Abstract
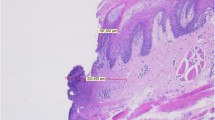
The aim of this study was to evaluate and compare the healing process after surgical treatment of chemically induced lesions in the lateral edge of tongue of hamsters performed with scalpel, electrocautery, carbon dioxide (CO2) laser radiation or neodymium:yttrium–aluminum–garnet (Nd:YAG) laser radiation. Eighty hamsters of both sexes were used and examined at postoperative days 7, 14, 21 and 28 by histological and histomorphometric analysis of the skeletal muscle fibers. In the histological analysis it was observed that the dynamics of the healing process was faster in the group treated by scalpel than in the other groups. The histomorphometric observation of the skeletal muscle fibers was submitted to one-way analysis of variance (ANOVA) and Tukey’s multiple comparison test, with a level of significance set at P < 0.05, which showed that the amount of skeletal muscle fiber formed had significantly increased in the group treated by scalpel in comparison with that in the groups treated by electrocautery (P < 0.01), CO2 laser irradiation (P < 0.001) and Nd:YAG laser irradiation (P < 0.01) on the 14th postoperative day. A gradual increase in skeletal muscle fibers formed during the healing process was observed in all groups. When the laser irradiated groups were compared, it was possible to conclude that tissue organization and vascularization were faster and more intense in the Nd:YAG laser irradiated group than in the CO2 laser irradiated group.






Similar content being viewed by others
References
Cotran RS, Kumar V, Robbins SL (1999) Robbins: Patologia estrutural e funcional, 6th edn. Guanabara Koogan, Rio de Janeiro
Li J, Chen J, Kirsner R (2007) Pathophysiology of acute wound healing. Clin Dermatol 25:9–18
Romanos G, Siar CH, Ng K, Toh CG (1999) A preliminary study of healing of superpulsed carbon dioxide laser incisions in the hard palate of monkeys. Lasers Surg Med 24:368–374
Morosolli ARC, Schubert MM, Niccoli-Filho W (2006) Surgical treatment of erythroleukoplakia in lower lip with carbon dioxide laser radiation. Lasers Med Sci 21:181–184
Deppe H, Horch HH (2007) Current status of laser applications in oral cranio-maxillofacial surgery. Med Laser Appl 22:39–42
Rossmann JA, Gottlieb S, Koudelka BM, McQuade MJ (1987) Effects of CO2 laser irradiation on gingiva. J Periodontol 58:423–425
Myers TD, Myers WD, Stone RM (1989) First soft tissue study utilizing a pulsed Nd:YAG dental laser. North West Dent 68:14–17
Romanos GE, Pelekanos S, Strub JR (1995) Effects of Nd:YAG laser on wound healing processes: clinical and immunohistochemical findings in rat skin. Lasers Surg Med 16:368–379
Frame JW (2003) Recent progress with the CO2 laser in oral surgery. Int Congr Ser 1248:3–7
Cantatore J, Kriegel D (2004) Laser surgery: an approach to the pediatric patient. J Am Dermatol 50:165–184
Sinha VK, Gallagher LA (2003) Effects of steel scalpel, ultrasonic scalpel, CO2 laser, and monopolar and bipolar electrosurgery on wound healing in guinea pig oral mucosa. Laryngoscope 113:228–236
Camacho-Alonso F, López-Jornet P (2007) Clinical-pathologic study of the healing of wounds provoked on the dorso-lingual mucosa in 186 albino rats. Otolaryngol Head Neck Surg 136:119–124
Gomes MF, Anjos MJS, Nogueira TO, Catanzaro-Guimarães SA (2002) Autogenous demineralized dentin matrix for tissue engineering applications: radiographic and histomorphometric studies. Int J Oral Maxillofac Implants 17:488–497
Masaki M, Obara K, Suzuki S, Orikasa K, Mitsuhashi H, Iwasaki K, et al (1990) The destructive effects of sclerosant ethanolamine oleate on mammalian vessel endothelium. Gastroenterol Jpn 25:230–235
Fisher SE, Frame JW, Browne RM, Trante RM (1983) A comparative histological study of wound healing following CO2 laser and conventional surgical excision of canine buccal mucosa. Arch Oral Biol 28:287–291
Pogrel MA (1989) The carbon dioxide laser in soft tissue preprosthetic surgery. J Prosthetic Dent 61:203–208
Luomanen M, Lehto VP, Meurman JH (1988) Myofibroblasts in healing laser wounds of rat tongue mucosa. Arch Oral Biol 33:17–23
Walsh LJ (1996) Pulpal temperature changes during low-power had-tissue CO2 laser procedures. Braz Dent J 7:5–11
Friesen LR, Cobb CM, Rappley JW, Forgas-Brockman L, Spencer P (1999) Laser irradiation of bone: II. Healing response following treatment by CO2 and Nd:YAG lasers. J Periodontol 70:75–83
Paes-Junior TA, Niccoli-Filho W (2001) Clinical comparison between conventional suture and vaporization with carbon dioxide laser in rat’s skin. J Clin Laser Med Surg 19:319–324
Thuaksuban N, Nuntanaranont T (2003) A comparative study of postoperative pain using carbon dioxide laser and scalpel in maxillofacial soft tissue surgery. Int Congress Series 1248:377–381
Horch HH, Deppe H (2005) New aspects of lasers in oral and craniomaxillofacial surgery. Med Laser Appl 20:7–11
Evrard L, Nammour S, Dourov N (1996) Scanning electron microscopic and immunocytochemical studies of contraction during secondary CO2 laser wound healing in rat tongue mucosa. J Oral Pathol Med 25:72–77
Kardos TB, Holt T, Ferguson MM (1989) Histological evaluation of the effect of a miniature carbon dioxide laser on oral mucosa. Int J Maxillofac Surg 18:117–120
Fortune DS, Huang S, Soto J, Pennington B, Ossof RH, Reinisch L (1998) Effect of pulse duration on wound healing using a CO2 laser. Laryngoscope 108:843–848
Acknowledgments
Financial support for this study was received from the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) (protocol number 141535/2006-7).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Morosolli, A.R.C., Veeck, E.B., Niccoli-Filho, W. et al. Healing process after surgical treatment with scalpel, electrocautery and laser radiation: histomorphologic and histomorphometric analysis. Lasers Med Sci 25, 93–100 (2010). https://doi.org/10.1007/s10103-009-0674-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-009-0674-3