Abstract
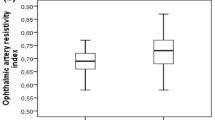
Purpose The evaluation of orbital blood flow parameters in patients with unilateral pseudoexfoliation syndrome (XFS) and in age–sex-matched control subjects using color Doppler imaging. Methods This prospective, comparative case series included 33 unilateral XFS patients and 33 age–sex-matched control subjects. Color Doppler imaging was used to evaluate the XFS-affected (Group 1) and -unaffected (Group 2) eyes that were matched with the corresponding side (Groups 3 and 4) of control subjects. All subjects were given a complete ophthalmological examination. A masked radiologist obtained the peak systolic velocity (PSV) and end diastolic velocity (EDV) of ophthalmic (OA), central retinal (CRA), nasal posterior ciliary (NPCA) and temporal posterior ciliary arteries (TPCA) as well as mean velocity of central retinal vein (CRV). Resistivity indices (RI) were calculated. Results Analysis of peak systolic and end diastolic velocity (PSV, EDV) and RI between Groups 1–2 and 3–4 did not show any significant difference. Comparing Groups 1–3 (corresponding eyes of pseudoexfoliation-affected and control subjects) and Groups 2–4 (corresponding eyes of pseudoexfoliation-unaffected and control subjects) revealed significantly low values for OA, PSV and EDV in both eyes of the XFS patients. The OA RI value in Group 1 was found to be significantly higher than that in Group 3 with the cut-off value of 0.72. Conclusion These findings suggest that ophthalmic artery hemodynamic parameters change in both eyes of unilateral XFS patients, illustrating out the systemic nature of the disease. We conclude that XFS decreases OA blood flow velocities and increases vascular resistance through progressive build-up.

Similar content being viewed by others
Abbreviations
- CRA:
-
Central retinal artery
- CRV:
-
Central retinal vein
- EDV:
-
End diastolic velocity
- OA:
-
Ophthalmic artery
- NPCA:
-
Nasal posterior ciliary artery
- PSV:
-
Peak systolic velocity
- RI:
-
Resistivity index
- TPCA:
-
Temporal posterior ciliary artery
- XFS:
-
Pseudoexfoliation syndrome
References
Ritch R (1994) The most common identifiable cause of open angle glaucoma. J Glaucoma 3:176–178
Schlotzer-Schrehardt U, Kuchle M, Hofmann-Rummelt C (2000) Latent TGF-beta 1 binding protein (LTBP-1); a new marker for intra- and extraocular PEX deposits. Klin Monatsbl Augenheilkd 216:412–419
Schlotzer-Schrehardt U, Kuchle M, Naumann GOH (1991) Electron-microscopic identification of pseudoexfoliation material in extrabulbar tissue. Arch Ophthalmol 109:565–570
Ritch R, Schlotzer-Schrehardt U (2001) Exfoliation syndrome. Surv Ophthalmol 45:265–315
Zoric L, Miric D, Milenkovic S, Jovanovic P, Trajkovic G (2006) Pseudoexfolition syndrome and its antioxidative protection deficiency as risk factors for age-related cataract. Eur J Ophthalmol 16:268–273
Mitchell P, Wang JJ, Hourihan F (1999) The relationship between glaucoma and pseudoexfoliation: the Blue Mountains Eye Study. Arch Ophthalmol 117:1319–1324
Puska PM (2002) Unilateral exfoliation syndrome: conversion to bilateral exfoliation and to glaucoma: a prospective 10-year follow-up study. J Glaucoma 11:517–524
Konstas AG, Stewart WC, Stroman GA, Sine CS (1997) Clinical presentation and initial treatment patterns in patients with exfoliation glaucoma versus primary open-angle glaucoma. Ophthal Surg Lasers 28:111–117
Shimizu T (1985) Changes of iris vessels in capsular glaucoma: three-dimensional and electron microscopic studies. Jpn J Ophthalmol 29:434–452
Repo LP, Terasvirta ME, Koivisto KJ (1993) Generalized transluminance of the iris and the frequency of the pseudoexfoliation syndrome in the eyes of transient ischemic attack patients. Ophthalmology 100:352–355
Hollo G, Lakatos P, Farkas K (1998) Cold pressor test and plasma endothelin-1 concentration in primary open-angle and capsular glaucoma. J Glaucoma 7:105–110
Repo LP, Suhonen MT, Terasvirta ME, Koivisto KJ (1995) Color Doppler imaging of the ophthalmic artery blood flow spectra of patients who have had a transient ischemic attack. Ophthalmology 102:1199–1205
Puska P, Vesti E, Tomita G, Ishida K, Raitta C (1999) Optic disc changes in normotensive persons with unilateral exfoliation syndrome: a 3-year follow-up study. Graefes Arch Clin Exp Ophthalmol 237:457–462
Saatçi OA, Ferliel ST, Ferliel M, Kaynak S, Ergin MH (1999) Pseudoexfoliation and glaucoma in eyes with retinal vein occlusion. Int Ophthalmol 23:75–78
Leske MC, Heijl A, Hussein M, et al. (2003) Factors for glaucoma progression and the effect of treatment: the early manifest glaucoma trial. Am J Ophthalmol 121:48–56
Shimizu K, Kimura Y, Aoki K (1988) Prevalence of exfoliation syndrome in the Japanese. Acta Ophthalmol 184[Suppl]:112–115
Medeiros FA, Sample PA, Weinreb RN (2003) Corneal thickness measurements and frequency doubling technology perimetry abnormalities in ocular hypertensive eyes. Ophthalmology 110:1903–1908
Yuksel N, Karabaş VL, Arslan A, Demirci A, Caglar Y (2001) Ocular hemodynamics in pseudoexfoliation syndrome and pseudoexfoliation glaucoma. Ophthalmology 108:1043–1049
Trible JR, Anderson DR (1998) Factors associated with retrobulbar hemodynamic measurements at variable intraocular pressure. J Glaucoma 7:33–38
Joos KM, Kay MD, Pillunat LE (1999) Effect of acute intraocular pressure changes on short posterior ciliary artery hemodynamics. Br J Ophthalmol 83:33–38
Trible JR, Sergott RC, Spaeth GL (1994) Trabeculectomy is associated with retrobulbar hemodynamic changes. A color Doppler analysis. Ophthalmology 101:340–351
Costa VP, Kuzniec S, Molnar LJ (1997) Clinical findings and hemodynamic changes associated with severe occlusive carotid artery disease. Ophthalmology 104:1994–2002
Greenfield DS, Heggerick PA, Hedges TR (1995) Color Doppler imaging of normal orbital vasculature. Ophthalmology 102:1598–1605
Williamson TH, Lowe GD, Baxter GM (1995) Influence of age, systemic blood pressure, smoking and blood viscosity on orbital velocities. Br J Ophthalmol 79:17–22
Meritt CRB (2005) Physics of ultrasound. In: Rumack CM, Wilson SR, Charboneau JW, Johnson JM (eds) Diagnostic ultrasound. Mosby Year Book, St Louis, pp 3–34
Kivela T, Hietanen J, Uusitalo M (1997) Autopsy analysis of clinically unilateral exfoliation syndrome. Invest Ophthalmol Vis Sci 38:2008–2015
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dayanir, V., Topaloğlu, A., Ozsunar, Y. et al. Orbital blood flow parameters in unilateral pseudoexfoliation syndrome. Int Ophthalmol 29, 27–32 (2009). https://doi.org/10.1007/s10792-008-9193-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-008-9193-7