Abstract
Background: Studies of lymph node micrometastases in patients with colorectal cancer have ignored the prognostic significance of the number and level of lymph node micrometastases. The aim of this study was to clarify the prognostic significance of the status of lymph node micrometastases in histologically node-negative colorectal cancer.
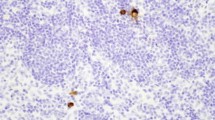
Methods: We used immunohistochemistry with anti-cytokeratin antibody CAM5.2 to examine 1013 lymph nodes in 42 patients (12 recurrent and 30 nonrecurrent) with histologically determined Dukes’ B colorectal cancer. Five serial 6-μm sections were used for immunohistochemical staining. The frequency, tumor cell pattern, and number and level of lymph node micrometastases were compared between the recurrent and nonrecurrent groups.
Results: Micrometastasis was confirmed in 16% (59/373) of lymph nodes in the recurrent group and 12% (77/640) of lymph nodes in the nonrecurrent group, and the frequency of lymph node micrometastases was 92% (11/12) in the recurrent group and 70% (21/30) in the nonrecurrent group. The tumor cell pattern in the metastatic lymph nodes was similar in the recurrent and nonrecurrent groups. Micrometastasis in four or more lymph nodes occurred more frequently in the recurrent group than in the nonrecurrent group (58% vs. 20%, P < .05), and micrometastasis to N2 or higher nodes occurred more frequently in the recurrent group than in the nonrecurrent group (92% vs. 47%, P < .01).
Conclusions: The number and level of positive micrometastatic lymph nodes was significantly correlated with postoperative recurrence of histologically determined Dukes’ B colorectal cancer. This parameter is a useful prognostic indicator in histologically node-negative colorectal cancer and is helpful in planning adjuvant chemotherapy.
Similar content being viewed by others
References
Beahrs OH. Colorectal cancer staging as a prognostic feature. Cancer 1982; 50: 2615–7.
Jass JR, Atkin WS, Cuzick J, et al. The grading of rectal cancer: historical perspectives and a multivariate analysis of 447 cases. Histopathology 1986; 10: 437–59.
Chapuis PH, Dent OF, Fisher R, et al. A multivariate analysis of clinical and pathological variables in prognosis after resection of large bowel cancer. Br J Surg 1985; 72: 698–702.
Fisher ER, Sass R, Palekar A, et al. Dukes’ classification revisited: findings from the National Surgical Adjuvant Breast and Bowel Projects (protocol R-01). Cancer 1989; 64: 2354–60.
Newland RC, Chapuis PH, Pheils MT, et al. The relationship of survival to staging and grading of colorectal carcinoma: a prospective study of 503 cases. Cancer 1981; 47: 1424–9.
Kune GA, Kune S, Field B, et al. Survival in patients with large bowel cancer: a population-based investigation from the Melbourne colorectal cancer study. Dis Colon Rectum 1990; 33: 938–46.
Moll R, Franke WW, Schiller DL, et al. The catalog of human cytokeratins: patterns of expression in normal epithelia, tumors and cultured cells. Cell 1982; 31: 11–24.
Haboubi NY, Clark P, Kaftan SM, et al. The importance of combining xylene clearance and immunohistochemistry in the accurate staging of colorectal carcinoma. J R Soc Med 1992; 85: 386–8.
Cooper D, Schermer A, Sun TT. Classification of human epithelia and their neoplasms using monoclonal antibodies to keratins: strategies, applications, and limitations. Lab Invest 1985; 52: 243–56.
Cutait R, Alves VA, Lopes LC, et al. Restaging of colorectal cancer based on the identification of lymph node micrometastases through immunoperoxidase staining of CEA and cytokeratins. Dis Colon Rectum 1991; 34: 917–20.
Jeffers MD, O’Dowd GM, Mulcahy H, et al. The prognostic significance of immunohistochemically detected lymph node micrometastases in colorectal carcinoma. J Pathol 1994; 172: 183–7.
ÖbergÅ, Stenling R, Tavelin B, et al. Are lymph node micrometastases of any clinical significance in Dukes’ stages A and B colorectal cancer? Dis Colon Rectum 1998; 41: 1244–9.
Adell G, Boeryd B, FrånlundB, et al. Occurrence and prognostic importance of micrometastases in regional lymph nodes in Dukes’ B colorectal carcinoma: an immunohistochemical study. Eur J Surg 1996; 162: 637–42.
Broll R, Schauer V, Schimmelpenning H, et al. Prognostic relevance of occult tumor cells in lymph nodes of colorectal carcinomas: an immunohistochemical study. Dis Colon Rectum 1997; 40: 1465–71.
Japanese Society for Cancer of the Colon and Rectum. Japanese Classification of Colorectal Carcinoma. 1st ed. Tokyo: Kanehara, 1997:4–40.
Makin CA, Bobrow LG, Bodmer WF. Monoclonal antibody to cytokeratin for use in routine histopathology. J Clin Pathol 1984; 37: 975–83.
Adachi Y, Inomata M, Miyazaki N, et al. Distribution of lymph node metastasis and level of inferior mesenteric artery ligation in colorectal cancer. J Clin Gastroenterol 1998; 26: 179–82.
Tang R, Wang JY, Chen JS, et al. Survival impact of lymph node metastasis in TNM stage III carcinoma of the colon and rectum. J Am Coll Surg 1995; 180: 705–12.
Cohen AM, Tremiterra S, Candela F, et al. Prognosis of node-positive colon cancer. Cancer 1991; 67: 1859–61.
Hida J, Yasutomi M, Fujimoto K, et al. Comparison between the Japanese general rules and the TNM system in the regional lymph node classification of carcinoma of the colon. J Am Coll Surg 1996; 183: 611–5.
Kayama K, Ohta H, Ueno M, et al. Study on grading and grouping of lymph node metastasis of colon and rectum by Japanese Research Society [in Japanese with English abstract]. J Jpn Soc Coloproctol 1998; 51: 57–64.
Greenson JK, Isenhart CE, Rice R, et al. Identification of occult micrometastases in pericolic lymph nodes of Dukes’ B colorectal cancer patients using monoclonal antibodies against cytokeratin and CC49: correlation with long-term survival. Cancer 1994; 73: 563–9.
Sasaki M, Watanabe H, Jass JR, et al. Occult lymph node metastases detected by cytokeratin immunohistochemistry predict recurrence in “node-negative” colorectal cancer. J Gastroenterol 1997; 32: 758–64.
Sasaki M, Watanabe H, Jass JR, et al. Immunoperoxidase staining for cytokeratins 8 and 18 is very sensitive for detection of occult node metastasis of colorectal cancer: a comparison with genetic analysis of. K-ras. Histopathology 1998; 32: 199–208.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Yasuda, K., Adachi, Y., Shiraishi, N. et al. Pattern of Lymph Node Micrometastasis and Prognosis of Patients with Colorectal Cancer. Ann Surg Oncol 8, 300–304 (2001). https://doi.org/10.1007/s10434-001-0300-5
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s10434-001-0300-5