Abstract
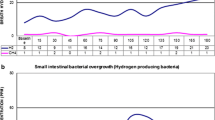
The increased availability of noninvasive breath tests, each with limitations, has led to widespread testing for small intestinal bacterial overgrowth (SIBO) in patients with non-specific gastrointestinal complaints. The lactulose breath test (LBT) is based upon an incorrect premise and therefore incorrect interpretations which has resulted in the over-diagnosis of SIBO and the excessive use of antibiotics in clinical practice. Despite limitations, the glucose breath test (GBT) should be exclusively employed when considering SIBO in appropriately chosen patients. This review suggests guidelines for the optimal use and appropriate interpretation of the GBT for suspected SIBO. The LBT should be discarded from future use, and the literature based upon the LBT should be discounted accordingly.

Similar content being viewed by others
References
Barker WH, Hummel LE. Macrocytic anemia in association with intestinal strictures and anastomoses. Bull Johns Hopkins Hosp. 1939;46:215–254.
Ellis H, Smith AD. The blind-loop syndrome. Monogr Surg Sci. 1967;4:193–215.
Corazza GR, Menozzi MG, Strocchi A, et al. The diagnosis of small bowel bacterial overgrowth. Reliability of jejunal culture and inadequacy of breath hydrogen testing. Gastroenterology. 1990;98:302–309. https://doi.org/10.1016/0016-5085(90)90818-l.
Pimentel M, Saad RJ, Long MD, Rao SSC. ACG clinical guideline: small intestinal bacterial overgrowth. Am J Gastroenterol. 2020;115:165–178. https://doi.org/10.14309/ajg.0000000000000501.
Posserud I, Stotzer PO, Bjornsson ES, Abrahamsson H, Simren M. Small intestinal bacterial overgrowth in patients with irritable bowel syndrome. Gut. 2007;56:802–808. https://doi.org/10.1136/gut.2006.108712.
Shah A, Talley NJ, Jones M, et al. Small intestinal bacterial overgrowth in irritable bowel syndrome: a systematic review and meta-analysis of case-control studies. Am J Gastroenterol. 2020;115:190–201. https://doi.org/10.14309/ajg.0000000000000504.
Tabaqchali S, Okubadejo OA, Neale G, Booth CC. Influence of abnormal bacterial flora on small intestinal function. Proc R Soc Med. 1966;59:1244–1246.
Saffouri GB, Shields-Cutler RR, Chen J, et al. Small intestinal microbial dysbiosis underlies symptoms associated with functional gastrointestinal disorders. Nat Commun. 2019;10:2012. https://doi.org/10.1038/s41467-019-09964-7.
Franco DL, Disbrow MB, Kahn A, et al. Duodenal Aspirates for small intestine bacterial overgrowth: yield, PPIs, and outcomes after treatment at a tertiary academic medical center. Gastroenterol Res Pract. 2015;2015:971582. https://doi.org/10.1155/2015/971582.
Berean KJ, Ha N, Ou JZ, et al. The safety and sensitivity of a telemetric capsule to monitor gastrointestinal hydrogen production in vivo in healthy subjects: a pilot trial comparison to concurrent breath analysis. Aliment Pharmacol Ther. 2018;48:646–654. https://doi.org/10.1111/apt.14923.
Levitt MD. Production and excretion of hydrogen gas in man. N Engl J Med. 1969;281:122–127. https://doi.org/10.1056/nejm196907172810303.
Dridi B, Henry M, El Khéchine A, Raoult D, Drancourt M. High prevalence of Methanobrevibacter smithii and Methanosphaera stadtmanae detected in the human gut using an improved DNA detection protocol. PLoS ONE. 2009;4:e7063. https://doi.org/10.1371/journal.pone.0007063.
Bjorneklett A, Jenssen E. Relationships between hydrogen (H2) and methane (CH4) production in man. Scand J Gastroenterol. 1982;17:985–992.
Keller J, Bassotti G, Clarke J, et al. Expert consensus document: advances in the diagnosis and classification of gastric and intestinal motility disorders. Nat Rev Gastroenterol Hepatol. 2018;15:291–308. https://doi.org/10.1038/nrgastro.2018.7.
Miller MA, Parkman HP, Urbain JL, et al. Comparison of scintigraphy and lactulose breath hydrogen test for assessment of orocecal transit: lactulose accelerates small bowel transit. Dig Dis Sci. 1997;42:10–18. https://doi.org/10.1023/a:1018864400566.
Rezaie A, Buresi M, Lembo A, et al. Hydrogen and methane-based breath testing in gastrointestinal disorders: The North American Consensus. Am J Gastroenterol. 2017;112:775–784. https://doi.org/10.1038/ajg.2017.46.
Yu D, Cheeseman F, Vanner S. Combined oro-caecal scintigraphy and lactulose hydrogen breath testing demonstrate that breath testing detects oro-caecal transit, not small intestinal bacterial overgrowth in patients with IBS. Gut. 2011;60:334–340.
Sellin JH. A breath of fresh air. Clin Gastroenterol Hepatol. 2016;14:209–211. https://doi.org/10.1016/j.cgh.2015.10.027.
Paterson W, Camilleri M, Simren M, Boeckxstaens G, Vanner SJ. Breath testing consensus guidelines for SIBO: RES IPSA LOCQUITOR. Am J Gastroenterol. 2017;112:1888–1889. https://doi.org/10.1038/ajg.2017.233.
Riordan SM, McIver CJ, Walker BM, Duncombe VM, Bolin TD, Thomas MC. The lactulose breath hydrogen test and small intestinal bacterial overgrowth. Am J Gastroenterol. 1996;91:1795–1803.
Simrén M, Stotzer PO. Use and abuse of hydrogen breath tests. Gut. 2006;55:297–303. https://doi.org/10.1136/gut.2005.075127.
Yao CK, Tuck CJ, Barrett JS, Canale KE, Philpott HL, Gibson PR. Poor reproducibility of breath hydrogen testing: Implications for its application in functional bowel disorders. Unit Eur Gastroenterol J. 2017;5:284–292. https://doi.org/10.1177/2050640616657978.
Brener W, Hendrix TR, McHugh PR. Regulation of the gastric emptying of glucose. Gastroenterology. 1983;85:76–82.
Gasbarrini A, Corazza GR, Gasbarrini G, et al. Methodology and indications of H2-breath testing in gastrointestinal diseases: the Rome Consensus Conference. Aliment Pharmacol Ther. 2009;29:1–49. https://doi.org/10.1111/j.1365-2036.2009.03951.x.
King CE, Toskes PP. Comparison of the 1-gram [14C]xylose, 10-gram lactulose-H2, and 80-gram glucose-H2 breath tests in patients with small intestine bacterial overgrowth. Gastroenterology. 1986;91:1447–1451. https://doi.org/10.1016/0016-5085(86)90199-x.
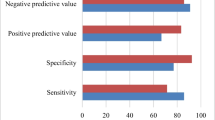
Erdogan A, Rao SS, Gulley D, Jacobs C, Lee YY, Badger C. Small intestinal bacterial overgrowth: duodenal aspiration vs glucose breath test. Neurogastroenterol Motil. 2015;27:481–489. https://doi.org/10.1111/nmo.12516.
Lin EC, Massey BT. Scintigraphy demonstrates high rate of false-positive results from glucose breath tests for small bowel bacterial overgrowth. Clin Gastroenterol Hepatol. 2016;14:203–208. https://doi.org/10.1016/j.cgh.2015.07.032.
Perman JA, Modler S, Engel RR, Heldt G. Effect of ventilation on breath hydrogen measurements. J Lab Clin Med. 1985;105:436–439.
Thompson DG, Binfield P, De Belder A, O’Brien J, Warren S, Wilson M. Extra intestinal influences on exhaled breath hydrogen measurements during the investigation of gastrointestinal disease. Gut. 1985;26:1349–1352. https://doi.org/10.1136/gut.26.12.1349.
Gilat T, Ben Hur H, Gelman-Malachi E, Terdiman R, Peled Y. Alterations of the colonic flora and their effect on the hydrogen breath test. Gut. 1978;19:602–605. https://doi.org/10.1136/gut.19.7.602.
Corazza G, Strocchi A, Sorge M, Bentai G, Gasbarrini G. Prevalence and consistency of low breath H2 excretion following lactulose ingestion. Possible implications for the clinical use of the H2 breath test. Dig Dis Sci.. 1993;38:2010–2016. https://doi.org/10.1007/bf01297077.
Corazza GR, Benati G, Strocchi A, Malservisi S, Gasbarrini G. The possible role of breath methane measurement in detecting carbohydrate malabsorption. J Lab Clin Med. 1994;124:695–700.
Montes RG, Saavedra JM, Perman JA. Relationship between methane production and breath hydrogen excretion in lactose-malabsorbing individuals. Dig Dis Sci. 1993;38:445–448. https://doi.org/10.1007/bf01316497.
Rana SV, Sinha SK, Sharma S, Kaur H, Bhasin DK, Singh K. Effect of predominant methanogenic flora on outcome of lactose hydrogen breath test in controls and irritable bowel syndrome patients of north India. Dig Dis Sci. 2009;54:1550–1554. https://doi.org/10.1007/s10620-008-0532-3.
Strocchi A, Corazza G, Ellis CJ, Gasbarrini G, Levitt MD. Detection of malabsorption of low doses of carbohydrate: accuracy of various breath H2 criteria. Gastroenterology. 1993;105:1404–1410. https://doi.org/10.1016/0016-5085(93)90145-3.
Tadesse K, Eastwood M. Breath-hydrogen test and smoking. Lancet. 1977;2:91. https://doi.org/10.1016/s0140-6736(77)90098-8.
Thompson DG, O’Brien JD, Hardie JM. Influence of the oropharyngeal microflora on the measurement of exhaled breath hydrogen. Gastroenterology. 1986;91:853–860. https://doi.org/10.1016/0016-5085(86)90686-4.
Mastropaolo G, Rees WD. Evaluation of the hydrogen breath test in man: definition and elimination of the early hydrogen peak. Gut. 1987;28:721–725. https://doi.org/10.1136/gut.28.6.721.
Anderson IH, Levine AS, Levitt MD. Incomplete absorption of the carbohydrate in all-purpose wheat flour. N Engl J Med. 1981;304:891–892. https://doi.org/10.1056/nejm198104093041507.
Erickson J, Wang Q, Slavin J. White grape juice elicits a lower breath hydrogen response compared with apple juice in healthy human subjects: a randomized controlled trial. J Acad Nutr Dietet. 2017;117:908–913. https://doi.org/10.1016/j.jand.2017.01.020.
Read NW, Al-Janabi MN, Bates TE, et al. Interpretation of the breath hydrogen profile obtained after ingesting a solid meal containing unabsorbable carbohydrate. Gut. 1985;26:834–842. https://doi.org/10.1136/gut.26.8.834.
Avallone EV, De Carolis A, Loizos P, Corrado C, Vernia P. Hydrogen breath test–diet and basal H2 excretion: a technical note. Digestion. 2010;82:39–41. https://doi.org/10.1159/000277630.
Bond JH, Jr., Levitt MD. Use of pulmonary hydrogen (H 2) measurements to quantitate carbohydrate absorption. Study of partially gastrectomized patients. J Clin Investig. 1972;51:1219-25. https://doi.org/10.1172/jci106916.
Sellin JH, Hart R. Glucose malabsorption associated with rapid intestinal transit. Am J Gastroenterol. 1992;87:584–589.
Iivonen MK, Ahola TO, Matikainen MJ. Bacterial overgrowth, intestinal transit, and nutrition after total gastrectomy. Comparison of a jejunal pouch with Roux-en-Y reconstruction in a prospective random study. Scand J Gastroenterol. 1998;33:63–70. https://doi.org/10.1080/00365529850166220.
Paik CN, Choi MG, Lim CH, et al. The role of small intestinal bacterial overgrowth in postgastrectomy patients. Neurogastroenterol Motility. 2011;23:e191–e196. https://doi.org/10.1111/j.1365-2982.2011.01686.x.
Perez Aisa A, Garcia Gavilan MC, Alcaide Garcia J, et al. Small intestinal bacterial overgrowth is common after gastrectomy but with little impact on nutritional status. Gastroenterol Hepatol. 2019;42:1–10. https://doi.org/10.1016/j.gastrohep.2018.07.001.
Mouillot T, Rhyman N, Gauthier C, et al. Study of small intestinal bacterial overgrowth in a cohort of patients with abdominal symptoms who underwent bariatric surgery. Obes Surg. 2020;30:2331–2337. https://doi.org/10.1007/s11695-020-04477-5.
Di Stefano M, Mengoli C, Bergonzi M, Miceli E, Pagani E, Corazza GR. Hydrogen breath test in patients with severe constipation: the interference of the mixing of intestinal content. Neurogastroenterology and motility: the official journal of the European Gastrointestinal Motility Society.. 2014;26:1754–1760. https://doi.org/10.1111/nmo.12456.
Brummer RJ, Armbrecht U, Bosaeus I, Dotevall G, Stockbruegger RW. The hydrogen (H2) breath test. Sampling methods and the influence of dietary fibre on fasting level. Scand J Gastroenterol.. 1985;20(8):1007–1013. https://doi.org/10.3109/00365528509088863.
Di Stefano M, Miceli E, Missanelli A, Malservisi S, Strocchi A, Corazza GR. Fermentation of endogenous substrates is responsible for increased fasting breath hydrogen levels in celiac disease. J Lab Clin Med. 2004;143:163–168. https://doi.org/10.1016/j.lab.2003.11.006.
Rana SV, Sharma S, Sinha SK, Kaur J, Prasad KK, Singh K. Influence of previously ingested wheat on fasting breath hydrogen in celiac patients. Dig Dis Sci. 2009;54:1276–1279. https://doi.org/10.1007/s10620-008-0496-3.
Strocchi A, Ellis CJ, Furne JK, Levitt MD. Study of constancy of hydrogen-consuming flora of human colon. Dig Dis Sci. 1994;39:494–497. https://doi.org/10.1007/bf02088333.
Jonderko K, Gabriel-Jasniok A, Szymszal M, Kasicka-Jonderko A, Blonska-Fajfrowska B. Unreliability of breath methane as a candidate indicator of functional bowel disorders. Gut Liver. 2008;2:180–185. https://doi.org/10.5009/gnl.2008.2.3.180.
Harvie RM, Tuck CJ, Schultz M. Evaluation of lactulose, lactose, and fructose breath testing in clinical practice: a focus on methane. JGH Open. 2020;4:198–205. https://doi.org/10.1002/jgh3.12240.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Massey, B.T., Wald, A. Small Intestinal Bacterial Overgrowth Syndrome: A Guide for the Appropriate Use of Breath Testing. Dig Dis Sci 66, 338–347 (2021). https://doi.org/10.1007/s10620-020-06623-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-020-06623-6