Abstract
Background
The current AJCC staging system for gastric cancer (AJCC7) incorporated several major revisions to the previous edition. The T and N categories and the stage groups were newly defined, and adenocarcinoma of the esophagogastric junction (EGJ) was reclassified and staged according to the esophageal system. Studies to validate these changes showed inconsistent results. The International Gastric Cancer Association (IGCA) launched a project to support evidence-based revisions to the next edition of the AJCC staging system.
Methods
Clinical and pathological data on patients who underwent curative gastrectomy at 59 institutions in 15 countries between 2000 and 2004 were retrospectively collected. Patients lost to follow-up within 5 years of surgery were excluded. Patients treated with neoadjuvant therapy were excluded. The data were analyzed in total, and separately by region of treatment.
Results
Of 25,411 eligible cases, 84.8 % were submitted from 24 institutions of Japan and Korea, 6.4 % from other Asian countries, and 8.8 % from 29 Western institutions. The T and N categories of AJCC7 clearly stratified the patient survival. Patients with pN3a and pN3b showed distinct prognosis in all regions, and by introducing pN3a and pN3b into a cluster analysis, we established a new stage grouping with better stratification than AJCC7, especially among stage III subgroups. Survival of Siewert type 2 and 3 EGJ tumors was better stratified by this IGCA stage grouping than by either esophageal or gastric scheme of AJCC7.
Conclusions
For the next revision of AJCC classification, we propose a new stage grouping based on a large, worldwide data collection.
Similar content being viewed by others
Introduction
The tumor-node-metastasis (TNM) classification by the Union for International Cancer Control (UICC) and American Joint Committee on Cancer (AJCC) is the global standard to stage solid tumors [1, 2]. The current 7th edition (AJCC7) underwent several major revisions in the chapters of esophagus and stomach, including refinements in the definitions of T and N categories and stage grouping, and the staging of all tumors of the EGJ according to the esophageal system. Before to this revision, the Worldwide Esophageal Cancer Collaboration (WECC) had assembled a large multi-institutional international database and proposed a new staging system for esophageal cancer [3, 4]. The WECC leadership proposed that this system also be applied to gastric cancer, but the esophageal stage grouping did not perform well for distal gastric cancers. A new stage grouping for gastric cancer was counter proposed based on Japanese and Korean databases, using the WECC-defined T and N categories, and it has been adopted in AJCC7 [5]. Thus the current TNM classification for gastric cancer is a “hybrid” of the T and N categories defined using the worldwide esophageal cancer dataset and the stage groups defined using Japanese and Korean databases [6].
Since adoption and publication of the AJCC7 staging system, a number of studies evaluating this new classification have been published [7–11]. Although most authors generally approve its prognostic value, its complexity is often criticized. AJCC6 had six stage groups from IA to IV, while AJCC7 has eight stage groups, adding two additional subgroups (IIB and IIIC), with no concomitant improvement in ability to predict stage-based outcome. A number of studies have suggested that cancer of the EGJ, especially Siewert type 2 and 3, were better risk stratified by the gastric rather that the esophageal staging system [12, 13]. The AJCC7 gastric staging system recognized the prognostic difference between pN3a and pN3b, but failed to incorporate N3b into any stage group.
The International Gastric Cancer Association (IGCA) is an academic group having 1400 members from 57 countries. In 2009, the association launched a staging project with the aim of collecting gastric cancer data worldwide to formulate a contemporary evidence based classification that would reflect patients’ prognosis across the global spectrum of this disease.
Materials and methods
Project organization
A project-specific data center was set up in the nonprofit organization Japan Clinical Research Support Unit (J-CRSU) with two biostatisticians (Y. Y., Y. O.). In addition to the operation office in Tokyo (T. S.), four researchers served as regional representative (D. C., F. R., P. K, and H. H. K. from North America, Europe, South America, and Korea, respectively) and took charge of data collection in each region.
Participating institutions
Data were collected on an institutional basis. In Japan and Korea, the Japanese Gastric Cancer Association (JGCA) and Korean Gastric Cancer Association (KGCA) had established nationwide database systems for gastric cancer. The Registration Committee of these Associations nominated their leading institutions to participate individually in the project. Besides these two countries, active IGCA members in major institutions around the world were invited to contribute data to the project. The ethical research committee of each participating institution approved the project protocol.
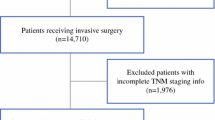
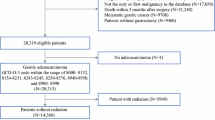
Patients
Based on the preliminary inquiry to participating institutions, it was planned to collect data of 25,000 patients: 10,000 each from Japan and Korea, and 5,000 from other countries. As AJCC7 has a general rule that stage IV means M1 disease, only M0 cases with complete follow-up were collected. The inclusion criteria were: histologically proven adenocarcinoma of the stomach or esophagogastric junction (Siewert type 2 or 3); R0 resection was performed during the 5-year period between January 2000 and December 2004; the patient’s vital status at the 5th postoperative year (alive, or date of death) must be confirmed; no chemotherapy or radiation therapy was given before surgery. Cases of gastric stump carcinoma and operative deaths were excluded.
Data collection and analysis
The data center sent a specially designed Excel spreadsheet to participating institutions by e-mail. Thirty clinical and pathological factors listed in Electronic Supplementary Material 1 were requested, of which 18 were mandatory. The returned spreadsheets were checked for validity and the data were integrated and analyzed using SAS software, version 9.2 (SAS Institute, Cary, NC, USA). Overall survival (OS) was calculated from the date of surgery to the date of death from any cause and was censored at 5 years. Survival curves were estimated using the Kaplan–Meier method, and compared by means of log-rank test. For stage grouping, a cluster analysis (k-means clustering) was performed for estimated hazard ratios, and the proposed model was compared with the AJCC7 stage groupings using the Schwarz Bayesian criterion.
Results
In response to the initial IGCA invitation, 72 institutions agreed to participate in the project, and 62 submitted the datasheet by December 2013. Preliminary data screening and subsequent inquiries identified three institutions whose data lacked information on at least one mandatory field; these patients were excluded. Ultimately, we collected analytical data on 25,411 patients from 59 institutions in 15 countries (Table 1, Appendix 1, Electronic supplementary material 2–1). All analyses were made using the total data, as well as for each of the four country/regional categories: Japan, Korea, other Asia, and the West, accounting for 41.8 %, 43.0 %, 6.4 %, and 8.8 % of the study population, respectively.
Patients, tumors, and surgery
Table 2 shows clinical and pathological features of the study population. Korean patients were younger, and Western patients were more often female, than other regions. The majority of the tumors were located in the distal two-thirds of the stomach in all regions. Siewert type 2 and 3 esophagogastric junction (EGJ) tumors accounted for 4.6 % of all cases, and their proportion in the Western patients (18.0 %) was significantly higher than in other regions. The proportion of pT1 tumors (early gastric cancer, EGC) was significantly higher in Japan (58 %) and Korea (48 %) than in the West (28 %) and other Asia (18 %). Results of peritoneal lavage cytology were reported in 25 % of all cases, of which 390 patients (1.5 %) were positive; positive cytology patients were excluded from survival analysis, because positive cytology (Cy+) is regarded as M1 in AJCC7.
Distal gastrectomy was the most frequently performed operation in all regions, followed by total and proximal gastrectomy. D2 or extended lymphadenectomy was performed in the majority of this study population. The median number of retrieved lymph nodes per patient was 32, which was highest in Japan (36) and lowest in other parts of Asia (22). The proportion of D0/D1 lymphadenectomy was highest in Japan (40.9 %), a finding associated with the high incidence of EGC.
Information about postoperative adjuvant therapy was incomplete in many institutions in this study. Among the cases having this information, 69.7 % of patients did not receive adjuvant chemotherapy. Patients with advanced-stage disease tended to receive such therapy. Adjuvant radiotherapy was uncommon in all regions.
T and N categories and survival
Survival curves according to the histological depth of tumor invasion (pT) and the number of regional lymph nodes with histological metastasis (pN) as defined in AJCC7 are shown in Fig. 1a, b, respectively. Survival decreased in a stepwise fashion with increasing pT. Although the difference between pT1a and pT1b was small, it was statistically significant. Survival also decreased in a stepwise fashion with increasing pN, with almost identical intervals between the curves. These trends were seen equally in all regions.
Cluster analyses and proposal of new stage grouping
The patients were divided into 25 groups according to their tumor/node status by combining five T categories (1/2/3/4a/4b) and five N categories (0/1/2/3a/3b), from T1N0, T1N1…to T4bN3b. In cluster analysis, the distance between a group and the base group (T1N0) was calculated based on the number of deaths in each group during the postoperative 5-year period, and the groups were clustered into seven (Fig. 2a) stage groups from IA to IIIC. We propose this matrix as “IGCA stage grouping.”
Seven of the 25 groups in the IGCA stage grouping have a different definition from their counterparts in the AJCC7 (Fig. 2b), mostly in the subgroups of stage III. The influence of N3a and N3b on outcome was the principal reason for this difference. As shown in Fig. 3, the largest subgroup of stage III by the AJCC7 is IIIC, whereas the largest subgroup in the IGCA stage grouping proposal is IIIA. Survival curves according to the stage grouping in the two systems (Fig. 4a, b) reflect this difference in distribution of stage III patients: the IGCA stage grouping widens the distance between the curves, thus better stratifies the survival probabilities.
The proposed IGCA stage grouping system was derived from the entire cohort of patents. Although the analysis is heavily influenced by the preponderance of Japanese and Korean patients, it appears to be valid in risk stratification for other Asian and Western patients as well (Electronic supplementary material 2–2).
EGJ tumors (Siewert type 2 and 3)
A total of 1170 patients were reported to have an EGJ tumor of Siewert type 2 or 3, of which 34.2 % were Western patients. Figure 5a, b, c shows survival curves according to the stage grouping by the AJCC7 esophageal system, by the AJCC7 gastric system, and by the proposed IGCA system, respectively. In the esophageal system, almost 40 % of tumors were classified as stage IIIC, and the survival curves of stage IIA and IIB were reversed. In the gastric system, the subgroups show a more balanced case distribution and the survival was better stratified than by esophageal scheme. The Schwarz Bayesian criterion selected the IGCA stage grouping as the best model among the three. Both Siewert type 2 (n = 554) and type 3 (n = 616) tumors were well stratified by this scheme (Electronic supplementary material 2–3).
Discussion
Gastric cancer shows large geographic differences in the world, not only in incidence and mortality but also in treatment results [14, 15]. The remarkable difference of long-term survival after curative surgery between the East and the West is attributable primarily to the differences in disease stage at presentation. Differences in stage-specific outcomes between East and West can be at least partly attributed to stage migration associated with differences in the extent of surgery and the pathological handling of dissected lymph nodes [16]. To appropriately compare treatment results in different regions, common staging rules of the disease using widely available prognostic factors are needed. The UICC/AJCC TNM classification is the global standard and should be constantly reviewed and refined based on worldwide data.
The IGCA Gastric Cancer Staging Project was launched to establish a classification that is applicable worldwide. We chose not to collect data from existing administrative databases such as the American Surveillance, Epidemiology, and End Results program or National Cancer Database, or the JGCA Registry. To assure high-quality contemporary data, for this project we requested specifically prepared datasets from individual high-volume institutions. The strength of this study includes the large sample size (25,411 patients), geographic variety (15 countries from the East and West), a short, recent, defined period of treatment (surgery during the 5 years between 2000 and 2004), and complete 5-year follow-up data. Weaknesses of this methodology include the retrospective nature of the data, incomplete data on postoperative treatments, and the lack of standardized methods of pathological handling of the specimens.
The vast majority of data were from Japan and Korea because the patient volume of specialized institutions in these countries is much larger than in the rest of the world, and institutional databases are well established. We would have been able to collect far more data from these two countries, but restricted the number of institutions in consideration of the balance in the world. Although results of this study are heavily influenced by the data from Japan and Korea, all analyses were validated separately in the other regions (Other Asia and West). Although the survival of each stage group is different among the regions, the IGCA stage grouping stratifies survival very well within each region (Electronic supplementary material 2–2).
The fact that only specialized major institutions submitted the data may raise concern that the results do not necessarily represent the general practice, particularly in the Western series: in this study, D2 lymphadenectomy was performed in 79 % of the Western institutions. The median number of examined nodes was as many as 27, much higher than the number of examined nodes reported from administrative databases. However, the goal of this study was not to find a simple staging method using limited information but to establish an accurate prognostic classification using sufficient surgical and pathological information, regardless of the regional differences in general practice.
We excluded patients receiving neoadjuvant therapy because of the potential for neoadjuvant therapy to affect pathological staging of the resected specimen. As the neoadjuvant strategy had already been adopted widely in the West during the study period of this project, several institutions in the United States and the United Kingdom could not contribute patients to our dataset. The aim of this study is to establish a pathological classification of the original, non-pretreated gastric cancer to correctly stratify patient prognosis. In the future, when we have sufficient clinical/pathological and outcome data on patients treated with neoadjuvant therapy, we will be able to derive a separate “yp” staging system. The data of the current project should provide the basis for that.
On the other hand, we did include patients who received postoperative adjuvant therapy from the study for the following reasons. In this retrospective survey, the quality of data on postoperative therapy was inadequate for analysis because of missing information and the wide range of adjuvant regimens employed. If we excluded patients in whom postoperative adjuvant therapy status was unknown or those patients who received adjuvant therapy, it would have introduced significant selection bias, especially among patients with stage II/III disease.
The TNM classification has undergone several major revisions in its half-century history. The 4th edition (1987) had two levels of regional lymph node metastasis (N1/N2) based on the anatomical location of the positive nodes. Then, the 5th edition (1997) had three levels based on the number of positive nodes: N1 = 1–6 positive nodes; N2 = 7–15 nodes; N3 = more than 15 nodes. In the 7th edition (2010), the cutoff levels of N category were changed to harmonize with esophageal cancer: N1 = 1–2 nodes; N2 = 3–6 nodes; N3 = more than 6 nodes. The definition of T-category has been also changed to harmonize with other gastrointestinal tract: T2/T3/T4a/T4b.
With the large database assembled for this project, we first examined the validity of definitions of T and N categories of AJCC7. Our analyses in the current dataset verified that the T and N categories in AJCC7 stratify patient survival quite well (Fig. 1a, b). Thus we decided not to seek further subclassifications of tumor depth or cutoff numbers of lymph nodes; we thought that minor modifications of these well-established categories would be confusing for clinicians and researchers without improving the classification.
We then evaluated the stage grouping. In AJCC7, the former N2 (7–15 positive nodes) and N3 (more than 15 nodes) were renamed as N3a and N3b, and grouped together as N3 for defining stage groups. This point was also a part of harmonization with esophageal cancer in which metastasis in more than 6 nodes means very poor prognosis [3]. In contrast to esophageal cancer, where involvement of more than 6 nodes is not associated with worse survival than involvement of 6 nodes, in gastric cancer there was a significant difference in survival comparing N3a to N3b (Fig. 1b). This trend was observed in the entire patient cohort, as well as in each region. N3a and N3b were designated as separate groups in the stage grouping cluster analysis and N3b maintained definite survival impact. With this modification, the distribution of patients in stage III subgroups changed (Fig. 3), and the survival curves became more distinct from each other (Fig. 4).
Staging of EGJ tumors has caused controversy since AJCC7 adopted the rule that a tumor whose epicenter is within 5 cm of the EGJ and extends into the esophagus is classified and staged according to the esophageal system. This rule did not mean that EGJ tumors should be treated as esophageal cancer, but did provoke opposition from gastric surgeons [11]. In the first instance, the initial WECC dataset upon which this recommendation was made had no information on Siewert type; tumors of the gastric cardia (type 3) were grouped with tumors arising in a background of Barrett’s dysplasia (type 1). In this IGCA project, we collected the data on 1170 patients with a Siewert type 2 or 3 tumor and tested the three staging systems in survival analysis (Fig. 5a, b, c). The best stratification was obtained by the IGCA stage grouping. As compared to non-EGJ tumors (Fig. 4a), survival of EGJ tumors (Fig. 5c) was generally inferior in each stage, probably reflecting the different tumor biology and/or difficult surgical approach. However, those factors that govern outcome within the subgroup of patients with Siewert type 2 and 3 tumors are much better characterized by the proposed IGCA gastric cancer system than by the existing AJCC7 esophageal system. As such, we propose that the IGCA gastric system is more appropriate to risk stratify patients with Siewert type 2 and 3 tumors. Accurate staging of patients with locoregionally advanced EGJ cancers will be further complicated by the fact that most of those patients are now treated with neoadjuvant chemotherapy with or without radiation. Staging of EGJ patients based on treatment with surgery alone is now almost obsolete, and efforts to create an “yp” staging system are likely to be an important component of AJCC8.
In conclusion, based on our analysis of this global dataset, we propose a new evidence-based stage grouping for gastric cancer, including Siewert type 2 and 3 EGJ adenocarcinoma. The new system more accurately risk stratifies patients with gastric cancer than the AJCC7 system, and much more accurately risk stratifies patients with Siewert type 2 and 3 EGJ cancer than the AJCC7 esophageal system. The system has been derived from and is applicable to patients with gastric cancer from all regions of the world. We believe it to be suitable for the next edition of the AJCC gastric cancer staging system.
References
Sobin L, Gospodarowicz MK, Wittekind C. TNM classification of malignant tumours. 7th ed. Hoboken: Wiley-Blackwell; 2009.
Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A. AJCC cancer staging manual. 7th ed. Berlin: Springer; 2009.
Rice TW, Rusch VW, Apperson-Hansen C, et al. Worldwide esophageal cancer collaboration. Dis Esophagus. 2009;22(1):1–8.
Rice TW, Rusch VW, Ishwaran H, Blackstone EH. Cancer of the esophagus and esophagogastric junction: data-driven staging for the seventh edition of the American Joint Committee on Cancer/International Union Against Cancer Cancer Staging Manuals. Cancer (Phila). 2010;116(16):3763–73.
Washington K. 7th edition of the AJCC cancer staging manual: stomach. Ann Surg Oncol. 2010;17:3077–9.
Ahn HS, Lee HJ, Hahn S, Kim WH, Lee KU, Sano T, et al. Evaluation of the seventh American Joint Committee on Cancer/International Union Against Cancer classification of gastric adenocarcinoma in comparison with the sixth classification. Cancer (Phila). 2010;116(24):5592–8.
Chae S, Lee A, Lee JH. The effectiveness of the new (7th) UICC N classification in the prognosis evaluation of gastric cancer patients: a comparative study between the 5th/6th and 7th UICC N classification. Gastric Cancer. 2011;14:166–71.
Fang WL, Huang KH, Chen JH, et al. Comparison of the survival difference between AJCC 6th and 7th editions for gastric cancer patients. World J Surg. 2011;35:2723–9.
Marrelli D, Morgagni P, de Manzoni G, et al. Prognostic value of the 7th AJCC/UICC TNM classification of noncardia gastric cancer: analysis of a large series from specialized Western centers. Ann Surg. 2012;255:486–91.
Sun Z, Wang ZN, Zhu Z, et al. Evaluation of the seventh edition of American Joint Committee on Cancer TNM staging system for gastric cancer: results from a Chinese monoinstitutional study. Ann Surg Oncol. 2012;19:1918–27.
Dikken JL, van de Velde CJH, Goenen M, et al. The New American Joint Committee on Cancer/International Union Against Cancer staging system for adenocarcinoma of the stomach: increased complexity without clear improvement in predictive accuracy. Ann Surg Oncol. 2012;19:2443–51.
Huang Q, Shi J, Feng A, et al. Gastric cardia carcinomas involving the esophagus are more adequately staged as gastric cancers by the 7th edition of the American Joint Committee on Cancer Staging System. Mod Pathol. 2011;24:138–46.
Suh YS, Han DS, Kong SH, et al. Should adenocarcinoma of the esophagogastric junction be classified as esophageal cancer? A comparative analysis according to the seventh AJCC TNM classification. Ann Surg. 2012;255:908–15.
Strong VE, Song KY, Park CH, et al. Comparison of gastric cancer survival following R0 resection in the United States and Korea using an internationally validated nomogram. Ann Surg. 2010;251:640–6.
Markar SR, Karthikesalingam A, Jackson D, Hanna GB. Long-term survival after gastrectomy for cancer in randomized, controlled oncological trials: comparison between West and East. Ann Surg Oncol. 2013;20:2328–38.
Davis PA, Sano T. The difference in gastric cancer between Japan, USA and Europe: What are the facts? What are the suggestions? Crit Rev Oncol Hematol. 2001;40:77–94.
Acknowledgments
We thank Dr. Susumu Aikou, University of Tokyo, and Ms. Yoko Koshio, J-CRSU, for their dedication to the data handling. We also thank Taiho Pharmaceutical Company Limited for their financial support for the project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions. Informed consent or a substitute for it was not obtained from patients for being included in the study because this is a retrospective data collection from established database in each participating institution. Instead, as mentioned in the text, the study was approved by the IRB of all institutions.
Additional information
For IGCA Staging Project.
H. H. Kim: representing the Korean Gastric Cancer Association.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix 1: Participating institutions (in alphabetical order in each region)
Appendix 1: Participating institutions (in alphabetical order in each region)
Japan: Aichi Cancer Center Hospital, Chiba Cancer Center, Hiroshima City Hospital, Iwate Prefectural Central Hospital, Kanagawa Cancer Center, Keio University Hospital, Keiyukai Sapporo Hospital, Kurashiki Central Hospital, National Cancer Center Hospital, National Hospital Organization Osaka National Hospital, Niigata Cancer Center Hospital, Osaka Medical Center for Cancer and Cardiovascular Diseases, Shikoku Cancer Center, The Cancer Institute Hospital of JFCR, Tochigi Cancer Center, Toyama Prefectural Central Hospital, Yamagata Prefectural Central Hospital. Korea: Ajou University, Asan Medical Center, Catholic University, Chonnam National University, Korea University, National Cancer Center, Samsung Medical Center, Seoul National University, Yonsei University. Other Asia: Beijing Cancer Hospital (China), National University of Singapore (Singapore), National Yang-Ming Hospital (Taiwan), Prince of Wales Hospital (Hong Kong), Shanghai Jiao Tong University (China), Tianjin Medical University Cancer Institute (China). West: Azienda Ospedaliera Citta della Salute e della Scienza di Torino, Turin (Italy), Busto Arsizio Hospital, Varese (Italy), Catholic University, Rome (Italy), Cologne University (Germany), Federal University of Sao Paulo (Brazil), Hospital Mutua de Terrassa, Barcelona (Spain), Humanitas Clinical and Research Center, Milan (Italy), Istituto Tumori G. Paolo II, Bari (Italy).
Karolinska University Hospital (Sweden), Leiden University (Netherlands), Memorial Sloan-Kettering Cancer Center (USA), Morgagni-Pierantoni Hospital, Forlì (Italy), Princess Alexandra Hospital, Brisbane (Australia), Regina Elena National Cancer Institute, Rome (Italy), San Raffaele Scientific Institute, Milan (Italy), Santa Casa Medical School (Brazil), San Vincenzo Hospital, Taormina, Messina (Italy), Second University of Naples (Italy), Technical University of Munich (Germany), University of Brescia (Italy), University of Chile (Chile), University of Florence (Italy), University of Heidelberg (Germany), University of Insubria, Varese (Italy), University of Padova (Italy), University of Perugia (Italy), University of Sao Paulo (Brazil), University of Siena (Italy), University of Verona (Italy), Valdarno Hospital, Arezzo (Italy).
Rights and permissions
About this article
Cite this article
Sano, T., Coit, D.G., Kim, H.H. et al. Proposal of a new stage grouping of gastric cancer for TNM classification: International Gastric Cancer Association staging project. Gastric Cancer 20, 217–225 (2017). https://doi.org/10.1007/s10120-016-0601-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-016-0601-9