Abstract
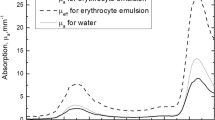
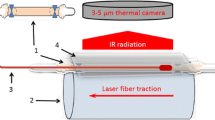
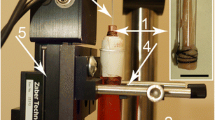
Endovenous laser ablation (EVLA) is successfully used to treat varicose veins. However, the exact working mechanism is still not fully identified and the clinical procedure is not yet standardized. Mathematical modeling of EVLA could strongly improve our understanding of the influence of the various EVLA processes. The aim of this study is to combine Mordon's optical-thermal model with the presence of a strongly absorbing carbonized blood layer on the fiber tip. The model anatomy includes a cylindrically symmetric blood vessel surrounded by an infinite homogenous perivenous tissue. The optical fiber is located in the center of the vessel and is withdrawn with a pullback velocity. The fiber tip includes a small layer of strongly absorbing material, representing the layer of carbonized blood, which absorbs 45 % of the emitted laser power. Heat transfer due to boiling bubbles is taken into account by increasing the heat conduction coefficient by a factor of 200 for temperatures above 95 °C. The temperature distribution in the blood, vessel wall, and surrounding medium is calculated from a numerical solution of the bioheat equation. The simulations were performed in MATLAB™ and validated with the aid of an analytical solution. The simulations showed, first, that laser wavelength did virtually not influence the simulated temperature profiles in blood and vessel wall, and, second, that temperatures of the carbonized blood layer varied slightly, from 952 to 1,104 °C. Our improved mathematical optical-thermal EVLA model confirmed previous predictions and experimental outcomes that laser wavelength is not an important EVLA parameter and that the fiber tip reaches exceedingly high temperatures.





Similar content being viewed by others
References
Weiss RA (2002) Comparison of endovenous radiofrequency versus 810 nm diode laser occlusion of large veins in an animal model. Dermatol Surg 28:56–61
Zimmet S, Min RJ (2003) Temperature changes in perivenous tissue during endovenous laser treatment in a swine model. J Vasc Interv Radiol 14:911–915
Fan C-M, Anderson RR (2008) Endovenous laser ablation: mechanism of action. Phlebology 23:206–213
Disselhoff BCVM, Rem AI, Verdaasdonk RM, der Kinderen DJ, Moll FL (2008) Endovenous laser ablation: an experimental study on the mechanism of action. Phlebology 23:69–76
van den Bos R, van Ruijven PW, van der Geld CW, van Gemert MJ, Neumann HA, Nijsten T (2012) Endovenous simulated laser experiments at 940 and 1,470 nm suggest wavelength independent temperature profiles. Eur J Vasc Endovasc Surg 44:77–81
Vuylsteke ME, Mordon SR (2012) Endovenous laser ablation: a review of mechanisms of action. Ann Vasc Surg 26:424–433
Van Gemert MJC, van derGeld CWM, Bruijninckx CMA, Verdaasdonk RM, Neumann HAM (2012) Comment to Vuylsteke ME and Mordon SR. Endovenous laser ablation: a review of mechanisms of action, Ann Vasc Surg 26:424–433. Ann Vasc Surg 2012; 26:881–883
Mordon SR, Wassmer B, Zemmouri J (2007) Mathematical modeling of 980 and 1,320-nm endovenous laser treatment. Lasers Surg Med 39:256–265
Meissner OA, Schmedt C-G, Hunger K, Hetterich H, Sroka R, Rieber J, Babaryka G, Steckmeier BM, Reiser M, Siebert U, Mueller-Lisse U (2007) Endovascular optical coherence tomography ex vivo: venous wall anatomy and tissue alterations after endovenous therapy. Eur Radiol 17:2384–2393
Verdaasdonk RM, Holstege FC, Jansen ED, Borst C (1991) Temperature along the surface of modified fiber tips for Nd:YAG laser angioplasty. Lasers Surg Med 11:213–222
van den Bos RR, Kockaert MA, Neumann HAM, Bremmer RH, Nijsten T, van Gemert MJC (2009) Heat conduction from the very hot fiber tip contributes to endovenous laser ablation of varicose veins. Lasers Med Sci 24:247–251, Erratum 2009; 24:679
Amzayyb M, van den Bos RR, Kodach VM, de Bruin DM, Nijsten T, Neumann HAM, van Gemert MJC (2010) Carbonized blood deposited on fibers during 810, 940, and 1,470 nm endovenous laser ablation: thickness and absorption by optical coherence tomography. Lasers Med Sci 25:439–447
Star WM (2011) Diffusion theory of light transport. In Welch AJ and van Gemert MJC (eds) Optical-thermal response of laser-irradiated tissue. 2nd edition. Springer, Dordrecht, The Netherlands, Chapter 6, Equation (6.104), page 183
Kuenstner JT, Norris KH (1994) Spectrophotometry of human hemoglobin in the near infrared region from 1,000 to 2,500 nm. J Near Infrared Spectrosc 2:59–65
Carslaw HS, Jaeger JC (1986) Conduction of heat in solids, 2nd edition, reprint. Clarendon, Oxford
Nogotov EF (1978) Applications of numerical heat transfer. McGraw-Hill, New York
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
van Ruijven, P.W.M., Poluektova, A.A., van Gemert, M.J.C. et al. Optical-thermal mathematical model for endovenous laser ablation of varicose veins. Lasers Med Sci 29, 431–439 (2014). https://doi.org/10.1007/s10103-013-1451-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-013-1451-x