Abstract
Purpose
To evaluate the incidence of and factors associated with intraoperative floppy iris syndrome (IFIS) in patients undergoing cataract phacoemulsification.
Methods
In total, 319 eyes of 319 patients who underwent phacoemulsification with implantation of an intraocular lens (IOL) into the posterior chamber were included in this study. Direct injection of epinephrine into the anterior chamber was performed in all cases. The following patient information was collected: gender, age, axial length of the eye, presence of pseudoexfoliation syndrome, glaucoma, diabetes mellitus, hypertension, current use of medications including alpha1 adrenergic receptor antagonists (alpha1-ARAs), finasteride, and benzodiazepines, duration of intake of alpha1-ARAs and finasteride, and duration of the surgery. Patients were classified as IFIS or non-IFIS after the surgery. Univariate and multivariate logistic regression analyses were performed.
Results
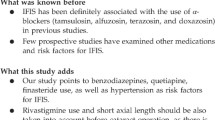
The overall incidence of IFIS was 9.09% (29/319 eyes). The multivariate analysis revealed that tamsulosin use (P = 0.004), finasteride use (P = 0.014), and increasing age (P = 0.006) were significantly associated with IFIS. Male gender and benzodiazepine use were significantly associated with IFIS in the univariate analysis, but not in the multivariate analysis. The non-selective alpha1-ARA doxazosin was not found to be associated with IFIS.
Conclusions
The findings suggest that finasteride use and aging are risk factors for IFIS and confirm the association of tamsulosin use with IFIS. Further, doxazosin appears to be a relatively safe drug with respect to the occurrence of IFIS.
Similar content being viewed by others
Introduction
Intraoperative floppy iris syndrome (IFIS) was first described by Chang and Campbell [1] as a triad of intraoperative signs during cataract surgery: flaccid iris stroma leading to billowing of the iris, iris prolapse through surgical wounds, and progressive intraoperative miosis.
They also defined three grades of IFIS depending on the number of signs observed during surgery: grade 1, one of the three signs; grade 2, two signs; and grade 3 (full IFIS), all three signs. Further, they reported that IFIS was caused by tamsulosin, a selective alpha1A adrenergic receptor antagonist (alpha1A-ARA), which is prescribed for benign prostatic hyperplasia (BPH). Tamsulosin blocks prostatic alpha1A adrenergic receptors (alpha1A-AR) thereby reduce bladder outfall obstruction by relaxing the prostatic smooth muscle tissue encircling the urethra. Tamsulosin may also selectively block alpha1A-ARs in the iris dilator muscle, inhibiting mydriasis during surgery, which can be a concern for ophthalmologists. Since 2005, the relationship between IFIS and non-selective alpha1-ARAs, hypertension, and male sex has been also reported [1,2,3]. An association between IFIS and other medications such as finasteride, mianserin, rivastigmine, antipsychotic drugs, and benzodiazepines has also been described [3,4,5].
Finasteride is recommended in combination with alpha1-ARA, particularly with tamsulosin, in the therapy of moderate-to-severe BPH with a risk of progression [6]. The influence of finasteride use in both monotherapy and combined therapy on the development of IFIS is still unclear. The overall prevalence of IFIS in the study by Chang and Campbell was 2%, but later studies found an even higher incidence, reaching up to 12.6% [2, 3, 7,8,9,10]. The occurrence of IFIS during cataract surgery may induce intraoperative complications including posterior capsule rupture, capsulorhexis tear, iris trauma, zonular dialysis, vitreous prolapse, and corneal edema, and thereby the identification of the risk factors for IFIS is particularly important for surgeons [9].
In light of the above, the aim of our prospective study was to investigate the incidence of IFIS during routine phacoemulsification and to determine the factors associated with IFIS. We focused particularly on the relationship between IFIS and finasteride use adjusted by the influence of other variables.
Patients and methods
This prospective study was conducted from February to October 2016 at the Department of Ophthalmology of the Military Institute of Aviation Medicine in Warsaw, Poland. In total, 319 eyes of 319 Caucasian patients undergoing cataract phacoemulsification with implantation of an intraocular lens (IOL) into the posterior chamber were consecutively included. The exclusion criteria were as follows: previous ocular surgery, previous trauma of the eye, undergoing combined ophthalmic surgery (e.g., cataract surgery and trabeculectomy or vitrectomy), peripheral anterior or posterior synechiae, iridodonesis, chronic uveitis, and proliferative diabetic retinopathy. All cataract surgeries in the study were performed by the same four surgeons. If a patient underwent an operation on both eyes during the study period, only the data of the first cataract surgery were included in the analysis. The following data were collected: occurrence and grade of IFIS during the surgery, gender, age, axial length of the eye, presence of pseudoexfoliation syndrome, glaucoma, medical comorbidities (diabetes mellitus and hypertension), and current use of medications (for at least one month) including alpha1 ARAs, finasteride, and benzodiazepines. The total duration of alpha1 ARA and finasteride intake was also noted. IOL calculations were performed preoperatively with the use of the IOLMaster 500 optical biometer (Carl Zeiss Meditec AG, Jena, Germany). The preoperative data were collected by the resident physician. After the surgery, the surgeon reported the occurrence and grade of IFIS, according to the recommendations of Chang and Campbell [1]. Surgeons were blinded preoperatively to the medications the patients were taking. The study protocol adhered to the tenets of the Declaration of Helsinki. All patients provided informed consent for participation in the study.
Topical antibiotics and oral acetazolamide were administered to all patients preoperatively. All procedures were performed under topical anesthesia using 0.5% proxymetacaine eye drops and an intracameral injection of 2% lidocaine. Preoperatively, the pupil was dilated with 10% phenylephrine and 1% tropicamide eye drops. During the operation, 0.03% epinephrine was injected directly into the anterior chamber after the intracameral administration of 2% lidocaine. Epinephrine was omitted from the irrigation bottle.
All surgeons used a standardized technique of cataract surgery, that in summary included the creation of a 2.6-mm clear corneal incision, capsulorhexis, phacoemulsification, cortex removal using a bimanual irrigation/aspiration tip, and posterior chamber foldable IOL implantation. Viscoelastic material (sodium hyaluronate 1%) was injected into the anterior chamber and behind the iris plane. An acrylic foldable IOL (Acrysof Natural Single-Piece SA60AT, Alcon) was implanted in all eyes. Phacoemulsification was performed using the Alcon Infinity Phaco Machine (Alcon, TX, USA).
Statistical analysis
All collected data were tabulated in a Microsoft Excel database (Microsoft Corporation, Redmond, Washington). All statistical analyses were performed using the Statistica version 13.1 PL software (Statsoft, Tulsa, Oklahoma). The categorical variables were compared using the Fisher exact test, and continuous variables were compared using the Mann–Whitney U test. The relationship between IFIS and the various risk factors was explored using univariate and multivariate logistic regression analysis. For the regression analyses, IFIS was considered a dichotomous variable (1 = IFIS, 0 = no IFIS). The multivariate logistic regression analysis was carried out using factors from the univariate analysis that reached statistical significance, defined as P < 0.05. The corresponding odds ratios (OR) and 95% confidence intervals (CI) were calculated to identify the risk factors for IFIS.
Results
The study involved 319 eyes of 319 patients who underwent cataract surgery during the study period (144 males and 175 females, mean age 76.06 ± 8.37 years, range 54 to 96 years). The study group included 200 hypertensives (62.70%), 83 diabetics (26.02%), 52 patients (16.30%) with glaucoma, 13 patients (4.08%) with pseudoexfoliation syndrome, 18 patients (5.64%) on tamsulosin, 24 (7.52%) on doxazosin, and 24 patients using finasteride (7.52%). Benzodiazepines were being taken in 5 (1.57%) cases. Antidepressants (tianeptine) and antipsychotic drugs (levomepromazine) were being taken in one case each (0.31%).
IFIS was noted in 29/319 eyes (9.09%). The IFIS prevalence in male patients was 13.69% (20/144 eyes), compared to 5.14% (9/175 eyes) in female patients. The IFIS grades were: grade 1 in 13 eyes (44.83%), grade 2 in 11 eyes (37.93%), and grade 3 in 5 eyes (17.24%). There was no significant difference in the prevalence of the syndrome between the four surgeons (P = 0.67).
Table 1 illustrates the demographics and clinical data in both the IFIS and non-IFIS groups. Male gender, tamsulosin use, finasteride use, and an older age were found to be significantly associated with IFIS. No significant associations were observed in regard to hypertension, diabetes mellitus, glaucoma, pseudoexfoliation syndrome, axial length, doxazosin use, and benzodiazepine use.
The duration of tamsulosin, doxazosin, and finasteride intake was not significantly associated with IFIS incidence. Among the patients taking tamsulosin, the mean duration of intake was 5.63 ± 6.07 years (range 1–20 years) for IFIS patients, compared to 3.70 ± 2.06 years (range 1–8 years) for non-IFIS patients (P = 0.63). Similarly, the mean duration of doxazosin intake was 5.25 ± 2.22 years (range 3–8 years) in the IFIS group and 6.35 ± 5.89 years (range 1–20 years) in the non-IFIS group (P = 0.68); and the mean duration of finasteride intake was 4.44 ± 2.40 years (range 2–8 years) for patients with IFIS, and 6.83 ± 4.73 years (range 1–18 years) for patients without (P = 0.24).
A total of 21/319 (6.58%) patients were receiving combined therapy (4.48% in the non-IFIS group vs. 27.59% in the IFIS group) consisting of alpha1-ARA (tamsulosin or doxazosin) with finasteride. The prevalence of IFIS was 30.77% (4/13) among the patients using doxazosin with finasteride, and there were no cases of IFIS among the 11 patients on doxazosin alone (without finasteride). The incidence of IFIS was 50% (4/8) among the patients using tamsulosin with finasteride, and 40% (4/10) among the patients using tamsulosin alone. Among patients with 1st, 2nd, and 3rd grade IFIS, the percentage of those who were receiving combined therapy was, respectively, 7.69% (1/13), 36.36% (4/11), and 60% (3/5). Unfortunately, these subgroups were too small to perform any meaningful statistical analysis.
The univariate analysis found that male sex, age (an increase of 1 year), current tamsulosin use, benzodiazepine use, and finasteride use were significantly associated with IFIS (P < 0.05 for each variable). No significant association was found for hypertension, diabetes mellitus, glaucoma, pseudoexfoliation syndrome, doxazosin use, and axial length of the eye. Tables 2 and 3 present, respectively, the results of the univariate and multivariate logistic regression analysis for the risk factors associated with IFIS. In the multivariate model logistic regression, only three factors were found to be significantly associated with IFIS: age, tamsulosin use, and finasteride use (P < 0.05 for each variable). A significant prolongation of the surgical time was observed in the IFIS group compared to the non-IFIS group (mean operative time 20.07 ± 08.31 vs. 16.13 ± 5.44 min; P = 0.004).
There were 21 eyes with IFIS (72.74%) that had not been exposed to tamsulosin. The mean age in this group was 79.81 ± 6.43 years (range 68–90 years). Statistical analysis of this subgroup revealed that the only significant risk factor for IFIS among these patients was finasteride use, with an adjusted OR of 7.64 (P = 0.001).
Discussion
In the initial report of intraoperative floppy iris syndrome, Chang and Campbell speculated on the association between IFIS and tamsulosin use [1], which was confirmed in several following publications [2, 4, 9,10,11,12]. According to the current literature, the incidence of IFIS is highly variable, and ranges from 0.8 to 12.6% [1,2,3, 8,9,10,11,12,13]. Lim et al. [13] reported a lower incidence of IFIS in Asian populations compared with Western populations and suggested that the difference might be attributed to the darker iris color in Korean patients. In our study, we found a 9.09% incidence of IFIS, which is lower than that found in a recent large study by Wahl et al. [8], who reported a 12.6% prevalence of IFIS among 947 patients undergoing cataract surgery, and in another study by Vollman et al. [9], who reported an incidence of 11.5% among 4923 cataract surgery cases. Further, Shah et al. [14] described the billowing and flaccid nature of the iris, as well as iris prolapse through the corneal section during phacoemulsification, in patients taking tamsulosin only two days before the day of surgery; the lower IFIS incidence in the present study might be reduced, because only patients who had taken medication for at least one month were arbitrarily considered. Compared to the earliest reports of IFIS, there appears to be an increasing prevalence of IFIS among more recent studies [1, 10, 11]. The reasons for this trend may be an increased prescription rate of the medications associated with IFIS, and a greater awareness of surgeons regarding the syndrome.
There are three subtypes of alpha1 adrenergic receptors, namely alpha1A, alpha1B, and alpha1D receptors [15]. Tamsulosin selectively blocks alpha1A-ARs, while terazosin, doxazosin, and alfuzosin have varying affinities for the aforementioned alpha1-AR subtypes. Previous animal studies found that apha1A-ARs are the most common subtype in the iris dilator muscle [16, 17]. The blockage of alpha1A-ARs by tamsulosin in the iris dilator muscle leads to poor muscle tone, and flaccid and floppy iris stroma, thus impeding of the dilatation of the pupil. Additionally, in vitro rabbit studies revealed that tamsulosin binds to melanin in the iris, causing atrophy of the dilator muscle, which could be a second mechanism leading to IFIS [18]. Alpha1A-ARs are also the most widespread adrenergic receptors in the arterioles of the iris, but a previous study using iris fluorescein angiography and anterior segment optical coherence tomography (AS-OCT) did not find evidence that tamsulosin use may lead to dysregulation of the iris vessels [19].
According to the current literature, the prevalence of IFIS during cataract surgery among patients taking tamsulosin (current or past) ranges from 40.4 to 86.4% [1, 10,11,12, 20, 21]. However, in Korean patients, Lim et al. [13] reported IFIS in only 3 out of 15 patients (20%) who had a history of tamsulosin use. In the present study, 40% (4/10 cases) of patients taking exclusively tamsulosin developed IFIS. The adjusted odds ratios (OR) in our paper indicate that the chance of developing IFIS during phacoemulsification with an intraoperative injection of epinephrine into the anterior chamber was 5.78 times greater among patients taking tamsulosin comparing to those who were not. In light of these results, physicians should pay attention to current guidelines on IFIS of the American Society of Cataract and Refractive Surgery (ASCRS) and the American Academy of Ophthalmology (AAO), which recommend scheduling cataract surgery prior to initiating tamsulosin, or using non-selective alpha1-ARAs for BPH treatment [22].
Although a relationship between IFIS and non-selective alpha1-ARAs, including doxazosin, alfuzosin, and terazosin, has been reported in several papers, the exact nature of their interaction is not quite clear [2, 8, 10, 11, 13, 20]. Most of the studies analyzing the OR for non-selective alpha1-ARAs make comparisons with alfuzosin or terazosin use, whereas the OR for doxazosin use in the current literature is poorly explored [2, 23]. In a meta-analysis concerning IFIS, alfuzosin and terazosin use had comparable ORs in the standard dichotomous analysis, whereas current doxazosin use did not obtain statistical significance using a dichotomous doxazosin/no-doxazosin approach [23]. The effect of doxazosin reached statistical significance in an alternative analysis (vs. patients not receiving any alpha1-ARAs), OR 24.2; 95% CI 1.7–351.7) [23]. In the present study, we did not find any significant association between doxazosin use and IFIS. The possible reason of this result can be the mechanism of activity of doxazosin. It based on the non-selective inhibition of the binding of norepinephrine to the all known alpha1-AR subtypes (alpha1A, alpha1B, and alpha1D receptors), in opposite to tamsulosin that blocks selectively alpha1A-ARs. In the light of this differences, we believe that the influence of doxazosin on alpha1A-ARs is probably weaker compared with tamsulosin. We did not execute the alternative analysis for doxazosin use (vs. patients not receiving any alpha1-ARAs) because of the scanty amount of cases.
Similar to other results [2, 4, 10], we found no correlation between the risk of IFIS and each of the following morbidities: diabetes mellitus, glaucoma, and pseudoexfoliation syndrome. However, there are some controversies occurring regarding the relationship between IFIS and high blood pressure. Schwinn and Afshari [24] suggested that the resistance of the relaxed iris dilator muscle to adrenergic agonists may be associated with endothelial dysregulation, which exists in systemic diseases like congestive heart failure, diabetes mellitus, and hypertension; however, the association of systemic high blood pressure with IFIS is unclear. Altan-Yaycioglu et al. [11] did not find any correlation between complete IFIS and hypertension among 500 patients who underwent phacoemulsification surgery. Chatziralli and Sergentanis [23] reported in a meta-analysis the positive association between IFIS and hypertension. However, the same author described 1 year later no significant influence of hypertension on the development of IFIS in a study of 738 eyes [2]. Similarly, in the present study we did not observe a correlation between hypertension and IFIS using logistic regression analysis.
In the initial study concerning IFIS, Chang and Campbell noted the development of the syndrome solely among men [1]. In 2016, Wahl et al. [8] found a gender distribution within IFIS patients of 57.1% male and 42.9% female. In the current study, 31.01% (9 eyes) of all IFIS cases occurred in female patients. The mean age among the women afflicted with IFIS was 80.56 ± 6.42 years (range 72–90 years). Among them, 66.67% had hypertension, whereas both glaucoma and pseudoexfoliation syndrome were noted in only two cases each (there was no female patients with both glaucoma and pseudoexfoliation syndrome). None of the women in the IFIS group were taking alpha1-ARAs, benzodiazepines, or antipsychotic drugs. This may be associated with prescribing other, uncharted drugs that may cause IFIS. The prescription rate of these drugs could have increased over the past years, causing the increase in IFIS incidence among women. In our study, male gender was significantly associated with IFIS in the univariate analysis, but not in the multivariate analysis. Similar results have been published in large prospective studies [2, 4]. However, Neff et al. [10] described male gender as a statistically significant risk factor for developing IFIS with a calculated OR of 4.7 using multivariate analysis.
Finasteride is a synthetic 4-azasteroid compound that is a specific inhibitor of steroid type II 5α-reductase, which is an intracellular enzyme that converts the androgen testosterone into 5α-dihydrotestosterone. The indications for finasteride include BPH and male pattern hair loss. In 2007, Issa and Dagres [6] first reported the possible association of IFIS during cataract surgery with finasteride use. Wong and Mak [25] described the likely influence of finasteride intake on both the occurrence of IFIS and cataract. In an experimental study on rabbits, Horvath et al. [26] observed an increased risk of iris billowing during some phacoemulsification maneuvers subjects treated with finasteride was similar with those obtained in rabbits treated with tamsulosin. To the best of our knowledge, there are only two large prospective studies in the literature investigating the association between IFIS and finasteride use [4, 8]. In our prospective study, the adjusted OR for finasteride use was 3.94 (95% CI 1.32–11.79; P = 0.014). Combined therapy consisting of alpha1-ARA and finasteride is recommended in cases of moderate-to-severe lower urinary tract symptoms and enlarged prostate (> 40 mL), which includes BPH [7]. Considering these recommendations, it is worth emphasizing that in our study the prevalence of IFIS among patients receiving combined therapy consisting of tamsulosin and finasteride was higher compared to those receiving tamsulosin alone (50 vs. 40%). Further, the incidence of the syndrome within patients receiving combined therapy including doxazosin and finasteride was lower compared with those receiving tamsulosin alone (30.77 vs. 40%). In present study, the duration of intake of tamsulosin, doxazosin, and finasteride did not differ between the IFIS and non-IFIS groups, which confirms the results of previous studies [4, 20].
Takayanagi [27] suggested that, in the iris dilator muscles, the potency of norepinephrine, which alters with aging, is proportional to the receptor reserve. They surmised that this is the mechanism underpinning the relationship between aging and the sensitivity of the iris to adrenergic antagonists. Using immunohistochemical analysis, Panagis et al. [28] confirmed the localization of alpha1A-ARs to the human iris arteriolar muscularis in addition to the iris dilator muscle, which suggests that IFIS may develop as a consequence of iris vascular dysfunction. Satoh et al. [29] investigated the incidence of leakage of fluorescein from the iris depending on the patient’s age. The fluorescein leakage in the pupillary margin was more frequent patients over 50 years than those under 50 years (48 vs. 3%), which suggests a link between iris vasculature dysfunction and aging. With these results in mind, the interesting result of our study is the increase in IFIS risk associated with aging: the adjusted OR for each 1-year increase in age was 1.09 (95% CI 1.03–1.16; P = 0.006). Wahl et al. [8] also reported a slight tendency for older patients to have more severe IFIS, but no statistical significance could be found.
Despite previous reports of the relationship between benzodiazepine use and the occurrence of IFIS, the exact nature of their interaction remains to be clarified [3, 4]. In the present study, the univariate analysis found a significant association between benzodiazepine use and IFIS, but the number of patients taking benzodiazepine in our study was small. Only one patient in the present study was taking an antipsychotic drug (levomepromazine). Although she was receiving treatment for hypertension and diabetes mellitus, she did not develop IFIS. An antidepressant (tianeptine) was being taken by one patient who also had hypertension, and IFIS was observed in this woman. Unlike the findings of a recent prospective study by Chatziralli et al. [4], which reported a significant relationship between short axial length and IFIS, we found no significant difference in the axial length of eyes between patients in the IFIS and non-IFIS groups.
The present study also compared the average surgical duration of phacoemulsification between patients in the IFIS and non-IFIS groups. To our knowledge, this has been studied in only one previous paper [2]. In the current study, the mean duration of the surgery in the IFIS group was 20.07 ± 8.31 min (range 10–50 min), and 16.13 ± 5.44 min (range 8–40 min) in the non-IFIS group; the difference was statistically significant (P = 0.004). The prolongation of the surgical time reflects the common view of most eye surgeons that IFIS increases the difficulty of the surgery [30]. Among patients with IFIS, we encountered one case of anterior capsular tear and no episodes of posterior capsule rupture (PCR) or vitreous loss. Similar results were seen in the literature, with no cases of PCR or vitreous loss [2, 10].
The limitations of our study include the limited number of cases and small number of events per variable. Using the recommendations of Peduzzi et al. [31] concerning logistic regression analysis and the 29 cases of IFIS in our dataset, the model was limited to three variables of interest.
In summary, our study confirms the association of tamsulosin use with IFIS and additionally indicates an increased risk of IFIS related to finasteride use and aging. There were no cases of IFIS among patients taking doxazosin alone, suggesting that doxazosin could be a relatively safe drug in the context of IFIS for patients expecting cataract surgery. The relatively high prevalence of IFIS in our study may reflect both the increasing diagnosis of IFIS by surgeons, and the association of IFIS with drugs other than alpha1-ARAs, which have been increasingly prescribed in recent years.
The combination of iris physiology and condition, variable medication use, individual susceptibility to drugs, coexisting ocular and systemic diseases, and other demographic factors likely all play a role in the incidence IFIS. Future studies should investigate how these factors affect both the incidence and the severity of IFIS, as well as the effects of combination therapies (e.g., tamsulosin and finasteride) on IFIS incidence. In addition, because IFIS has been observed in women who are not receiving alpha1-ARAs, there might be other underlying mechanisms that need to be clarified. This information would support the prediction of possible intraoperative complications and surgical outcomes. Additionally, as suggested by Chang et al. [30], there is a need to educate urologists and primary care physicians about IFIS.
References
Chang DF, Campbell JR (2005) Intraoperative floppy iris syndrome associated with tamsulosin. J Cataract Refract Surg 31(4):664–673. https://doi.org/10.1016/j.jcrs.2005.02.027
Goyal S, Dalela D, Goyal NK et al (2014) Intraoperative floppy iris syndrome in Indian population: a prospective study on incidence, risk factors, and impact on operative performance. Indian J Ophthalmol 62(8):870–875. https://doi.org/10.4103/0301-4738.141051
Chatziralli IP, Sergentanis TN, Papazisis L, Moschos MM (2012) Risk factors for intraoperative floppy iris syndrome: a retrospective study. Acta Ophthalmol 90(2):e152–e153. https://doi.org/10.1111/j.1755-3768.2011.02132.x
Chatziralli IP, Peponis V, Parikakis E, Maniatea A, Patsea E, Mitropoulos P (2016) Risk factors for intraoperative floppy iris syndrome: a prospective study. Eye 30(8):152–153. https://doi.org/10.1038/eye.2016.122
Matsuo M, Sano I, Ikeda Y, Fujihara E, Tanito M (2016) Intraoperative floppy-iris syndrome associated with use of antipsychotic drugs. Can J Ophthalmol 51(4):294–296. https://doi.org/10.1016/j.jcjo.2016.02.008
Issa SA, Dagres E (2007) Intraoperative floppy-iris syndrome and finasteride intake. J Cataract Refract Surg 33(12):2142–2143. https://doi.org/10.1016/j.jcrs.2007.07.025
Gravas S, Bach T, Bachmann A et al (2016) EAU guidelines on management of non neurogenic male LUTS. Eur Assoc Urol Guidel 21–23
Wahl M, Tipotsch-Maca SM, Vecsei-Marlovits PV (2016) Intraoperative floppy iris syndrome and its association with various concurrent medications, bulbus length, patient age and gender. Graefe’s Arch Clin Exp Ophthalmol. https://doi.org/10.1007/s00417-016-3515-7
Vollman DE, Gonzalez-Gonzalez LA, Chomsky A, Daly MK, Baze E, Lawrence MG (2014) Intra-operative floppy iris and prevalence of intra-operative complications: results from Ophthalmic Surgery Outcomes Database. Am J Ophthalmol 158(4):847–848. https://doi.org/10.1016/j.ajo.2014.06.027
Neff KD, Sandoval HP, Fernández de Castro LE, Nowacki AS, Vroman DT, Solomon KD (2009) Factors associated with intraoperative floppy iris syndrome. Ophthalmology 116(4):658–663. https://doi.org/10.1016/j.ophtha.2008.12.026
Altan-Yaycioglu R, Gedik S, Pelit A, Akova YA, Akman A (2009) Clinical factors associated with floppy iris signs: a prospective study from two centers. Ophthalmic Surg Lasers Imaging 40(3):232–238. https://doi.org/10.9999/15428877-20090430-02
Altiaylik Ozer P, Altiparmak UE, Unlu N, Hazirolan DO, Kasim R, Duman S (2013) Intraoperative floppy-iris syndrome: comparison of tamsulosin and drugs other than alpha antagonists. Curr Eye Res 38(4):480–486. https://doi.org/10.3109/02713683.2013.763986
Lim DH, Lee MG, Chung T-Y, Chung E-S (2014) Korean patients taking alpha1-adrenergic receptor antagonists show lower incidence of intraoperative floppy iris syndrome than western patients. Br J Ophthalmol 98(4):479–483. https://doi.org/10.1136/bjophthalmol-2013-304135
Shah N, Tendulkar M, Brown R (2009) Should we anticipate intraoperative floppy iris syndrome (IFIS) even with very short history of tamsulosin? Eye 23(3):740. https://doi.org/10.1038/Eye.2008.95
Hieble JP, Bylund DB, Clarke DE et al (1990) International Union of Pharmocology X. Recommendation for nomenclature of a1-adrenoceptors: consensus update. Pharmacol Rev 47(2):297–314
Yu Y, Koss MC (2003) Studies of alpha-adrenoceptor antagonists on sympathetic mydriasis in rabbits. J Ocul Pharmacol Ther 19(3):255–263. https://doi.org/10.1089/108076803321908374
Yu Y, Koss MC (2003) Functional characterization of alpha-adrenoceptors mediating pupillary dilation in rats. Eur J Pharmacol 471(2):135–140
Goseki T, Ishikawa H, Ogasawara S et al (2012) Effects of tamsulosin and silodosin on isolated albino and pigmented rabbit iris dilators: possible mechanism of intraoperative floppy-iris syn- drome. J Cataract Refract Surg 38:1643–1649. https://doi.org/10.1016/j.jcrs.2012.05.025
Shtein RM, Hussain MT, Cooney TM, Elner VM, Hood CT (2014) Effect of tamsulosin on iris vasculature and morphology. J Cataract Refract Surg 40(5):793–798. https://doi.org/10.1016/j.jcrs.2013.10.031
Chang DF, Campbell JR, Colin J, Schweitzer C (2014) Prospective masked comparison of intraoperative floppy iris syndrome severity with tamsulosin versus alfuzosin. Ophthalmology 121(4):829–834. https://doi.org/10.1016/j.ophtha.2013.10.031
Blouin M, Blouin J, Perreault S, Lapointe A, Dragomir A (2007) Intraoperative floppy-iris syndrome associated with alpha1-adrenoreceptors: comparison of tamsulosin and alfuzosin. J Cataract Refract Surg 33(7):1227–1234. https://doi.org/10.1016/j.jcrs.2007.03.032
Intraoperative Floppy Iris Syndrome (IFIS) Associated with Systemic Alpha-1 Antagonists (2014) ASCRS and AAO Educational Update Statement, ASCRS and AAO Quality of Care Secretariat, Hoskins Center for Quality Eye Care
Chatziralli IP, Sergentanis TN (2011) Risk factors for intraoperative floppy Iris syndrome: a meta-analysis. Ophthalmology 118(4):730–735. https://doi.org/10.1016/j.ophtha.2010.08.039
Schwinn DA, Afshari NA (2006) α1-adrenergic receptor antagonists and the iris: new mechanistic insights into floppy iris syndrome. Surv Ophthalmol 51(5):501–512. https://doi.org/10.1016/j.survophthal.2006.06.011
Wong ACM, Mak ST (2011) Finasteride-associated cataract and intraoperative floppy-iris syndrome. J Cataract Refract Surg 37(7):1351–1354. https://doi.org/10.1016/j.jcrs.2011.04.013
Horvath K, Vultur F, Simon V, Voidazan S, Gh M (2015) Research on intraoperative iris behavior in rabbits treated with tamsulosin and finasteride. Hippokratia 19(1):20–24
Takayanagi I (1994) Effects of aging on drug receptor mechanisms in smooth muscles. Nihon Yakurigaku Zasshi. Folia Pharmacol Jpn 104(3):163–175
Panagis L, Basile M, Friedman AH, Danias J (2010) Intraoperative floppy iris syndrome: report of a case and histopathologic analysis. Arch Ophthalmol 128(11):1437–1441
Satoh K, Takaku Y, Ohtsuki K, Mizuno K (1999) Effects of aging on fluorescein leakage in the iris and angle in normal subjects. Jpn J Ophthalmol 43(3):166–170
Chang DF, Braga-Mele R, Mamalis N et al (2008) Clinical experience with intraoperative floppy-iris syndrome. Results of the 2008 ASCRS member survey. J Cataract Refract Surg 34(7):1201–1209. https://doi.org/10.1016/j.jcrs.2008.04.014
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR (1996) A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 49(12):1373–1379
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Kaczmarek, I.A., Prost, M.E. & Wasyluk, J. Clinical risk factors associated with intraoperative floppy iris syndrome: a prospective study. Int Ophthalmol 39, 541–549 (2019). https://doi.org/10.1007/s10792-018-0840-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-018-0840-3