Abstract
Background
Developments in inguinal hernia surgery have substantially lowered recurrence rates, yet recurrences remain an important outcome parameter of inguinal hernia repair. The aim of this study was to analyze the characteristics of all reoperated groins after endoscopic totally extraperitoneal (TEP) inguinal hernia repair in a high-volume hernia clinic in the Netherlands.
Methods
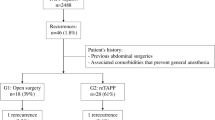
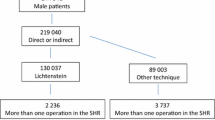
All groins with recurrence-like symptoms reoperated after previous TEP inguinal hernia repair between January 2006 and December 2016 were analyzed. Patient characteristics, imaging findings, primary hernia type, time to recurrence and recurrence type were assessed.
Results
A total of 137 groins were reoperated in 130 patients. The median age at the TEP procedure was 55 years [interquartile range (IQR) 45–64 years]. Fifty-seven groins were initially part of a bilateral procedure (42%). Median time until recurrence was 9 months (IQR 4–26 months). Reoperation findings were a hernia recurrence in 76%, an isolated lipoma in 18%, and no recurrence or lipoma in 6%. The majority of hernias recurred at their initial site (70%), of which the greatest part involved direct hernias. Isolated lipomas were more frequently seen after indirect hernia repair.
Conclusions
Inguinal hernia recurrences were still observed in this high-volume hernia clinic. Recurrences were most frequently seen at their initial hernia site, the majority involving direct hernias. Isolated lipomas presenting as a pseudorecurrence were most frequently seen after correction of indirect hernias. In accordance with the current guidelines, reducing recurrence rates can be achieved by mesh fixation in bilateral, large and direct defects and by thoroughly reducing lipomas.

Similar content being viewed by others
References
Read RC (2009) Herniology: past, present, and future. Hernia 13:577–580
Campanelli G, Canziani M, Frattini F et al (2008) Inguinal hernia: state of the art. Int J Surg 6(S1):S26–S28
Nathan JD, Pappas TN (2003) An old condition with new solutions. Ann Surg 238(S6):S148–S157
Kukleta JF (2006) Causes of recurrence in laparoscopic inguinal hernia repair. J Minim Access Surg 2(3):187–191
Read RC (2011) Crucial steps in the evolution of the preperitoneal approaches to the groin: an historical review. Hernia 15(1):1–5
McCormack K, Wake BL, Fraser C et al (2005) Trans abdominal pre-peritoneal (TAPP) versus totally extraperitoneal (TEP) laparoscopic techniques for inguinal hernia repair: a systematic review. Hernia 9(2):109–114
Simons MP, Aufenacker T, Bay-Nielsen M et al (2009) European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 13(4):343–403
Miserez M, Peeters E, Aufenacker T et al (2014) Update with level 1 studies of the European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 18(2):151–163
HerniaSurge Group (2018) International guidelines for groin hernia management. Hernia 22(1):1–165
Bittner R, Arregui ME, Bisgaard T et al (2011) Guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia [International Endohernia Society (IEHS)]. Surg Endosc 25(9):2773–2843
Bittner R, Montgomery MA, Arregui E et al (2015) Update of guidelines on laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia (International Endohernia Society). Surg Endosc Other Interv Tech 29(2):289–321
Liem MSL, van der Graaf Y, van Steensel CJ et al (1997) Comparison of conventional anterior surgery and laparoscopic surgery for inguinal hernia repair. N Engl J Med 336:1541–1547
O’Reilly EA, Burke JP, O’Connell PR (2012) A meta-analysis of surgical morbidity and recurrence after laparoscopic and open repair of primary unilateral inguinal hernia. Ann Surg 255(5):846–853
Langeveld HR, Van‘t Riet M, Weidema WF et al (2010) Total extraperitoneal inguinal hernia repair compared with Lichtenstein (the LEVEL-trial): a randomized controlled trial. Ann Surg 251:819–824
Burcharth J, Andresen K, Pommergaard HC et al (2014) Recurrence patterns of direct and indirect inguinal hernias in a nationwide population in Denmark. Surgery 155(1):173–177
Sevonius D, Gunnarsson U, Nordin P et al (2011) Recurrent groin hernia surgery. Br J Surg 98(10):1489–1494
Scheuerlein H, Schiller A, Schneider C et al (2003) Totally extraperitoneal repair of recurrent inguinal hernia: results from 179 consecutive patients. Surg Endosc Other Interv Tech 17(7):1072–1076
Kockerling F, Jacob D, Wiegank W et al (2016) Endoscopic repair of primary versus recurrent male unilateral inguinal hernias:are there differences in the outcome? Surg Endosc 30(3):1146–1155
Burgmans JP, Voorbrood CE, Simmermacher RK et al (2016) Long-term results of a randomized double-blinded prospective trial of a lightweight (Ultrapro) versus a heavyweight mesh (Prolene) in laparoscopic total extraperitoneal inguinal hernia repair (TULP-trial). Ann Surg 263(5):862–866
Roos MM, Bakker WJ, Schouten N et al (2018) Higher recurrence rate after endoscopic totally extraperitoneal (TEP) inguinal hernia repair with Ultrapro lightweight mesh. Ann Surg 268(2):241–246
Neumayer L, Giobbie-Hurder A, Jonasson O et al (2004) Open mesh versus laparoscopic mesh repair of inguinal hernia. N Engl J Med 350(18):1819–1827
Schouten N, Simmermacher RK, van Dalen T et al (2013) Is there an end of the “learning curve” of endoscopic totally extraperitoneal (TEP) hernia repair? Surg Endosc 27(3):789–794
Lamb ADG, Robson AJ, Nixon SJ (2006) Recurrence after totally extraperitoneal laparoscopic repair: implications for operative technique and surgical training. Surgeon 4(5):299–307
Felix E, Scott S, Crafton B et al (1998) Causes of recurrence after laparoscopic hernioplasty—a multicenter study. Surg Endosc 12:226–231
Miserez M, Alexandre JH, Campanelli G et al (2007) The European hernia society groin hernia classification: simple and easy to remember. Hernia 11(2):113–116
Liem MSL, Van Duyn EB, Van der Graaf Y et al (2003) Recurrences after conventional anterior and laparoscopic inguinal hernia repair: a randomized comparison. Ann Surg 237:136–141
Lau H, Loong F, Yuen WK et al (2007) Management of herniated retroperitoneal adipose tissue during endoscopic extraperitoneal inguinal hernioplasty. Surg Endosc 21(9):1612–1616
Nasr AO, Tormey S, Walsh TN (2005) Lipoma of the cord and round ligament: an overlooked diagnosis?. Hernia 9(3):245–247
Shpitz B, Kuriansky J, Werener M et al (2004) Early postoperative evaluation of groins after laparoscopic total extraperitoneal repair of inguinal hernias. J Laparoendosc Adv Surg Tech A 14(6):353–357
Young J, Gilbert AI, Graham MF (2007) The use of ultrasound in the diagnosis of abdominal wall hernias. Hernia 11(4):347–351
Funding
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
MR declares no conflict of interest. CvH declares no conflict of interest. EV declares no conflict of interest. GC declares no conflict of interest. PD declares no conflict of interest. CV declares no conflict of interest. RS declares no conflict of interest. JB declares no conflict of interest.
Ethical approval
This study design is in accordance with ethical standards. Institutional Review Board approval was obtained.
Human and animal rights
This article does not contain any studies with animal subjects.
Informed consent
For this type of study informed consent is not required.
Rights and permissions
About this article
Cite this article
Roos, M.M., van Hessen, C.V., Verleisdonk, E.J.M.M. et al. An 11-year analysis of reoperated groins after endoscopic totally extraperitoneal (TEP) inguinal hernia repair in a high volume hernia center. Hernia 23, 655–662 (2019). https://doi.org/10.1007/s10029-018-1827-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-018-1827-8