Abstract
Liver metastases from gastric cancer are rarely indicated for surgery because they are often diagnosed as multiple nodules occupying both lobes and coexist with extrahepatic disease. A literature search identified no clinical trials on hepatectomy for this disease; only retrospective studies of a relatively small number of cases collected over more than a decade, mostly from a single institution, were found. Five-year survival rates from these reports ranged from 0 % to 37 %, and long-term survivors were observed among carefully selected case series. The most commonly reported prognostic factor was the number of metastatic nodules, and patients with a solitary metastasis tended to have superior outcome. Patients diagnosed to have a small number of metastatic nodules by modern imaging tools could be indicated for surgery. Because both intrahepatic and extrahepatic recurrences are common, patients are likely to benefit from perioperative adjuvant chemotherapy, although it is not possible at this time to specify which regimen is the most appropriate.
Similar content being viewed by others
Introduction
Hepatectomy for liver metastases should only be attempted when cure is the goal because hepatectomy usually does not relieve symptoms. Colorectal liver metastases are widely considered as targets of surgery with intent to cure, because they often present as a liver-only disease [1], which is not always the case with other types of cancer. A prognostic model based on several prognostic factors effectively stratified cancers of various origins into three groups in a comprehensive analysis of various noncolorectal nonendocrine liver metastases treated by hepatectomy in 41 French centers [2]. Gastric cancer metastasis in that report was classified into the intermediate-risk group in which 5-year survival rate was in the range of 15–30 %, with hepatic metastasis from pancreatic cancer, melanoma, and duodenal cancer. The low-risk group with a 5-year survival rate >30 % consisted of metastases from adrenal cancer, ovarian cancer, breast cancer, and renal cancer among others, and a high-risk group with 5-year survival <15 % consisted of metastases from cancer of the lung, esophagus, head and neck, and gastroesophageal junction.
Gastric cancer is known to be heterogeneous in nature, consisting of cancer cells with varying biological characteristics. Gastric cancer can metastasize through the lymphatic pathway, the hematogenous pathway, and by direct dissemination into the peritoneal cavity from the serosal surface. Moreover, the fate of cancer cells that enter the portal circulation could vary. Hematogenous metastases can occur according to both the seed-and-soil hypothesis and the anatomical/mechanical hypothesis, neither of which needs to be mutually exclusive, and the extent to which either mechanism is operational depends on the tumor under investigation [3]. When gastric cancer cells spread through the hematogenous pathway, its first site of metastasis according to the anatomical/mechanical hypothesis would be the liver, followed by the lung. In addition, several gastric cancers spread along the seed-and-soil route, resulting in various distant metastases in the absence of hepatic metastases [4]. This result is in contrast with colorectal cancer in which the anatomical/mechanical hypothesis would seem more often applicable. The aggressive characteristics and unpredictable nature of gastric cancer cells are the reason that surgical resection of hepatic metastases has not been seriously considered.
However, some might not agree that gastric cancer even with solitary liver metastasis should always be considered as a contraindication for surgical treatment. The Japanese Gastric Cancer Treatment Guidelines recommend only chemotherapy, radiation, palliative surgery, and best supportive care for treatment of Stage IV or metastatic gastric cancer [5]. Recently, the guidelines committee of the Japan Gastric Cancer Association decided to revisit the treatment of potentially resectable M1 disease. A working group was organized to discuss whether any tentative comments could be added to the next version of the guidelines regarding surgical treatment with curative intent of (1) patients with resectable hepatic metastasis, (2) patients who are positive for cytological examination of peritoneal washes, and (3) patients with swollen nodes in the paraaortic region. This article is a summary of the literature search and discussion on gastric cancer hepatic metastasis by the members of the working group for this task.
Literature search
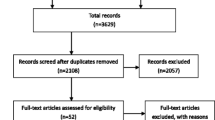
A search for relevant literature was conducted in March 2013 using PubMed and Scopus. Key search terms used included “gastric cancer,” “liver metastasis,” “hepatectomy,” and “surgery” to find articles on hepatectomy for gastric cancer metastasis to the liver that were published in English after 2000. Sixty-eight articles were identified, of which the following were excluded: 15 articles that included either other types of distant metastases or hepatic metastasis from other cancer types with no independent outcome data for gastric cancer metastases, 15 articles with emphasis on treatment modalities other than hepatectomy, 6 articles with fewer than 15 cases, 5 articles on prediction and diagnosis of hepatic metastasis, 4 review articles, 3 articles on irrelevant subjects, and 1 article describing only hepatic metastasis from pT1 stage cancer. Three articles analyzed patients from the same institution, and the most recent report by Takemura et al. [6] was selected and added to a total of 17 articles to be analyzed in the current review [2, 6–21]. Most of the papers were retrospective single-institution analyses of consecutive patients who underwent hepatectomy during a given period, with two exceptions in which patients were recruited from multiple institutions [5, 7]. Wang et al. [8] analyzed only patients with synchronous liver metastases, but all other papers discussed both synchronous and metachronous metastases. Two papers analyzed all patients with hepatic metastasis who underwent gastrectomy, regardless of whether the patients underwent hepatectomy [9, 10]. Data of the patients who went on to receive hepatectomy could be retrieved from these reports for subsequent analyses. A paper by Adam et al. was a comprehensive analysis of noncolorectal nonendocrine liver metastases [2], from which patients with gastric cancer metastases could be retrieved for some of the analyses in this review.
Results and discussion
The median number of patients analyzed among the 17 series was 25 (range, 15–73), spanning a median period of 15 years (range, 5–36). Details such as the indication for surgery, diagnostic modalities used, type of surgery performed, and adjuvant treatments given were diverse and, in addition, could have changed substantially in each institution during the periods studied. Synopses of findings in the 17 papers are summarized in Table 1.
The type of hepatectomy performed was diverse. A greater proportion of patients underwent wedge or nonanatomic resection of the metastatic nodules, and major hepatectomy such as hemihepatectomy was reserved for 23.4 % of the patients (79 of 337). The selection was presumably based on the number, size, and location of the tumors rather than the surgeons’ intent to perform anatomic resection for additional resection margin. In cases of colorectal liver metastasis, the preservation of hepatic parenchyma is considered to be of increasing importance in the setting of chemotherapy-associated steatohepatitis and the growing number of patients undergoing repeated metastectomy [22]. Even in gastric cancer metastasis, the most frequent pattern of recurrence was intrahepatic recurrence, observed in 79 % (166 of 209) of all the recurrences reported.
Mortality was 1.1 % (5/426) among the 15 studies in which the data were available, and morbidity ranged from 19 % to 47 % among 6 studies.
The 5-year survival reported from each series ranged from 0 % to 37 % and exceeded 30 % in five series [6, 10, 12, 15, 16]. Median survival time ranged from 9 to 38.8 months. The diversity in outcome may have reflected the diversity in patient selection and strategy taken, including the use of adjuvant therapies. The 5-year survival of all patients analyzed in the current study, calculated by dividing the number of 5-year survivors reported in each article by the total number of patients, was 18.8 % (97 of /515). Although these series should be considered to represent a well-selected and more favorable population compared with patients with liver metastases who were treated with systemic chemotherapy and had poorer outcome, the 5-year survival rate at 18.8 % obtained cannot be ignored as futile. Gastric cancer with liver metastases has long been considered as a systemic disease with no indication for surgery with curative intent. This point has been made clear, both in the National Comprehensive Cancer Network (NCCN) Guidelines Version 1.2013 [23] and in the Japanese Guidelines [5]. However, there are occasions when such metastases are found as clinically resectable disease, and whether these exceptions should still be treated either by palliative chemotherapy or supportive care could be an issue for debate.
Indication for surgery has not been established but could be considered based on analysis of prognostic factors. Independent prognostic factors identified through multivariate analyses were varied, and included the number of metastatic nodules, unilobular distribution, solitary tumor, tumor diameter, and capsular formation regarding hepatic tumors (Table 2). Among these, the “number of metastatic nodules” was considered to be an important factor across several series if “solitary metastasis” was to be included. Among 319 patients with relevant information in the current series, 195 (61.1 %) actually had solitary metastases. One should note, however, that the number of nodules can differ, depending on the type of imaging studies used [24, 25]. Because most institutions needed more than a decade to accumulate 15 patients or more, there should have been much difference in the potential of imaging modalities at the beginning and the end of the study period. In the largest single-institution series, Takemura et al.[6] reported a 5-year survival of 37 %. It may be of note that they currently consider surgery when the number of metastatic nodules was diagnosed as three or fewer, using state-of-the-art imaging tools. As for other prognostic factors, some have found metachronous hepatic metastases to be a sign of favorable prognosis [11, 12, 20] whereas others consider this as irrelevant. In addition, status of the primary tumor such as serosal invasion, lymphatic invasion, and clinical stage were listed as relevant prognostic factors.
It may be worthwhile to mention that the incidence of clinically resectable hepatic metastasis may be lower than what a surgeon expects. Sakamoto et al. [14] reported that they found synchronous liver metastases in 2.2 % of the 5,209 patients who underwent gastrectomy at National Cancer Center, Japan, whereas 1.3 % developed metachronous metastases. About 20 % of these patients underwent hepatectomy for cure. In contrast, 1,013 of 10,259 patients (9.9 %) diagnosed as gastric cancer in the Yonsei University Health System, Korea, had synchronous or metachronous liver metastases [9]. Of these, 58 had metastases confined to the liver and 41 (only 4 % of all patients with liver metastases) underwent surgery with curative intent, which denotes management of both the primary tumor and the liver. The five-year survival rate of these 41 patients was 20.8 %, and the median survival time fell just short of 20 months. In short, 20 % of the patients with liver metastases can be treated surgically in a situation where only patients with potentially resectable disease are referred, a situation possibly encountered at the surgical department in a high-volume cancer center. In contrast, resectable liver metastasis undoubtedly is a rare disease when one attempts to carefully select patients from all gastric cancer patients who visit a hospital.
Indication for the adjuvant therapy given perioperatively was even more varied among the researchers, as no trial-based evidence exists for the population who underwent hepatectomy for gastric cancer metastasis. Takemura et al. [6] took an aggressive approach in which 18 of 73 patients received neoadjuvant chemotherapy and 31 received postoperative chemotherapy, including 5 cases that received arterial infusion (HAIC) postoperatively. In contrast, Sakamoto et al. [14] reported that they delivered chemotherapy only for those who subsequently had recurrences. There is no prospective trial showing the effect of perioperative adjuvant therapies for gastric cancer metastases to the liver. The high incidence of recurrence implies that micrometastases remain in situ after surgery, however. That micrometastases could be managed by modern chemotherapeutic agents has been proven by several adjuvant chemotherapy trials [26–28]. Thus, there is a rationale for perioperative chemotherapy, or even HAIC, given the high incidence of recurrence within the liver. Chemotherapy delivered preoperatively could be useful to identify cancers that do not respond to chemotherapy and progress rapidly and to avoid futile surgery. All five series with 5-year survival >30 % reported details on adjuvant strategies, including neoadjuvant chemotherapy and HAIC. In contrast, none of the patients received chemotherapy until recurrence in another series by Sakamoto et al., who reported their 5-year survival at 11 % as unsatisfactory. These facts imply the relevance of perioperative chemotherapy, although outcomes obtained from retrospective case series should be interpreted with caution. Evidence at a higher level will not be available for the time being because the chances of conducting a decently designed trial to generate evidence for adjuvant therapies in a disease as rare as resectable gastric liver metastases would be sparse.
Systemic chemotherapy, HAIC, and radiofrequency ablation (RFA) are among other treatment modalities for gastric cancer metastasis to the liver. No prospective trial investigating systemic chemotherapy specified in hepatic metastases has been reported, with the exception of one small pilot study involving 8 patients [29]. In recent phase III trials of first-line chemotherapy against advanced/metastatic gastric cancer, median survival time ranged from 11 to 15 months [30–34]; 5-year survivors were rarely observed. In a report that integrated 643 patients enrolled in five separate prospective trials performed by the Japan Clinical Oncology Group, the 5-year survival rate of patients with metastasis confined to the liver and treated with systemic chemotherapy alone was 1.7 % [35]. Presumably, this series does not include patients with a relatively small cancer burden for whom indication for surgery was seriously considered, and comparison of survival data with those of highly selected patients who underwent surgical resection of the metastases needs to be interpreted with caution. Nevertheless, it remains impractical to hope to cure patients with gastric cancer metastases to the liver by systemic chemotherapy.
The rationale for HAIC is in high intrahepatic drug concentration in relationship to the systemic concentration [36]. A response rate >50 % has been reported that led to good local control [36, 37]. However, good local control did not necessarily lead to prolonged survival in cases of gastric cancer, in which extrahepatic metastases often emerge even during the course of successful liver-oriented treatment. In addition, an inadequately placed or malfunctioning catheter prevents efficient drug delivery [38]. Thus, catheter-related events such as occlusion, dislocation, and infection could result in interruption or termination of the treatment, even when the tumors are responding.
RFA has been attempted to treat selected patients with hepatic metastasis. The indication for RFA would include (1) liver-only disease; (2) size of the largest tumor less than 5 cm in diameter; and (3) location of tumor not adjacent to major vessels. RFA can be conducted either percutaneously under ultrasonic imaging guidance, laparoscopically, or by the open surgery approach. Reports on RFA applied to treat gastric cancer metastases to the liver remain scarce. Kim et al. [39] treated 20 patients by RFA or RFA and gastrectomy in case of synchronous metastases, achieving a median survival time of 30.7 months, whereas the experience by Kim et al. with 7 patients was more disappointing, with a median survival time of 11 months [40]. There is another report of 7 patients treated by HAIC followed by RFA who achieved a median survival time of 16.5 months [41]. This strategy was meant to select the patients so that RFA would only be delivered after confirming that new intrahepatic or systemic lesions do not develop during the HAIC. The chances of conducting a hepatectomy-versus-RFA trial for gastric cancer metastasis to the liver would seem unlikely. So far, the only clue of whether to perform hepatectomy or RFA comes from a meta-analysis of retrospective comparisons for colorectal liver metastases in which hepatectomy was significantly superior, even when conditions were limited to tumors >3 cm and solitary tumors [42]. Further prospective studies are needed to establish the position of RFA as an option for treatment of gastric liver metastases.
Conclusions
This working group reached the conclusion that hepatectomy could be considered in carefully selected cases of gastric cancer liver metastasis. The abstract of this article will appear in the forthcoming version of the Japanese gastric cancer treatment guidelines.
References
Shimada H, Tanaka K, Endou I, Ichikawa Y. Treatment for colorectal liver metastases: a review. Langenbecks Arch Surg. 2009;394:973–83.
Adam R, Chice L, Aloia T, Elias D, Salmon R, Rivoire M, et al. Hepatic resection for noncolorectal nonendocrine liver metastases. Analysis of 1425 patients and development of a prognostic model. Ann Surg. 2006;244:524–35.
Langley RR, Fidler IJ. The seed and soil hypothesis revisited: the role of tumor–stroma interactions in metastasis to different organs. Int J Cancer. 2011;128:2527–35.
Kodera Y, Ito S, Mochizuki Y, Yamamura Y, Misawa K, Ohashi N, et al. The number of metastatic lymph nodes is a significant risk factor for bone metastasis and poor outcome after surgery for linitis plastica-type gastric carcinoma. World J Surg. 2008;32:2015–20.
Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines (ver. 3). Gastric Cancer. 2010;2011(14):113–23.
Takemura N, Saiura A, Koga R, Arita J, Yoshioka R, Ono Y, et al. Long-term outcomes after surgical resection for gastric cancer liver metastasis: an analysis of 64 macroscopically complete resections. Langenbecks Arch Surg. 2012;397:951–7.
Shirabe K, Shimada M, Matsumata T, Higashi H, Yakeishi Y, Wakiyama S, et al. Analysis of the prognostic factors for liver metastasis of gastric cancer after hepatic resection: a multi-institutional study of the indication for resection. Hepatogastroenterology. 2003;50:1560–3.
Wang Y-N, Shen K-T, Ling J-Q, Gao X-D, Hou Y-Y, Wang X-F, et al. Prognostic analysis of combined curative resection of the stomach and liver lesions in 30 gastric cancer patients with synchronous liver metastases. BMC Surg. 2012;12:20.
Cheon SH, Rha SY, Jeung HC, Im CK, Kim SH, Kim HR, et al. Survival benefit of combined curative resection of the stomach (D2 resection) and liver in gastric cancer patients with liver metastases. Ann Oncol. 2008;19:1146–53.
Makino H, Kunisaki C, Izumisawa Y, Tokuhisa M, Oshima T, Nagano Y, et al. Indication for hepatic resection in the treatment of liver metastasis from gastric cancer. Anticancer Res. 2010;30:2367–76.
Ambiru S, Miyazaki M, Ito H, Nakagawa K, Shimizu H, Yoshidome H, et al. Benefits and limits of hepatic resection for gastric metastases. Am J Surg. 2001;151:279–83.
Okano K, Maeba T, Ishimura K, Karasawa Y, Goda F, Wakabayashi H, et al. Hepatic resection for metastatic tumors from gastric cancer. Ann Surg. 2002;235:86–91.
Zacherl J, Zacherl M, Scheuba C, Steininger R, Wenzl E, Muhlbacher F, et al. Analysis of hepatic resection of metastasis originating from gastric adenocarcinoma. J Gastrointest Surg. 2002;6:682–9.
Sakamoto Y, Sano T, Shimada K, Esaki M, Saka M, Fukagawa T, et al. Favorable indications for hepatectomy in patients with liver metastasis from gastric cancer. J Surg Oncol. 2007;95:534–9.
Morise Z, Sugiokla A, Hoshimoto S, Kato T, Ikeda M, Uyama I, et al. The role of hepatectomy for patients with liver metastases of gastric cancer. Hepatogastroenterology. 2008;55:1238–41.
Thelen A, Jonas S, Benckert C, Lopez-Hanninen E, Neumann U, Rudolph B, et al. Liver resection for metastatic gastric cancer. Eur J Surg Oncol. 2008;34:1328–34.
Tsujimoto H, Ichikura T, Ono S, Sugasawa H, Hiraki S, Sakamoto N, et al. Outcomes for patients following hepatic resection of metastatic tumors from gastric cancer. Hepatol Int. 2010;4:406–13.
Miki Y, Fujitani K, Hirao M, Kurokawa Y, Mano M, Tsujie M, et al. Significance of surgical treatment of liver metastases from gastric cancer. Anticancer Res. 2012;32:665–70.
Garancini M, Uggeri F, Degrate L, Nespoli L, Gianotti L, Nespoli A, et al. Surgical treatment of liver metastases of gastric cancer: is local treatment in a systemic disease worthwhile? HPB (Oxf). 2012;14:209–15.
Schildberg CW, Croner R, Merkel S, Schellerer V, Muller V, Yedibela S, et al. Outcome of operative therapy of hepatic metastatic stomach carcinoma: a retrospective analysis. World J Surg. 2012;36:872–8.
Imamura H, Matsuyama Y, Shimada R, Kubota M, Nakayama A, Kobayashi A, et al. A study of factors influencing prognosis after resection of hepatic metastases from colorectal and gastric carcinoma. Am J Gastroenterol. 2001;96:3178–84.
Sarpel U, Bonavia AS, Grucela A, Roayaie S, Schwarz ME, Labow DM. Does anatomic versus nonanatomic resection affect recurrence and survival in patients undergoing surgery for colorectal liver metastasis? Ann Surg Oncol. 2009;16:379–84.
Ajani JA, Barthel JS, Bekaii-Saab T, Bentrem DJ, D’Amico TA, Das P, et al. Gastric cancer. J Natl Compr Canc Netw. 2010;8:378–409.
Wang Z, Chen J-Q. Imaging in assessing hepatic and peritoneal metastases of gastric cancer: a systemic review. BMC Gastroenterol. 2011;11:19.
Maas M, Rutten IJG, Nelemans PJ, Lambregts DM, Cappendijk VC, Beets GL, et al. What is the most accurate whole-body imaging modality for assessment of local and distant recurrent disease in colorectal cancer? A meta-analysis. Eur J Nucl Med Mol Imaging. 2011;38:1560–71.
Sasako M, Sakuramoto S, Katai H, Kinoshita T, Furukawa H, Yamaguchi T, et al. Five-year outcomes of a randomized phase III trial comparing adjuvant chemotherapy with S-1 versus surgery alone in stage II or III gastric cancer. J Clin Oncol. 2011;29:4387–93.
Bang YJ, Kim YW, Yang HK, Chung HC, Park YK, Lee KH, et al. Adjuvant vapecitabine and oxaliplatin for gastric cancer after D2 gastrectomy (CLASSIC): a phase 3 open-label, randomised controlled trial. Lancet. 2012;379:315–21.
Cunningham D, Allum WH, Stenning SP, Thompson JN, Van de Velde CJ, Nicolson M, et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med. 2006;355:11–20.
Li Z-Y, Tang L, Zhang L-H, Bu Z-D, Wu A-W, Wu X-J, et al. Weekly docetaxel and cisplatin plus fluorouracil as a preoperative treatment for gastric cancer with synchronous multiple hepatic metastasis: a pilot study. Med Oncol. 2010;27:1314–8.
Bang YJ, Van Cutsem E, Feyereislova A, Chung HC, Shen L, Sawaki A, et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet. 2010;376:687–97.
Koizumi W, Narahara H, Hara T, Takagane A, Akiya T, Takagi M, et al. S-1 plus cisplatin versus S-1 alone for first-line treatment of advanced gastric cancer (SPIRITS trial): a phase III trial. Lancet Oncol. 2008;9:215–21.
Cunningham D, Starling N, Rao S, Iveson T, Nicolson M, Coxon F, et al. Capecitabine and oxaliplatin for advanced esophagogastric cancer. N Engl J Med. 2008;358:36–46.
Ohtsu A, Shah MA, Van Cutsem E, Rha SY, Sawaki A, Park SR, et al. Bevacizumab in combination with chemotherapy as first-line therapy in advanced gastric cancer: a randomized, double-blind, placebo-controlled phase III study. J Clin Oncol. 2011;29:3968–76.
Narahara H, Ishii H, Imamura H, Tsuburaya A, Chin K, Imamoto H, et al. Randomized phase III study comparing the efficacy and safety of irinotecan plus S-1 with S-1 alone as first-line treatment for advanced gastric cancer (study GC0301/TOP-002). Gastric Cancer. 2011;14:72–80.
Yoshida M, Ohtsu A, Boku N, Miyata Y, Shirao K, Shimada Y, et al. Longterm survival and prognostic factors in patients with metastatic gastric cancers treated with chemotherapy in the Japan Clinical Oncology Group (JCOG) study. Jpn J Clin Oncol. 2004;34:654–9.
Kumada T, Arai Y, Itoh K, Takayasu Y, Nakamura K, Ariyoshi Y, et al. Phase II study of combined administration of 5-fluorouracil, epirubicin and mitomycin-C by hepatic artery infusion in patients with liver metastases of gastric cancer. Oncology. 1999;57:216–23.
Ojima H, Ootake S, Yokobori T, Mochida Y, Hosouchi Y, Nishida Y, et al. Treatment of multiple liver metastasis from gastric carcinoma. World J Surg Oncol. 2007;5:70.
Inaba Y, Arai Y, Matsueda K, Takeuchi Y, Aramaki T. Right gastric artery embolization to prevent acute gastric mucosal lesions in patients undergoing repeat hepatic arterial infusion chemotherapy. J Vasc Interv Radiol. 2001;12:957–63.
Kim HR, Cheon SH, Lee KH, Ahn JR, Jeung HC, Lee SS, et al. Efficacy and feasibility of radiofrequency ablation for liver metastases from gastric adenocarcinoma. Int J Hypertherm. 2010;26:305–13.
Kim HO, Hwang SI, Hong HP, Yoo CH. Radiofrequency ablation for metachronous hepatic metastases from gastric cancer. Surg Laparosc Endosc Percutan Tech. 2009;19:208–12.
Yamakado K, Nakatsuka A, Takaki H, Mori Y, Tonouchi H, Kusunoki M, et al. Prospective study of arterial infusion chemotherapy followed by radiofrequency ablation for the treatment of liver metastasis of gastric cancer. J Vasc Interv Radiol. 2005;16:1747–51.
Weng M, Zhang Y, Zhou D, Yang Y, Tang Z, Zhao M, et al. Radiofrequency ablation versus resection for colorectal cancer liver metastases: a meta-analysis. PLoS One. 2012;7:e45493.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kodera, Y., Fujitani, K., Fukushima, N. et al. Surgical resection of hepatic metastasis from gastric cancer: a review and new recommendation in the Japanese gastric cancer treatment guidelines. Gastric Cancer 17, 206–212 (2014). https://doi.org/10.1007/s10120-013-0299-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-013-0299-x