretical basis, design, population, outcome variables, and findings. Results Ten studies met the inclusion criteria. Telephone and mailings (n = 7) and websites (n = 3) were the primary modes of participant contact in these primarily home-based interventions. These studies demonstrate that individualizing interventions may contribute to increased postpartum weight loss and improved dietary behaviors; however, researchers remain challenged to improve physical activity in this population. Additionally, even when testing primarily home-based interventions, recruitment rates were very low, underscoring challenges of engaging this population in lifestyle changes. Conclusions Postpartum interventions addressing the broader social-ecological dimensions of health behaviors should be tested in women with prior GDM. Researchers and clinicians must continue to explore ways to engage women, including women’s families and communities, in interventions to adequately address the sociocultural determinants that affect women’s lifestyle behaviors impacting their DM risk.
Similar content being viewed by others
Significance
Several pilot and feasibility studies have demonstrated promise in improving health behaviors to reduce diabetes risk in women with prior GDM yet, larger randomized controlled trials are needed to assess the efficacy of postpartum lifestyle interventions on curbing diabetes progression in this population. Given the persistent challenges of engaging women with prior GDM in lifestyle behavioral change interventions, greater effort should be made to engage women’s families and communities to provide necessary social support. Researchers must design and test interventions accounting for the broader social-ecological determinants of postpartum women’s health behaviors in addition to individual-level determinants.
Introduction
Current prevalence estimates of type 2 diabetes mellitus (DM) in the United States (U.S.) approach 29.1 million, or 9.3 % of the U.S. population, and ethnic minority populations experience DM disproportionately (Centers for Disease Control and Prevention 2014). Women with a history of gestational diabetes mellitus (GDM), or glucose intolerance first diagnosed during pregnancy, are frequently overlooked for primary prevention of DM (McCloskey et al. 2014). This population has a seven to 12-fold lifetime risk for the subsequent development of DM with a 20–50 % chance of developing DM in the 5–10 years following the index GDM pregnancy (American Diabetes Association 2014; Bellamy et al. 2009). Furthermore, DM develops disproportionately among ethnically diverse women with prior GDM, with cumulative incidence approaching 60–70 % in East Indian and American Indian women, respectively (Kim et al. 2002). Importantly, a post hoc analysis of racially and ethnically diverse women with self-reported, remote histories of GDM in the Diabetes Prevention Program (DPP) demonstrated that women randomized to an intensive lifestyle program, aimed at reducing weight and increasing physical activity, had a 53 % risk reduction for DM (Ratner et al. 2008). Observational 10-year follow-up of this landmark study revealed that both lifestyle changes and metformin were highly effective in reducing DM progression in women with prior GDM (Aroda et al. 2015).
Since GDM diagnosis may heighten a woman’s risk perception for her health and that of her offspring, recent motherhood presents an underappreciated window of opportunity for prevention (Bentley-Lewis et al. 2008; Jones et al. 2012; Nicklas et al. 2011). However, implementing interventions to reduce weight and increase physical activity in this population is challenging due to women’s competing priorities and demands (Ferrara and Ehrlich 2011). Researchers, clinicians, and communities are challenged to identify effective ways to address the complex individual, interpersonal, and sociocultural factors that impact women’s lifestyle behaviors during and following GDM-affected pregnancy.
Despite demonstrated efficacy of lifestyle behavioral modification in preventing DM (Knowler et al. 2009), relatively little is known regarding how to effectively translate prevention in high-risk, ethnically diverse women with prior GDM. Tailoring interventions for situational and cultural relevance has emerged as a promising approach to eliminate health disparities in vulnerable populations (Institute of Medicine 2003). Numerous barriers to postpartum lifestyle changes exist for women with prior GDM, and these same barriers may make it difficult to engage women in face-to-face interventions (Jones et al. 2015; Nicklas et al. 2011; Razee et al. 2010). Therefore, the purpose of this systematic review was to synthesize current knowledge and practices around tailoring multimodal interventions for situational and cultural relevance to reduce DM risk in women with prior GDM. We followed the framework for Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) to report our findings (Moher et al. 2009).
Methods
We systematically searched MEDLINE and CINAHL databases to identify relevant English language, original research articles published electronically or in print from January 2000 through July 2015. The lead author conducted the final search in August 2015. Search terms included: gestational diabetes mellitus, type 2 diabetes mellitus, prevention, health behavior, postpartum, postpartum program, and lifestyle intervention. Inclusion criteria were: (a) study sample of women with prior GDM; (b) lifestyle modification intervention to reduce DM risk; (c) multimodal, primarily home-based intervention, thus not fully reliant on face-to-face mode of delivery; (d) clear elements of situational and/or cultural tailoring in interventions; (e) randomized controlled trial (RCT). We limited the review to quantitative studies that described completed or recently launched interventions.
We used a two-step exclusion process to identify relevant articles. First, the study’s lead author reviewed the titles and abstracts to determine if they met inclusion criteria. If there was concern about inclusion, the other authors reviewed the article to determine if the article met inclusion criteria. After excluding duplicates and irrelevant articles, the lead author and second author then reviewed each remaining full article to determine if it met the criteria. We categorized included articles according to whether the intervention was initiated during pregnancy and continued postpartum or initiated during the postpartum period. We compared articles by study objective, intervention delivery modes, intervention components, degree of individualization, theoretical basis, design, population, outcome variables, and findings, when applicable (Tables 1, 2). We assessed risk of bias at the study-level using the domain-based evaluation recommended by the Cochrane Collaboration (Higgins and Green 2011).
Results
The initial search yielded 805 articles (Fig. 1); after screening to remove duplicates and irrelevant articles, we identified 38 full-text articles to be reviewed in-depth by two authors (H.E.F., E.J.J.). This resulted in the selection of 19 articles for full review; nine of these met inclusion criteria. We hand-searched articles included in two relevant systematic reviews (Chasan-Taber 2015; Morton et al. 2014) and identified one additional article for inclusion. Therefore, we will present results from a final sample of ten articles.
Multimodal Interventions Initiated During Pregnancy
Telephone and Mailings as Primary Modes of Contact
Three RCTs were initiated during the third trimester of pregnancy, soon after confirmation of GDM (Tables 1, 2). Of these, one pilot RCT and two RCT protocols described health-behavior change interventions delivered or to be delivered primarily via telephone and mailings with minimal or no face-to-face sessions during the studies’ year long duration. Ferrara et al. (2011) and Chasan-Taber et al. (2014) included one individual, face-to-face session at the initiation of the prenatal phase and one at the initiation of the early postpartum (active) phase. Ferrara et al. (2011) included a second face-to-face session at the conclusion of the early postpartum phase. With no face-to-face sessions, Ferrara et al. (2014) describe an interactive program-specific website to supplement their intervention’s telephone sessions and mailings.
The completed pilot RCT (Ferrara et al. 2011) included 197 participants; Chasan-Taber et al. (2014) aim to recruit 300 participants, while Ferrara et al. (2014) are recruiting from a pool of 2320 eligible women. Each study’s intervention is divided into three distinct phases: prenatal (third trimester), early postpartum (6-weeks to 6- to 7-months postpartum), and late postpartum (6- to 7-months to 12 months postpartum). The goal of the prenatal phase focuses on optimizing gestational weight gain and on preparing women for DM prevention following GDM; in the pilot RCT (Ferrara et al. 2011), this phase also aimed to increase women’s breastfeeding support following delivery. The shared goal of the interventions’ second (active) phase is to assist women to set postpartum dietary, physical activity, and weight loss goals and problem-solve around barriers to achieving those goals. The goal of the interventions’ third (maintenance) phase is to foster women’s independence in maintaining positive behavior changes established in the active period.
These three highly individualized interventions reflect situational and cultural relevance for a racially and ethnically diverse sample of women with GDM in northern California (Ferrara et al. 2011, 2014) and Hispanic women with GDM in western Massachusetts (Chasan-Taber et al. 2014). Both studies by Ferrara and colleagues were adapted from the DPP, but by using telephone sessions and mailings as the primary modes of participant contact, rather than individual, face-to-face counseling sessions, each intervention was tailored for recent motherhood. These interventions seek to accommodate women’s busy lives and limited time for face-to-face interaction and to promote accountability via regular contact with a lifestyle coach/interventionist. Each intervention relied/relies heavily on using motivational interviewing principles, tailored questionnaires, and self-monitoring diaries to individualize the interventions according to women’s goals, preferences, and available resources. The two RCT protocols specify using multi-language materials to ensure cultural and linguistic relevance (Chasan-Taber et al. 2014; Ferrara et al. 2014); additionally, Ferrara et al. (2014) describe using bilingual (English/Spanish) lifestyle coaches. In each of these studies, the authors specified drawing from social cognitive theory (SCT) (Bandura 1986) and the Transtheoretical Model (TTM) (Prochaska and Velicer 1997) to address self-efficacy, social support, and stages of change.
Results from the pilot RCT (Ferrara et al. 2011) indicated that a greater proportion of women in the intervention arm reached their postpartum weight goals, decreased their dietary fat intake, and increased breastfeeding compared to women receiving usual care, although none of these differences achieved statistical significance. No differences were observed between the two groups related to postpartum physical activity. The study was limited by a small sample size and risk for attrition bias due to loss to follow-up differences between the intervention and control arms of the study. Yet, importantly, this pilot study demonstrated that a lifestyle behavior-change intervention initiated during pregnancy and continued through the first postpartum year is feasible and shows promise for reducing pregnancy weight retention.
Chasan-Taber et al. (2014) and Ferrara et al. (2011, 2014) specify procedures to reduce the risk of detection bias by blinding outcome assessors from knowledge of intervention allocation. However, given the nature of the lifestyle interventions and self-reported measures within the studies, each study presents a high risk of performance bias due to the participants’ knowledge of intervention allocation and the added potential for recall or social desirability biases.
Multimodal Interventions Initiated Postpartum
Telephone and Mailings as Primary Modes of Contact
Seven RCTs were initiated during the postpartum period (Tables 1, 2). Of these, four Australian studies, including three pilot RCTs and one RCT, described interventions delivered primarily via telephone and mailings with no or minimal (one to two) face-to-face sessions during the intervention timeframes, ranging from 12-weeks to 1 year. Three interventions included one individual, face-to-face session with an expert interventionist at initiation (Cheung et al. 2011; McIntyre et al. 2012; Smith et al. 2014); Smith and colleagues additionally included a second face-to-face session 2-weeks after the first. Study samples ranged from 28 to 59 participants. The goal of two interventions was to improve physical activity and healthy eating behaviors during the immediate/early postpartum period (Reinhardt et al. 2012) and within 6 months to 4 years out from a GDM-affected pregnancy (Smith et al. 2014). The other two interventions sought only to increase physical activity during the immediate/early postpartum period (McIntyre et al. 2012) and within the first 4 years following GDM (Cheung et al. 2011).
By using flexible modes of participant contact and individualizing the interventions at varying degrees, these interventions reflect situational and cultural relevance for geographically (rural versus urban) and socioeconomically diverse samples of women with prior GDM in Australia. All studies involved patient-centered counseling by expert interventionists to individualize the interventions in terms of cultural needs, goal-setting, and ongoing support to initiate and maintain behavioral change. By using pedometers, researchers in two studies tailored the intervention according to participants’ baseline physical activity levels and ongoing progress toward goal achievement (Cheung et al. 2011; Smith et al. 2014). Reinhardt et al. (2012) and Smith et al. (2014) also provided participants with physical activity and dietary journals to promote behavioral self-monitoring. In addition to telephone calls and mailings, Smith et al. (2014) supplemented the intervention with SMS/text messages.
McIntyre et al. (2012) specified drawing from SCT; while the other authors did not specify particular theoretical underpinnings, they each discussed embedding behavioral constructs that align closely to those represented in SCT such as self-regulation and self-sufficiency (Cheung et al. 2011), health beliefs, perceived barriers, perceived benefits, and social support (Reinhardt et al. 2012), and self-efficacy and barriers to change (Smith et al. 2014).
Results from the RCT with 59 racially and ethically diverse women living in New South Wales (Smith et al. 2014) indicated that women in the intervention arm achieved statistically significant improvements in caloric, total and saturated fats, and carbohydrate intake but did not improve physical activity. The authors note a lack of power for detecting intervention effects due to loss to follow-up.
Results from the three pilot RCTs were mixed. Findings from the 12-month pilot RCT with 43 women (Cheung et al. 2011) showed that women in the intervention arm met the primary physical activity target at a significantly greater rate than women in the control arm. However, the authors noted difficulty in recruiting enough participants to detect differences in long-term DM risk along with significant resource-related challenges in conducting such a large-scale intervention study. Findings from the 12-week pilot RCT with 28 women (McIntyre et al. 2012) demonstrated improvements in planned physical activity in the intervention group, but no changes were achieved in biophysical/anthropometric measures in either group. Although participant retention was a strength, limitations of this study included poor recruitment rates, small sample size, and short duration of follow-up. Lastly, findings from the 6-month pilot RCT with 38 women in rural, northern New South Wales (Reinhardt et al. 2012) demonstrated that women in the intervention arm achieved significant improvements in total fat and carbohydrate intake, glycemic load, and body mass index. This group also increased leisure time physical activity; however, no significant changes in total physical activity levels occurred.
In all four reviewed studies that were initiated in the postpartum period and utilized telephone and mailings as the primary mode of contact, authors noted poor recruitment and participation rates as a major limitation. In addition, risk of performance bias is high due to participants’ and study personnel’s knowledge of active intervention assignment, and risk of recall and social desirability biases is high due to the self-reported measures. Risk of detection bias is unclear as the authors do not provide details regarding blinding of outcome assessment. Challenges related to participant retention and subsequent loss to follow up (Cheung et al. 2011; Reinhardt et al. 2012; Smith et al. 2014) present some risk of attrition bias in these studies, as well, although Reinhardt et al. (2012) and Smith et al. (2014) specify analytic procedures to address that risk.
Website as Primary Mode of Contact
Three of the seven RCTs initiated postpartum tested web-based interventions as the primary mode of contact. Two interventions required no face-to-face contact with participants; of these, one was initiated in the early postpartum period (Nicklas et al. 2014) and one within 3 years postpartum (Kim et al. 2012). One study tested a web-based intervention supplemented with four face-to-face counseling sessions (Peacock et al. 2015). The aim of the DPP-adapted lifestyle intervention with diverse, urban-dwelling women in Boston, Massachusetts, was to decrease postpartum weight retention (Nicklas et al. 2014). With a broader focus, the aims of the pedometer interventions with women in Michigan (Kim et al. 2012) and Brisbane, Australia, (Peacock et al. 2015) were to examine the interventions’ impact on women’s physical activity behaviors, anthropometrics, and insulin and glucose levels.
Using online educational modules, all interventions were situationally relevant for postpartum women. These interventions provided individualized feedback regarding progress towards goals through web-linked pedometers (Kim et al. 2012; Peacock et al. 2015), text-messaging (Kim et al. 2012) and optional, self-initiated counseling sessions via email or telephone with a lifestyle coach (Nicklas et al. 2014). Nicklas and colleagues also provided participants with pedometers, complementary YMCA memberships, body scales, and journals to promote behavioral self-monitoring, but noted that these were underutilized. To promote interaction among participants, Kim and colleagues provided an online messaging board; however, only three women used this feature to reach study staff, not other participants. Each of these RCTs included English-only speakers; methods to ensure cultural relevance for individual participants were not explicit.
While the authors did not specify particular theoretical foundations, the DPP-adapted program by Nicklas et al. (2014) embedded behavioral constructs from the SCT and TTM, and Kim et al. (2012) and Peacock et al. (2015) discussed addressing behavioral constructs that closely align with SCT such as self-efficacy, perceived risk, social support, and behavioral goals.
While results from Kim and colleagues’ intervention demonstrate feasibility, they found that the structured web-based education had small impact on weight and insulin and minimal impact on health behaviors, and intervention uptake was low. In contrast, the web-based interventions supplemented with individual counseling and self-monitoring (Nicklas et al. 2014) and face-to-face, group-based nutrition counseling and self-monitoring (Peacock et al. 2015) demonstrated both feasibility and efficacy to decrease weight in women with prior GDM. Additionally, Peacock et al. (2015) demonstrated clinical improvement in physical activity and eating behavior; however, significant differences in physical activity between groups were not detected in any of the studies.
All authors noted low recruitment rates as a significant challenge. Further, each of the three web-based intervention studies poses risk of performance bias due to knowledge of intervention allocation by participants as well as recall and social desirability biases related to the self-reported measures. Nicklas et al. (2014) report measures taken to reduce risk of detection and attrition biases, while Kim et al. (2012) and Peacock et al. (2015) do not provide sufficient details to estimate such risk.
Discussion
Overall, the studies reviewed demonstrate the applicability and feasibility of multimodal, primarily home-based interventions to promote postpartum lifestyle behavioral change following GDM. Findings suggest that individualizing interventions for situational and cultural relevance may contribute to improved outcomes in terms of postpartum weight loss and dietary behaviors. However, in the eight completed studies reviewed, the authors noted no statistically significant changes in women’s postpartum physical activity behaviors, underscoring the challenges inherent in improving physical activity in women who struggle to balance competing priorities and time constraints. Additionally, the majority of authors reported poor recruitment rates, underscoring challenges to engage women and improve health in this population. Furthermore, only Ferrara et al. (2014) described a plan to analyze the cost effectiveness of their intervention, a key element of feasibility and sustainability.
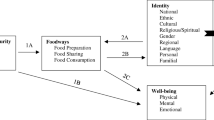
Based on this review, several overarching lessons emerge for researchers in this field. First, the careful embedding of behavioral constructs in the interventions is crucial. A study’s underlying theoretical framework clearly influences the way researchers design the interventions, selecting both modes of delivery and methods of participant engagement congruent with key constructs such as self-efficacy, perceived barriers to change, and self-regulation. However, even with careful attention to these constructs, researchers struggled to change women’s physical activity behaviors. This could, in part, be related to the fact that the SCT and TTM are focused primarily at the individual level and not the broader socio-ecological level. Perhaps dietary behaviors are more amenable to change than physical activity behaviors due to time constraints that are socially influenced by maternity leave policies, traditional workday hours, and childcare practices impacting women in the first postpartum year. Researchers acknowledge the need to target physical activity determinants at various levels of the social-ecological continuum in interventions aimed at preventing unhealthy weight in children (Kellou et al. 2014). Similarly, we suggest that interventions that carefully consider the social-ecological dimensions of health behaviors, beyond the individual level, should be tested for relevance in women with prior GDM. For example, interventions designed to impact women’s physical activity behaviors should address family, community, and/or societal influences on these behaviors.
Findings also suggest that those interventions beginning in pregnancy and continuing postpartum capitalize on the ‘teachable moments’ during GDM-affected pregnancy and may facilitate a smoother transition to sustain lifestyle-related behavioral changes during the complex postpartum period (Chasan-Taber et al. 2014; Ferrara et al. 2011, 2014). Additionally, those interventions that were individualized to greater degrees and incorporated methods of behavioral self-monitoring such as food and physical activity diaries and pedometers demonstrated greater improvements in behavior change (Cheung et al. 2011; Ferrera et al. 2011; Nicklas et al. 2014; Peacock et al. 2015; Reinhardt et al. 2012; Smith et al. 2014). Regular, supportive interactions through ongoing, individualized coaching over longer study duration appear to be key in improving health behaviors during the postpartum period. A longer intervention phase coupled with a phase of supported transition to independence may help sustain health benefits over time in this high-risk population.
Finally, researchers must continue to explore solutions to barriers that result in poor recruitment rates in this population as successful scaling up of effective interventions depends on successful recruitment and retention. Several authors specifically mentioned using qualitative methods to inform their interventions, but this could also be particularly useful for determining the most-effective recruitment and retention methods. Using mixed-methods approaches to incorporate participant voices in the intervention development phase may be critical to designing effective, sustainable interventions (Creswell et al. 2011), particularly when participants are from underserved or understudied high-risk groups who develop diabetes disparately following GDM.
Overall, these studies show promise in demonstrating the feasibility of multimodal, primarily home-based interventions in addressing the barrier of time constraints that make participating in face-to-face interventions challenging for childbearing women. However, researchers need to further explore the feasibility of family-based and community-based interventions to reduce DM risk in women with prior GDM, such as the Croí MyAction community lifestyle modification program in Ireland (Infanti et al. 2013). Since some childbearing women may predominantly view their own behaviors in the context of family health behaviors and rely on families for crucial social support (Jones et al. 2015), a family-focused lifestyle program could be a motivating approach to engage women in lifestyle change following GDM.
Across the ten studies, interventions were based on the underlying assumption that the postpartum period is a unique time of transition. If women are to be successful in changing lifestyle behaviors during this adaptive life stage, ample social support and, perhaps, direct support from expert interventionists are essential. However, researchers should also explore the effectiveness of interventions incorporating social support from lay community health workers or peers. This approach has been effective in improving diabetes self-management in vulnerable populations (Kim et al. 2015) and in promoting exclusive breastfeeding in underserved women (Coutinho et al. 2014) and should be tested as a DM delay or prevention strategy in women with prior GDM.
There were several limitations of this review. First, by setting our inclusion criteria more narrowly than prior systematic reviews in this area to capture only those trials that used multimodal, primarily home-based interventions, we did not review family-focused, face-to-face interventions that may be relevant and effective. In addition, the majority of studies reviewed were pilot RCTs, therefore, while we can draw some conclusions about feasibility, we cannot estimate the overall efficacy of the interventions since the small sample sizes in many of the studies limited the power to detect differences in outcomes. Furthermore, primary outcomes varied across studies, so it is challenging to estimate risk of bias across studies in this review. However, all studies reviewed present risk for performance bias given the nature of the lifestyle interventions and participants’ knowledge of intervention assignment. Additionally, the inclusion of self-reported measures within studies results in high risk for measurement bias, specifically recall or social desirability bias. It is unclear if these biases resulted in overestimation of the intervention effect on self-reported dietary and physical activity measures in the review studies. Lastly, this review is subject to both publication bias and publication language bias as unpublished studies and those published in a language other than English were not included.
This review highlights a limited number of studies testing multimodal, primarily home-based, and highly individualized lifestyle interventions to reduce DM risk in women with prior GDM, and, thus, demonstrates why more research is required in this important area of maternal child health. These interventions have great potential to reduce DM risk, especially in women from diverse sociocultural groups who progress to DM at disparate rates. Future studies could add much to the existing literature by focusing on these women in particular, utilizing behavioral theories and mixed-methods designs to inform the interventions. Interventions should ideally begin during pregnancy, facilitating a smoother transition to the postpartum period and first postpartum year, and they should promote accountability through behavioral self-monitoring as well as supportive coaching. Researchers must continue to explore cost-effective, innovative ways to include women’s families and communities in interventions to provide ample social support and address the broader sociocultural determinants that affect women’s daily lifestyle choices impacting their DM risk following GDM.
References
American Diabetes Association. (2014). Standards of medical care in diabetes – 2014. Diabetes Care, 37(Suppl. 1), S14–S80. doi:10.2337/dc14-S014.
Aroda, V. R., Christophi, C. A., Edelstein, S. L., Zhang, P., Herman, W. H., Barrett-Connor, E., et al. (2015). The effect of lifestyle intervention and metformin on preventing or delaying diabetes among women with and without gestational diabetes: The Diabetes Prevention Program outcomes study 10-year follow-up. Journal of Clinical Endocrinology and Metabolism, 100, 1646–1653. doi:10.1210/jc.2014-3761.
Bandura, A. (1986). Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice Hall.
Bellamy, L., Casas, J. P., Hingorani, A. D., & Williams, D. (2009). Type 2 diabetes mellitus after gestational diabetes: A systematic review and meta analysis. Lancet, 373, 1773–1779. doi:10.1016/S0140-6736(09)60731-5.
Bentley-Lewis, R., Levkoff, S., Stuebe, A., & Seely, E. W. (2008). Gestational diabetes mellitus: Postpartum opportunities for the diagnosis and prevention of type 2 diabetes mellitus. Nature Clinical Practice Endocrinology & Metabolism, 4, 552–558. doi:10.1038/ncpendmet0965.
Centers for Disease Control and Prevention. (2014). National diabetes statistics report: Estimates of diabetes and its burden in the United States, 2014. Atlanta, GA: U.S. Department of Health and Human Services. Retrieved from http://www.cdc.gov/diabetes/pubs/statsreport14/national-diabetes-report-web.pdf.
Chasan-Taber, L. (2015). Lifestyle interventions to reduce risk of diabetes among women with prior gestational diabetes mellitus. Best Practice and Research. Clinical Obstetrics & Gynaecology, 29, 110–122. doi:10.1016/j.bpobgyn.2014.04.019.
Chasan-Taber, L., Marcus, B. H., Rosal, M. C., Tucker, K. L., Hartman, S. J., Pekow, P., et al. (2014). Estudio Parto: Postpartum diabetes prevention program for Hispanic women with abnormal glucose tolerance in pregnancy: A randomised controlled trial—study protocol. BMC Pregnancy and Childbirth, 14, 100. doi:10.1186/1471-2393-14-100.
Cheung, N. W., Smith, B. J., van der Ploeg, H. P., Cinnadaio, N., & Bauman, A. (2011). A pilot structured behavioural intervention trial to increase physical activity among women with recent gestational diabetes. Diabetes Research and Clinical Practice, 92, e27–e29. doi:10.1016/j.diabres.2011.01.013.
Coutinho, S. B., Lira, P. I., Lima, M. C., Frias, P. G., Eickmann, S. H., & Ashworth, A. (2014). Promotion of exclusive breast-feeding at scale within routine health services: Impact of breast-feeding counselling training for community health workers in Recife, Brazil. Public Health Nutrition, 17, 948–955. doi:10.1017/S1368980013001833.
Creswell J. W., Klassen A. C., Plano Clark V. L., & Smith K. C. For the Office of Behavioral and Social Sciences Research. (2011). Best practices for mixed methods research in the health sciences. National Institutes of Health. Retrieved from http://obssr.od.nih.gov/mixed_methods_research.
Ferrara, A., & Ehrlich, S. F. (2011). Strategies for diabetes prevention before and after pregnancy in women with GDM. Current Diabetes Reviews, 7, 75–83.
Ferrara, A., Hedderson, M. M., Albright, C. L., Brown, S. D., Ehrlich, S. F., Caan, B. J., et al. (2014). A pragmatic cluster randomized clinical trial of diabetes prevention strategies for women with gestational diabetes: Design and rationale of the Gestational Diabetes’ Effects on Moms (GEM) study. BMC Pregnancy and Childbirth, 14, 21. doi:10.1186/1471-2393-14-21.
Ferrara, A., Hedderson, M. M., Albright, C. L., Ehrlich, S. F., Quesenberry, C. P, Jr., Peng, T., et al. (2011). A pregnancy and postpartum lifestyle intervention in women with gestational diabetes mellitus reduces diabetes risk factors: A feasibility randomized control trial. Diabetes Care, 34, 1519–1525. doi:10.2337/dc10-2221.
Higgins, J. P. T., Green, S. (Editors). (2011). Cochrane handbook for systematic reviews of interventions. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration. www.cochrane-handbook.org.
Infanti, J. J., Dunne, F. P., O’Dea, A., Gillespie, P., Gibson, I., Glynn, L. G., et al. (2013). An evaluation of Croí MyAction community lifestyle modification programme compared to standard care to reduce progression to diabetes/pre-diabetes in women with prior gestational diabetes mellitus (GDM): Study protocol for a randomised controlled trial. Trials, 14, 121. doi:10.1186/1745-6215-14-121.
Institute of Medicine. (2003). Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, DC.: National Academies Press. Retrieved from http://www.nap.edu/openbook.php?record_id=10260&page=R1.
Jones, E. J., Appel, S. J., Eaves, Y. D., Moneyham, L., Oster, R. A., & Ovalle, F. (2012). Cardiometabolic risk, knowledge, risk perception, and self-efficacy among American Indian women with previous gestational diabetes. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 41, 246–257. doi:10.1111/j.1552-6909.2012.01339.x.
Jones, E. J., Peercy, M., Woods, J. C., Parker, S. P., Jackson, T., Mata, S. A., et al. (2015). Identifying postpartum intervention approaches to reduce cardiometabolic risk among American Indian women with prior gestational diabetes, Oklahoma, 2012–2013. Preventing Chronic Disease, 12, E45. doi:10.5888/pcd12.140566.
Kellou, N., Sandalinas, F., Copin, N., & Simon, C. (2014). Prevention of unhealthy weight in children by promoting physical activity using a socio-ecological approach: What can we learn from intervention studies? Diabetes and Metabolism, 40, 258–271. doi:10.1016/j.diabet.2014.01.002.
Kim, C., Draska, M., Hess, M. L., Wilson, E. J., & Richardson, C. R. (2012). A web-based pedometer programme in women with a recent history of gestational diabetes. Diabetic Medicine, 29, 278–283. doi:10.1111/j.1464-5491.2011.03415.x.
Kim, M. T., Kim, K. B., Huh, B., Nguyen, T., Han, H. R., Bone, L. R., et al. (2015). The effect of a community-based self-help intervention: Korean Americans with type 2 diabetes. American Journal of Preventive Medicine. doi:10.1016/j.amepre.2015.04.033.
Kim, C., Newton, K. M., & Knopp, R. H. (2002). Gestational diabetes and the incidence of type 2 diabetes: A systematic review. Diabetes Care, 25, 1862–1868.
Knowler, W. C., Fowler, S. E., Hamman, R. F., Christophi, C. A., Hoffman, H. J., Brenneman, A. T., et al. (2009). 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet, 374, 1677–1686. doi:10.1016/S0140-6736(09)61457-4.
McCloskey, L., Bernstein, J., Winter, M., Iverson, R., & Lee-Parritz, A. (2014). Follow-up of gestational diabetes mellitus in an urban safety net hospital: Missed opportunities to launch preventive care for women. Journal of Women’s Health, 23, 327–334. doi:10.1089/jwh.2013.4628.
McIntyre, H. D., Peacock, A., Miller, Y. D., Koh, D., & Marshall, A. L. (2012). Pilot study of an individualised early postpartum intervention to increase physical activity in women with previous gestational diabetes mellitus. International Journal of Endocrinology, 2012, 892019. doi:10.1155/2012/892019.
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & PRISMA Group. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Journal of Clinical Epidemiology, 62, 1006–1012. doi:10.1016/j.jclinepi.2009.06.005.
Morton, S., Kirkwood, S., & Thangaratinam, S. (2014). Interventions to modify the progression to type 2 diabetes mellitus in women with gestational diabetes: A systematic review of literature. Current Opinion in Obstetrics and Gynecology, 26, 476–486. doi:10.1097/GCO.0000000000000127.
Nicklas, J. M., Seely, E. W., Zera, C. A., Abdul-Rahim, Z. S., Rudloff, N. D., & Levkoff, S. E. (2011). Identifying postpartum intervention approaches to prevent type 2 diabetes in women with a history of gestational diabetes. BMC Pregnancy and Childbirth. doi:10.1186/1471-2393-11-23.
Nicklas, J. M., Zera, C. A., England, L. J., Rosner, B. A., Horton, E., Levkoff, S. E., et al. (2014). A web-based lifestyle intervention for women with recent gestational diabetes mellitus: A randomized controlled trial. Obstetrics and Gynecology, 124, 563–570. doi:10.1097/AOG.0000000000000420.
Peacock, A. S., Bogossian, F. E., Wilkinson, S. A., Gibbons, K. S., Kim, C., & McIntyre, H. D. (2015). A randomised controlled trial to delay or prevent type 2 diabetes after gestational diabetes: Walking for exercise and nutrition to prevent diabetes for you. International Journal of Endocrinology, 2015, 423717. doi:10.1155/2015/423717.
Prochaska, J. O., & Velicer, W. F. (1997). The transtheoretical model of health behavior change. American Journal of Health Promotion, 12, 38–48.
Ratner, R. E., Christophi, C. A., Metzger, B. E., Dabelea, D., Bennett, P. H., Pi-Sunyer, X., et al. (2008). Prevention of diabetes in women with a history of gestational diabetes: Effects of metformin and lifestyle interventions. Journal of Clinical Endocrinology and Metabolism, 93, 4774–4779. doi:10.1210/jc.2008-0772.
Razee, H., van der Ploeg, H. P., Blignault, I., Smith, B. J., Bauman, A. E., McLean, M., et al. (2010). Beliefs, barriers, social support, and environmental influences related to diabetes risk behaviours among women with a history of gestational diabetes. Health Promotion Journal of Australia, 21, 130–137.
Reinhardt, J. A., van der Ploeg, H. P., Grzegrzulka, R., & Timperley, J. G. (2012). Implementing lifestyle change through phone-based motivational interviewing in rural-based women with previous gestational diabetes mellitus. Health Promotion Journal of Australia, 23, 5–9.
Smith, B. J., Cinnadaio, N., Cheung, N. W., Bauman, A., Tapsell, L. C., & van der Ploeg, H. P. (2014). Investigation of a lifestyle change strategy for high-risk women with a history of gestational diabetes. Diabetes Research and Clinical Practice, 106, e60–e63. doi:10.1016/j.diabres.2014.09.035.
Acknowledgments
Dr. Emily J. Jones is a 2014 Robert Wood Johnson Foundation Nurse Faculty Scholar and recognizes the Foundation’s support of this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jones, E.J., Fraley, H.E. & Mazzawi, J. Appreciating Recent Motherhood and Culture: A Systematic Review of Multimodal Postpartum Lifestyle Interventions to Reduce Diabetes Risk in Women with Prior Gestational Diabetes. Matern Child Health J 21, 45–57 (2017). https://doi.org/10.1007/s10995-016-2092-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-016-2092-z