Abstract
The purpose of this investigation was to analyze the burden of respiratory syncytial virus (RSV)-related hospitalizations in infants and children with congenital heart disease (CHD) over three consecutive RSV seasons. Retrospectively, all children with hemodynamically significant (HS-CHD) and not significant (HNS-CHD) CHD born between 2004 and 2008 at a tertiary care university hospital and identified by ICD-10 diagnoses were included. Data on RSV-related hospitalizations over the first three years of life covering at least three RSV seasons (November–April) were analyzed. The overall incidence of RSV-related hospitalization was 9.6 % (58/602), without a statistically significant difference between HS-CHD and HNS-CHD (7.3 % vs. 10.4 %; p = 0.258). Recommendation of palivizumab prophylaxis did not influence the RSV hospitalization rates between groups. Patients with HS-CHD and early surgery were significantly less often hospitalized due to RSV compared to those with delayed surgery (1.3 % vs. 14.3 %; p = 0.003). The median duration of hospitalization was 8.5 days (HS-CHD: 14 vs. HNS-CHD: 7 days; p = 0.003). Thirteen patients (22.4 %) were admitted to the intensive care unit (ICU), for a median of 10 days. The median age at admission was 2 months, with a significant difference between HS-CHD and HNS-CHD (6 vs. 2 months; p = 0.001). The majority (97 %) of RSV-related hospitalizations occurred before 12 months of age. Patients with HS-CHD had a significantly more severe course of RSV disease and were older at the time of hospitalization. Early surgery seemed to significantly reduce the risk of RSV hospitalization during the first RSV season.
Similar content being viewed by others
Introduction
The importance of respiratory syncytial virus (RSV)-associated lower respiratory tract infection (LRTI) in infants and children diagnosed as having congenital heart disease (CHD) is well documented [1–12]. In a recent review, children with CHD had a mean RSV hospitalization rate of 7.8 % (range 1.4–16.4 %) and a mean mortality rate of 7.3 % (range 0–37 %) [13]. RSV-related morbidity in infants and children with CHD has been reported in detail by Altman et al. in 2000 [14]. RSV infection resulted in delayed cardiac surgery in 35 %, admission to the intensive care unit (ICU) in 25 %, with an average duration of stay of 9.7 ± 8.8 days, and mechanical ventilation in 11 %, with an average treatment duration of 13.0 ± 6.4 days. Patients with pulmonary hypertension required longer ventilator support, had more costly RSV-related hospitalizations, and tended to have longer ICU stays. There is a lot of controversy regarding the use of palivizumab in high-risk infants like young children with CHD due to the high costs of the product [13].
Currently, no data on RSV-related hospitalizations in infants and children diagnosed as having CHD in Austria exist. Therefore, we aimed to analyze the burden of RSV-related hospitalizations in infants and children with CHD over three consecutive RSV seasons.
Materials and methods
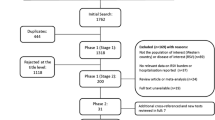
Retrospectively, all children with a diagnosis of CHD and birth between January 1, 2004 and December 31, 2008, who were treated at the Department of Pediatrics of the Medical University of Graz, a tertiary care center in the southern part of Austria, were included for analysis. Patient charts were identified using a search for International Classification of Diseases (ICD), Tenth Revision.
Children were all followed over three consecutive RSV seasons from November to April according to long-term epidemiologic data from Austria [15]. Exclusion criteria were as follows: death during the study period, admission for heart surgery solely, lost to follow-up during the first three years of life, and closure of a patent ductus arteriosus during the neonatal period. Data were collected regarding gender, date of birth, gestational age, birth weight, small for gestation age (defined as birth weight below the 10th percentile), and prescription of palivizumab prophylaxis as documented in the medical charts and according to the Austrian recommendations for RSV immune prophylaxis in infants and children with CHD [16].
CHD was classified as being hemodynamically significant (HS-CHD) or hemodynamically not significant (HNS-CHD) according to the definition of the pediatric cardiologists (M.K. and A.G.). CHD was additionally classified as cyanotic or acyanotic, and the presence of pulmonary hypertension was documented.
RSV hospitalization was defined as hospitalization associated with LRTI and a positive RSV test result. RSV testing was performed from nasopharyngeal aspirates using RSV-ELISA (Directigen EZ RSV test, Becton Dickinson, USA; sensitivity 66.7–87.2 %; specificity 85.5–91.6 %).
Data were collected regarding days of hospitalization due to respiratory illness, age at admission in months, month of RSV hospitalization, days of oxygen requirement, days at the ICU, and days of respiratory support (either nasal continuous positive airway pressure or mechanical ventilation). The severity of LRTI was measured using the lower respiratory infection (LRI) score [17].
Statistical analysis
Statistical analysis was performed using LibreOffice Calc and SPSS. Interval-scaled and normally distributed characteristics were analyzed using Student’s t-test. The Mann–Whitney U-test was used in ordinal-scaled or interval-scaled data, after checking the normality assumption with the Kolmogorov–Smirnov test. Dichotomous data were analyzed using the χ2 test. If expected values were too low, Fisher’s exact test was used. Statistical significance was set at p < 0.05.
Results
The study population comprised 602 out of 798 screened children, of whom 451 (74.9 %) had HNS-CHD, and 102 (16.9 %) had acyanotic and 49 (8.1 %) cyanotic HS-CHD. Pulmonary hypertension was diagnosed in 48 of 151 children (31.8 %) with HS-CHD.
Data of the study population and rates of RSV-related hospitalizations are shown in Table 1.
A total of 58 of the 602 children (9.6 %) were readmitted due to RSV infection. Hospitalization rates between HS-CHD (11 of 151; 7.3 %) and HNS-CHD (47 of 451; 10.4 %) did not differ significantly (p = 0.258).
The median length of RSV-related hospitalization was 8.5 days (range 1–70). Twenty-nine children (50 %) required supplemental oxygen therapy. The median duration of supplemental oxygen was 1 day (range 0–38 days). Thirteen children (22.4 %) had to be treated at the ICU. The median length of stay at the ICU was 10 days (range 2–70 days) and the median duration of mechanical ventilation was 4 days (range 0–38 days). The median LRI score was 3 (range 2–5). The median age at admission was 2 months (range 0–26 months).
Data on RSV-related hospitalization comparing children with HS-CHD to HNS-CHD are given in Table 2. Four of 11 children with HS-CHD had cyanosis and five of them had pulmonary hypertension. Two children (3.4 %) died (having had HS-CHD). No death was attributed to RSV infection; one was related to underlying VACTERL syndrome with severe trachea-bronchomalacia and the other to atrioventricular blocking following heart surgery.
The seasonal distribution showed a peak in January, with 15 of 58 (25.9 %) RSV-related hospitalizations. Forty of 58 children (69 %) were hospitalized during the typical RSV season, and 38 (65.5 %) within the first RSV season. Eighteen children (31 %) were hospitalized outside the typical RSV season, nine before the first and nine between the first and second RSV seasons (see Fig. 1).
Recommendation of palivizumab prophylaxis was documented in 41 children (27.2 %) with HS-CHD and 10 children (2.2 %) with HNS-CHD. Three of the children with HS-CHD (7.3 %) were hospitalized due to RSV infection compared to 8 of 110 (7.3 %) without recommendation (differences not significant). Children with HS-CHD and early heart surgery were, independent of palivizumab recommendation, significantly less often hospitalized due to RSV compared to those with delayed heart surgery (1.3 % vs. 14.3 %; p = 0.003).
Discussion
The burden of RSV disease in children with CHD measured by RSV-related hospitalization rates was high, with an overall rate of 9.6 % that increased up to 16.3 % in children without heart surgery before the first RSV season and having no documented palivizumab recommendation compared to the literature [1–12, 18]. As found in most of these studies, our results confirmed the more severe course of RSV disease in children with HS-CHD [1, 2, 5, 6, 18]. Interestingly, prematurity did not significantly alter the course of RSV disease in our study cohort, despite the fact that prematurity was evident in one-third of our study children, thus being significantly higher than the 16.4 % rate reported by a Spanish study group [18]. The duration of RSV-related hospital and ICU stays (median 14 and 10 days, respectively) were found to be higher compared to the Spanish data (median 7 and 6 days, respectively) [18].
Children with HNS-CHD were significantly younger of age compared to those with HS-CHD, and RSV hospitalization rates were astonishingly high (up to 11.7 %). Children with diagnosis of HNS-CHD suffer a substantial burden of RSV disease that seems to be underestimated and underreported in the literature, as far as most studies focused on HS-CHD. A very recent study found an RSV hospitalization rate of only 1.5 % in infants with HNS-CHD compared to 2.1 % in infants with acyanotic HS-CHD and 4.8 % in those with cyanotic HS-CHD, respectively [12]. ICU admission rates and need for ventilator support were high, especially in cyanotic HS-CHD, and, overall, comparable to our findings [12]. Risk factors that may exacerbate the adverse effects of respiratory disease in young CHD patients include compromised cardiorespiratory status at baseline, altered pulmonary mechanics, potential cyanosis, and/or pulmonary hypertension and ventilation–perfusion mismatch, and it is this precarious cardiorespiratory baseline that produces increased risk from RSV LRTI [19].
The weighted mean RSV case fatality rate was reported to be 1.2 % among preterm infants, 5.2 % among children with CHD, and 4.1 % among children with bronchopulmonary dysplasia [20]. We found no RSV-attributed mortality, in contrast to most other studies [1–6, 9–12].
The influence of palivizumab on RSV on rates of RSV hospitalizations and the course of disease were found to be low, but our results are limited by the fact that its evaluation was only based on the documentation of palivizumab recommendation in the medical charts and that national recommendations for the use of palivizumab in children with CHD [16] were relatively new during the study period. Cohen et al. reported RSV hospitalization rates of 1.6 % and 2.6 % in acyanotic and cyanotic CHD, respectively [21]. Nevertheless, rates increase significantly by inadequate palivizumab prophylaxis and have been reported to increase from 3.3 % to 7.9 % in one study [18].
The seasonality of RSV hospitalizations was typically peaking in January and comparable to peaks observed in preterm born infants of Austria [15]. Interestingly, a high proportion of RSV hospitalizations, namely more than 30 %, were documented occurring outside the typical RSV season between November and April. Follow-up over three consecutive RSV seasons clearly documented that the highest burden of RSV disease (97 % of all hospitalizations) happened during the first year of life. The second and third RSV seasons showed negligible rates of RSV hospitalizations.
Our findings support only partly the new and restrictive recommendations for the use of palivizumab in children with HS-CHD recently published by the American Academy of Pediatrics [22]. In this statement, children with HS-CHD who might most likely benefit from immunoprophylaxis include either those with acyanotic heart disease receiving medication to control congestive heart failure and requiring cardiac surgical procedures or infants with moderate to severe pulmonary hypertension. The latter is no longer supported by our findings, representing a high rate of RSV hospitalizations in children without evidence of pulmonary hypertension or cyanosis. Efforts are needed in order to improve the mandatory compliance and adherence to palivizumab prophylaxis for infants with HS-CHD and age younger than 12 months at onset of the RSV season in order to yield an effective reduction of the burden of RSV disease in this population.
There are certain limitations of this study that need to be noted. This is a retrospective study performed in a single-center analysis that included patients enrolled over a long period of time and the interpretation of palivizumab prophylaxis results was based solely on medical charts’ recommendations. On the other hand, the single-center experience presented here includes homogeneous follow-up data due to the geographical catchment area.
In conclusion, the burden of RSV measured by hospitalization rates was high for both HS-CHD and HNS-CHD, with a more severe course of disease in children with HS-CHD. Early surgery seemed to significantly reduce the risk of RSV hospitalization during the first RSV season, and nearly all RSV-related hospitalizations occurred during the first year of life.
References
MacDonald NE, Hall CB, Suffin SC, Alexson C, Harris PJ, Manning JA (1982) Respiratory syncytial viral infection in infants with congenital heart disease. N Engl J Med 307:397–400
Moler FW, Khan AS, Meliones JN, Custer JR, Palmisano J, Shope TC (1992) Respiratory syncytial virus morbidity and mortality estimates in congenital heart disease patients: a recent experience. Crit Care Med 20:1406–1413
Navas L, Wang E, de Carvalho V, Robinson J (1992) Improved outcome of respiratory syncytial virus infection in a high-risk hospitalized population of Canadian children. Pediatric Investigators Collaborative Network on Infections in Canada. J Pediatr 121:348–354
Wang EE, Law BJ, Stephens D (1995) Pediatric Investigators Collaborative Network on Infections in Canada (PICNIC) prospective study of risk factors and outcomes in patients hospitalized with respiratory syncytial viral lower respiratory tract infection. J Pediatr 126:212–219
Simoes EA, Sondheimer HM, Top FH Jr, Meissner HC, Welliver RC, Kramer AA, Groothuis JR (1998) Respiratory syncytial virus immune globulin for prophylaxis against respiratory syncytial virus disease in infants and children with congenital heart disease. The Cardiac Study Group. J Pediatr 133:492–499
Feltes TF, Cabalka AK, Meissner HC, Piazza FM, Carlin DA, Top FH Jr, Connor EM, Sondheimer HM; Cardiac Synagis Study Group (2003) Palivizumab prophylaxis reduces hospitalization due to respiratory syncytial virus in young children with hemodynamically significant congenital heart disease. J Pediatr 143:532–540
Kristensen K, Stensballe LG, Bjerre J, Roth D, Fisker N, Kongstad T, Svendsen AL, Nielsen BW (2009) Risk factors for respiratory syncytial virus hospitalisation in children with heart disease. Arch Dis Child 94:785–789
Kristensen K, Hjuler T, Ravn H, Simões EA, Stensballe LG (2012) Chronic diseases, chromosomal abnormalities, and congenital malformations as risk factors for respiratory syncytial virus hospitalization: a population-based cohort study. Clin Infect Dis 54:810–817
Meberg A, Bruu AL (2006) Respiratory syncytial virus infections in congenital heart defects—hospitalizations and costs. Acta Paediatr 95:404–406
Simon A, Müller A, Khurana K, Engelhart S, Exner M, Schildgen O, Eis-Hübinger AM, Kamin W, Schaible T, Wadas K, Ammann RA, Wilkesmann A; DSM RSV Paed Study Group (2008) Nosocomial infection: a risk factor for a complicated course in children with respiratory syncytial virus infection—results from a prospective multicenter German surveillance study. Int J Hyg Environ Health 211:241–250
Duppenthaler A, Ammann RA, Gorgievski-Hrisoho M, Pfammatter JP, Aebi C (2004) Low incidence of respiratory syncytial virus hospitalisations in haemodynamically significant congenital heart disease. Arch Dis Child 89:961–965
Chiu SN, Shao PL, Chen HC, Lin MT, Huang LM, Kao FY, Huang SK, Wang JK, Wu MH (2016) Risk of respiratory syncytial virus infection in cyanotic congenital heart disease in a subtropical area. J Pediatr 171:25–30.e1. doi:10.1016/j.jpeds.2015.12.029
Resch B, Michel-Behnke I (2013) Respiratory syncytial virus infections in infants and children with congenital heart disease: update on the evidence of prevention with palivizumab. Curr Opin Cardiol 28:85–91
Altman CA, Englund JA, Demmler G, Drescher KL, Alexander MA, Watrin C, Feltes TF (2000) Respiratory syncytial virus in patients with congenital heart disease: a contemporary look at epidemiology and success of preoperative screening. Pediatr Cardiol 21:433–438
Resch B, Sommer C, Nuijten MJ, Seidinger S, Walter E, Schoellbauer V, Mueller WD (2012) Cost-effectiveness of palivizumab for respiratory syncytial virus infection in high-risk children, based on long-term epidemiologic data from Austria. Pediatr Infect Dis J 31:e1–e8
Pinter M, Geiger R (2005) Recommendations for RSV immune prophylaxis in infants and children with congenital heart disease (in German). Monatsschr Kinderheilkd 153:878–880
Groothuis JR, Simoes EAF, Levin MJ, Hall CB, Long CE, Rodriguez WJ, Arrobio J, Meissner HC, Fulton DR, Welliver RC, Tristram DA, Siber GR, Prince GA, van Raden M, Hemming VG (1993) Prophylactic administration of respiratory syncytial virus immune globulin to high-risk infants and young children. The Respiratory Syncytial Virus Immune Globulin Study Group. N Engl J Med 329:1524–1530
Medrano López C, García-Guereta L; CIVIC Study Group (2010) Community-acquired respiratory infections in young children with congenital heart diseases in the palivizumab era: the Spanish 4-season civic epidemiologic study. Pediatr Infect Dis J 29:1077–1082
Cabalka AK (2004) Physiologic risk factors for respiratory viral infections and immunoprophylaxis for respiratory syncytial virus in young children with congenital heart disease. Pediatr Infect Dis J 23(1 Suppl):S41–S45
Szabo SM, Gooch KL, Bibby MM, Vo PG, Mitchell I, Bradt P, Levy AR (2013) The risk of mortality among young children hospitalized for severe respiratory syncytial virus infection. Paediatr Respir Rev 13(Suppl 2):S1–S8
Cohen SA, Zanni R, Cohen A, Harrington M, VanVeldhuisen P, Boron ML; Palivizumab Outcomes Registry Group (2008) Palivizumab use in subjects with congenital heart disease: results from the 2000–2004 Palivizumab Outcomes Registry. Pediatr Cardiol 29:382–387
American Academy of Pediatrics Committee on Infectious Diseases; American Academy of Pediatrics Bronchiolitis Guidelines Committee (2014) Updated guidance for palivizumab prophylaxis among infants and young children at increased risk of hospitalization for respiratory syncytial virus infection. Pediatrics 134:415–420
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Funding
None.
Ethical approval
By the Ethics Committee of the Medical University of Graz, number 26-391 ex 13/14.
Informed consent
Not applicable due to the retrospective design of the study.
Rights and permissions
About this article
Cite this article
Resch, B., Kurath-Koller, S., Hahn, J. et al. Respiratory syncytial virus-associated hospitalizations over three consecutive seasons in children with congenital heart disease. Eur J Clin Microbiol Infect Dis 35, 1165–1169 (2016). https://doi.org/10.1007/s10096-016-2649-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-016-2649-1