Abstract
Background
We performed this study to compare the safety and feasibility of single-incision laparoscopic cholecystectomy (SILC) with conventional multiple-port laparoscopic cholecystectomy (MPLC).
Methods
We searched PubMed, Embase, Web of Science, the Cochrane Controlled Register of Trials (CENTRAL), and ClinicalTrials.gov for randomized controlled trials comparing SILC versus MPLC. We evaluated the pooled outcomes for complications, pain scores, and surgery-related events. This study was performed in accordance with PRISMA guidelines.
Results
A total of 48 randomized controlled trials involving 2838 patients in the SILC group and 2956 patients in the MPLC group were included in this study. Our results showed that SILC was associated with a higher incidence of incisional hernia (relative risk = 2.51; 95% confidence interval = 1.23–5.12; p = 0.01) and longer operation time (mean difference = 15.27 min; 95% confidence interval = 9.67–20.87; p < 0.00001). There were no significant differences between SILC and MPLC regarding bile duct injury, bile leakage, wound infection, conversion to open surgery, retained common bile duct stones, total complication rate, and estimated blood loss. No difference was observed in postoperative pain assessed by a visual analogue scale between the two groups at four time points (6 h, 8 h, 12 h, and 24 h postprocedure).
Conclusions
Based on the current evidence, SILC did not result in better outcomes compared with MPLC and both were equivalent regarding complications. Considering the additional surgical technology and longer operation time, SILC should be chosen with careful consideration.
Similar content being viewed by others
Laparoscopic cholecystectomy is the gold-standard surgical procedure for treating benign gallbladder diseases and was first reported in 1985 [1]. In conventional laparoscopic cholecystectomy, three or four ports are used. However, increasing patients demand for less invasive and cosmetic, the first single-incision laparoscopic cholecystectomy was reported in 1997 [2] and multiple studies using the technique have since been published. Recently, more literature became available for the feasibility of SILC [3, 4]. Some studies suggested that single-incision laparoscopic cholecystectomy (SILC) might be associated with less postoperative pain, better aesthetic results, and shorter recovery time [5,6,7,8]. Recently studies and meta-analysis showed that SILC is a safe procedure with postoperative outcome similar to that of standard LC [8,9,10]. However, SILC is still not in widespread use because of its longer operation time, greater technical difficulty, and a possible significant increase in complication rates [8, 11,12,13]. Several studies have compared SILC and multiport laparoscopic cholecystectomy (MPLC); however, definitive conclusions from these comparisons remain controversial. Meta-analyses have also been performed to compare SILC with MPLC regarding related events [9, 14,15,16], but findings are inconsistent. More recent studies evaluated only the technical considerations of SILC [14, 17, 18]. Therefore, a study is needed to evaluate recent randomized controlled trials (RCTs). To evaluate the safety and feasibility of SILC versus MPLC, we performed a meta-analysis to compare SILC with conventional MPLC (three- or four-port) using recently-published RCTs.
Methods
Inclusion and exclusion criteria
The search criteria included all studies comparing SILC and MPLC published in English with full texts. We included recent studies published by the same authors or agency. We excluded articles with insufficient data on outcome measures (study enrolled only 1 treatment method; data could not be used for statistical analysis and reported less one of the outcomes) and any studies evaluating miniport laparoscopic cholecystectomy (any trocar < 5 mm in size).
Search strategy
We searched PubMed, Embase, Web of Science, the Cochrane Controlled Register of Trials (CENTRAL) and ClinicalTrials.gov up to 1 May 2019. MPLC was defined as conventional laparoscopic cholecystectomy using three or four ports. English search terms included, but were not limited to, the following: “single incision,” “single port,” “single access,” “multiport,” “standard,” “conventional,” and “laparoscopic cholecystectomy”. The references of articles identified after the initial search were also manually reviewed.
Outcome measures
The outcomes measures included bile duct injury (BDI), bile leakage, wound infection, incisional hernia, conversion to open cholecystectomy, total complication rate, operating time, estimated blood loss volume, and postoperative pain score assessed by a visual analogue scale at four time points (4 h, 6 h, 8 h, 12 h, and 24 h postprocedure).
Data extraction
Two reviewers independently extracted the original data from the literature to ensure homogeneity of the extracted data. The standardized selection form included the first author, year of publication, country in which the study was performed, and general data. Conflicts in data abstraction were resolved by consensus and by referring to the original article. Extracted data were entered into a pregenerated standard Microsoft Excel file (Microsoft Corporation, Redmond, WA, USA).
IRB approval and informed consent were not needed for this study.
Risk of bias assessment
We used the Cochrane Collaboration Handbook [19] to evaluate the quality of included studies. Disagreement, if any, was resolved by discussion.
Statistical analysis
All statistical analyses were performed using Review Manager (RevMan) version 5.3 software (Cochrane Informatics and Knowledge Management Department, London, UK). Summary outcomes are described as proportions and 95% confidence intervals (CI) for categorical data and weighted mean difference ± standard deviation for continuous data. Publication bias was evaluated using the χ2 test and funnel plots. Heterogeneity among studies was evaluated using the χ2 test. A two-tailed p value of < 0.05 was considered statistically significant. We also assessed the potential for publication bias through a visual inspection of funnel plot asymmetry. This meta-analysis was performed according to the PRISMA statement guidelines.
Results
Study selection and characteristics of the trials
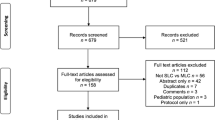
Using the search strategy, the initial research yielded 1049 studies; 201 studies were identified after eliminating duplicates. Another 595 studies were excluded after reviewing the titles and abstracts. Finally, 48 RCTs were included in this meta-analysis [3, 4, 7, 10, 14, 18, 20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61]. A total of 5654 included patients were divided into an SILC group of 2769 patients and an MPLC group of 2885 patients. The sample size in the studies ranged from 33 to 600 patients and involved 19 countries. A detailed flowchart of the selection process following the PRISMA template is shown in Fig. 1. The characteristics of the included studies are shown in Table 1.
Methodological quality and risk of bias
The methodological quality of the included studies was evaluated by two reviewers using the Cochrane Collaboration tool for assessing the risk of bias. An overall summary of the methodological quality of the included studies is shown in Fig. 2.
Outcome measures
BDI
The incidence of BDI was reported in 25 studies. BDI was identified in 6/1563 patients in the SILC group and 5/1665 patients in the MPLC group. The risk ratio of BDI in SILC versus MPLC was 1.15 (95% CI 0.42–3.19, p = 0.78) (Fig. 3).
Bile leakage
Bile leakage was identified in 20 studies. The incidence of bile leakage tended to be higher in the SILC group (13/1407 patients) than in the MPLC group (10/1284 patients), although the difference was not statistically significant (relative risk (RR): 1.08; 95% CI 0.5–2.31; p = 0.85) (Fig. 4).
Wound infection
Twenty-four studies reported wound infection and we found no significant difference between the two groups (RR: 1.05; 95% CI 0.67–1.66; p = 0.82) (Fig. 5).
Incisional hernia
Incisional hernia was reported in 35 studies and occurred in 29/2208 patients in the SILC group and in 7/2304 patients in the MPLC group. The pooled data for the meta-analysis showed that SILC may be associated with higher incisional hernia rates compared with MPLC (RR: 2.51; 95% CI 1.23–5.12; p = 0.01) (Fig. 6A). A subgroup analysis showed no significant difference in the incidence of postoperative hernia in the single-incision subgroup (RR: 0.65; 95% CI 0.03–16.44; p = 0.79) (Fig. 6B) and that SILC was associated with a higher incidence of incisional hernia compared with MPLC in the single-port subgroup (RR: 2.97; 95% CI 1.46–6.03 p = 0.003) (Fig. 6C).
Conversion to open cholecystectomy
Twenty studies reported conversion to open cholecystectomy and we found no significant difference between SILC and MPLC (RR: 0.94; 95% CI 0.47–1.88; p = 0.85; Fig. 7).
Retained common bile duct stones
Twelve studies reported retained common bile duct stones and we found no significant difference between the two groups using a fixed-effects model (RR: 1.23; 95% CI 0.45–3.39; p = 0.69) (Fig. 8).
Total complications
We found no significant difference in total complication rates between the two groups (RR: 1.50; 95% CI 0.58–3.87; p = 0.41) (Fig. 9).
Operation time
Operation time was reported in 27 studies. Compared with MPLC, SILC had a longer operation time and the difference was significant compared with MPLC (mean difference: 15.27 min; 95% CI 9.67–20.87; p < 0.00001) (Fig. 10).
Estimated blood loss
Eleven trials reported estimated blood loss volumes. The pooled results showed that there was no significant difference between the SILC group and the MPLC group (mean difference: 1.35 ml; 95% CI − 0.02–2.71; p = 0.05) (Fig. 11).
Postoperative pain assessed using a visual analogue scale (VAS)
Postoperative pain was estimated at four time points after laparoscopic cholecystectomy (6 h, 8 h, 12 h, and 24 h) using a VAS. SILC appeared to provide no better pain score than for MPLC in each of the four time subgroups (p = 0.50, p = 0.44, p = 0.54 and p = 0.66, respectively; Fig. 12).
Publication bias
Most graphical funnel plots of the parameters were symmetrical and Egger’s test revealed no significant publication bias.
Discussion
This current meta-analysis of RCTs showed that SILC was associated with a higher incidence of incisional hernia and longer operation time. There was no significant difference between SILC and MPLC groups regarding BDI, bile leakage, wound infection, conversion to open cholecystectomy, or total complication rates. No difference was observed in postoperative pain assessed by VAS between the two groups 6 h, 8 h, 12 h, and 24 h postprocedure.
Laparoscopic cholecystectomy has become the gold-standard procedure for benign gallbladder disease. In conventional laparoscopic cholecystectomy, three or four ports are usually used. Previous studies have demonstrated that conventional laparoscopic cholecystectomy is safe and feasible for cholecystectomy [62]; however, to reduce postoperative pain and improve cosmetic results, SILC was introduced in 1997 [2]. Today, SILC and MPLC are the main approaches for laparoscopic cholecystectomy [63,64,65,66]. RCTs and meta-analyses have compared SILC with MPLC, but results are controversial.
The results of our review showed that SILC may be associated with a higher incidence of incisional hernia, as reported in several previous studies [15, 41, 67]. The size of the SILC incision is larger than that for MPLC, which may lead to a higher incidence of incisional hernia. Additionally, incision-related events, namely wound infection, seroma, and hematoma, may be associated with postoperative incisional hernia. Interestingly, many studies, including ours, showed no difference in the incidence of postoperative wound infections between the two groups, which indicates that in SILC, wound infection is not the only factor influencing postoperative incisional hernia rates. Some studies focusing on this topic have claimed that a larger fascial defect may increase the risk of incisional hernia [41, 68, 69]. The approach used in SILC includes a single skin incision or a specific port. Our subgroup analysis showed no significant difference in the incidence of postoperative incisional hernias in the single skin incision subgroup. However, SILC was associated with higher incisional hernia rates compared with MPLC in the single-port subgroup. A study performed by Chuang et al. published in 2016 demonstrated that multiple trocars through a single skin incision may decrease the incidence of hernia [70]. The studies included in the meta-analysis could not provide complete data in terms of port size and the SILS ports used in the included studies were different. However, whether SILC increases the incidence of postoperative incisional hernia remains inconclusive. Many factors may affect the incidence of hernia [35, 71, 72]. Most studies included in this meta-analysis provided the data of BMI which showed no difference between two groups. Interestingly, in the study by Marks et al. [41], there was a difference in BMI between the two groups, and there was a difference in the incidence of postoperative hernias between the two groups. However, multivariate analysis showed that BMI was not associated with postoperative hernia. A short follow-up time may underestimate the incidence of incisional hernia, which may occur years after the procedure. The follow-up time in our included studies ranged from 1 to 17 months, which was short, when assessing the occurrence of incisional hernia. Large-scale trials with > 30 months’ follow-up demonstrated no difference between the two groups [73]; however, higher numbers of high-quality studies with longer follow-ups are required.
Postoperative pain is a main point of comparison between SILC and MPLC. In contrast to some previous meta-analyses [15, 67], our current study showed no significant difference between SILC and MPLC; findings for this comparison are controversial. Two studies performed by Bucher et al. [25] and Tsimoyianni et al. [47] showed that SILC has an advantage over MPLC regarding pain; however, findings for postoperative pain in recent studies differ considerably. The incision length, use of different anesthetics, pneumoperitoneal pressure, patients’ psychological factors and the methods used to assess pain could contribute to heterogeneity in our included studies [15]. Regarding aesthetic results, assessment time points and methods differed in the included studies, although most reports documented better aesthetic results after SILC [25, 74, 75]. Arezzo et al. demonstrated that SILC was associated with better aesthetic results; however, results had high overall heterogeneity across the included studies. More high-quality RCTs focused on patients’ postoperative pain and aesthetic results are needed.
SILC and MPLC had a similar rate of postoperative complication, namely, BDI, bile leakage and retained common bile duct stones. BDI is a major concern in laparoscopic cholecystectomy. In the current meta-analysis, we found no significant difference in the incidence of BDI and bile leakage, similar to findings in previous studies. Regarding retained common bile duct stones, we found no significant difference between SILC and MPLC; however, in some studies, routine cholangiography was performed during surgery [21, 76], so the rate of retained common bile duct stones differed in the included studies.
Consistent with previous studies, operation time was significantly longer for patients undergoing SILC, which involves an unnaturally ergonomic technique for surgeons. However, with continuous developments in SILC technology and greater experience, this difference has gradually narrowed. A recent RCT performed by Umemura et al. showed no significant difference between SILC and MPLC regarding operation time [17]; however, the learning curves for SILC are longer than for MPLC and SILC requires more surgical experience.
Although our meta-analysis incorporated several of the latest RCTs, certain limitations must be mentioned. First, several trials in the present study had a high risk of bias and outcomes following SILC and MPLC may have been over- or underestimated. Second, the criteria describing intraoperative and postoperative complications were inconsistent. Third, we included studies published only in English. Considering these limitations, more large-scale, high-quality RCTs are required.
Conclusions
Based on the current evidence, SILC did not result in better outcomes compared with MPLC and both were equivalent regarding complications. Considering the additional surgical technology and longer operation time, SILC should be chosen with careful consideration.
Data availability
All the data used in the study can be obtained from the original articles.
References
Muhe E (1991) [Laparoscopic cholecystectomy–late results]. Langenbecks Archiv fur Chirurgie Supplement Kongressband Deutsche Gesellschaft fur Chirurgie Kongress. Springer, Berlin, pp 416–423
Navarra G, Pozza E, Occhionorelli S, Carcoforo P, Donini I (1997) One-wound laparoscopic cholecystectomy. Br J Surg 84:695
Arezzo A, Passera R, Bullano A, Mintz Y, Kedar A, Boni L, Cassinotti E, Rosati R, Fumagalli Romario U, Sorrentino M, Brizzolari M, Di Lorenzo N, Gaspari AL, Andreone D, De Stefani E, Navarra G, Lazzara S, Degiuli M, Shishin K, Khatkov I, Kazakov I, Schrittwieser R, Carus T, Corradi A, Sitzman G, Lacy A, Uranues S, Szold A, Morino M (2017) Multi-port versus single-port cholecystectomy: results of a multi-centre, randomised controlled trial (MUSIC trial). Surg Endosc 31:2872–2880
Zheng M, Qin M, Zhao H (2012) Laparoendoscopic single-site cholecystectomy: a randomized controlled study. Minim Invasive Ther Allied Technol MITAT 21:113–117
Joseph S, Moore BT, Sorensen GB, Earley JW, Tang F, Jones P, Brown KM (2011) Single-incision laparoscopic cholecystectomy: a comparison with the gold standard. Surg Endosc 25:3008–3015
Hauters P, Meunier D, Urgyan S, Jouret JC, Janssen P, Nys JM (1996) Prospective controlled study comparing laparoscopy and the Shouldice technique in the treatment of unilateral inguinal hernia. Ann Chir 50:776–781
Solomon D, Shariff AH, Silasi DA, Duffy AJ, Bell RL, Roberts KE (2012) Transvaginal cholecystectomy versus single-incision laparoscopic cholecystectomy versus four-port laparoscopic cholecystectomy: a prospective cohort study. Surg Endosc 26:2823–2827
Markar SR, Karthikesalingam A, Thrumurthy S, Muirhead L, Kinross J, Paraskeva P (2012) Single-incision laparoscopic surgery (SILS) vs. conventional multiport cholecystectomy: systematic review and meta-analysis. Surg Endosc 26:1205–1213
Sinan H, Saydam M, Demir P, Ozer MT, Demirbas S (2019) Comparison of single-incision and conventional laparoscopic cholecystectomy in terms of quality of life, body image, and cosmesis. Niger J Clin Pract 22:521–526
Qu JW, Xin C, Wang GY, Yuan ZQ, Li KW (2019) Feasibility and safety of single-incision laparoscopic cholecystectomy versus conventional laparoscopic cholecystectomy in an ambulatory setting. Hepatobiliary Pancreat Dis Int 18:273–277
Allemann P, Schafer M, Demartines N (2010) Critical appraisal of single port access cholecystectomy. Br J Surg 97:1476–1480
Joseph M, Phillips MR, Farrell TM, Rupp CC (2012) Single incision laparoscopic cholecystectomy is associated with a higher bile duct injury rate: a review and a word of caution. Ann Surg 256:1–6
Garg P, Thakur JD, Garg M, Menon GR (2012) Single-incision laparoscopic cholecystectomy vs. conventional laparoscopic cholecystectomy: a meta-analysis of randomized controlled trials. J Gastrointest Surg 16:1618–1628
Omar MA, Redwan AA, Mahmoud AG (2017) Single-incision versus 3-port laparoscopic cholecystectomy in symptomatic gallstones: a prospective randomized study. Surgery 162:96–103
Haueter R, Schutz T, Raptis DA, Clavien PA, Zuber M (2017) Meta-analysis of single-port versus conventional laparoscopic cholecystectomy comparing body image and cosmesis. Br J Surg 104:1141–1159
Evers L, Bouvy N, Branje D, Peeters A (2017) Single-incision laparoscopic cholecystectomy versus conventional four-port laparoscopic cholecystectomy: a systematic review and meta-analysis. Surg Endosc 31:3437–3448
Umemura A, Suto T, Nakamura S, Fujiwara H, Endo F, Nitta H, Takahara T, Sasaki A (2019) Comparison of Single-incision laparoscopic cholecystectomy versus needlescopic cholecystectomy: a single institutional randomized clinical trial. Dig Surg 36:53–58
Zhao L, Wang Z, Xu J, Wei Y, Guan Y, Liu C, Xu L, Liu C, Wu B (2016) A randomized controlled trial comparing single-incision laparoscopic cholecystectomy using a novel instrument to that using a common instrument. Int J Surg (London, England) 32:174–178
Higgins J, Green SE (2011) Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration (eds) Naunyn-Schmiedebergs Archiv für experimentelle Pathologie und Pharmakologie 5, pp S38
Abd Ellatif ME, Askar WA, Abbas AE, Noaman N, Negm A, El-Morsy G, El Nakeeb A, Magdy A, Amin M (2013) Quality-of-life measures after single-access versus conventional laparoscopic cholecystectomy: a prospective randomized study. Surg Endosc 27:1896–1906
Aprea G, Coppola Bottazzi E, Guida F, Masone S, Persico G (2011) Laparoendoscopic single site (LESS) versus classic video-laparoscopic cholecystectomy: a randomized prospective study. J Surg Res 166:e109–e112
Bingener J, Skaran P, McConico A, Novotny P, Wettstein P, Sletten DM, Park M, Low P, Sloan J (2015) A double-blinded randomized trial to compare the effectiveness of minimally invasive procedures using patient-reported outcomes. J Am Coll Surg 221:111–121
Borle FR, Mehra B, Ranjan Singh A (2015) Comparison of cosmetic outcome between single-incision laparoscopic cholecystectomy and conventional laparoscopic cholecystectomy in rural Indian population: a randomized clinical trial. Indian J Surg 77:877–880
Brown KM, Moore BT, Sorensen GB, Boettger CH, Tang F, Jones PG, Margolin DJ (2013) Patient-reported outcomes after single-incision versus traditional laparoscopic cholecystectomy: a randomized prospective trial. Surg Endosc 27:3108–3115
Bucher P, Pugin F, Buchs NC, Ostermann S, Morel P (2011) Randomized clinical trial of laparoendoscopic single-site versus conventional laparoscopic cholecystectomy. Br J Surg 98:1695–1702
Chang SK, Wang YL, Shen L, Iyer SG, Madhavan K (2015) A randomized controlled trial comparing post-operative pain in single-incision laparoscopic cholecystectomy versus conventional laparoscopic cholecystectomy. World J Surg 39:897–904
Deveci U, Barbaros U, Kapakli MS, Manukyan MN, Simsek S, Kebudi A, Mercan S (2013) The comparison of single incision laparoscopic cholecystectomy and three port laparoscopic cholecystectomy: prospective randomized study. J Korean Surg Soc 85:275–282
Guo W, Liu Y, Han W, Liu J, Jin L, Li JS, Zhang ZT (2015) Randomized trial of immediate postoperative pain following single-incision versus traditional laparoscopic cholecystectomy. Chin Med J 128:3310–3316
Hajong R, Hajong D, Natung T, Anand M, Sharma G (2016) A comparative study of single incision versus conventional four ports laparoscopic cholecystectomy. J Clin Diagn Res 10:PC06–PC09
He GL, Jiang ZS, Cheng Y, Lai QB, Zhou CJ, Liu HY, Gao Y, Pan MX, Jian ZX (2015) Tripartite comparison of single-incision and conventional laparoscopy in cholecystectomy: a multicenter trial. World J Gastrointest Endosc 7:540–546
Ito E, Takai A, Imai Y, Otani H, Onishi Y, Yamamoto Y, Ogawa K, Tohyama T, Fukuhara S, Takada Y (2019) Quality of life after single-incision laparoscopic cholecystectomy: a randomized, clinical trial. Surgery 165:353–359
Jorgensen LN, Rosenberg J, Al-Tayar H, Assaadzadeh S, Helgstrand F, Bisgaard T (2014) Randomized clinical trial of single-versus multi-incision laparoscopic cholecystectomy. Br J Surg 101:347–355
Justo-Janeiro JM, Vincent GT, Vazquez de Lara F, de la Rosa Paredes R, Orozco EP, Vazquez de Lara LG (2014) One, two, or three ports in laparoscopic cholecystectomy? Int Surg 99:739–744
Khorgami Z, Shoar S, Anbara T, Soroush A, Nasiri S, Movafegh A, Aminian A (2014) A randomized clinical trial comparing 4-port, 3-port, and single-incision laparoscopic cholecystectomy. J Investig Surg 27:147–154
Lai EC, Yang GP, Tang CN, Yih PC, Chan OC, Li MK (2011) Prospective randomized comparative study of single incision laparoscopic cholecystectomy versus conventional four-port laparoscopic cholecystectomy. Am J Surg 202:254–258
Lirici MM, Califano AD, Angelini P, Corcione F (2011) Laparo-endoscopic single site cholecystectomy versus standard laparoscopic cholecystectomy: results of a pilot randomized trial. Am J Surg 202:45–52
Luna RA, Nogueira DB, Varela PS, Rodrigues Neto Ede O, Norton MJ, Ribeiro Ldo C, Peixoto AM, de Mendonca YL, Bendet I, Fiorelli RA, Dolan JP (2013) A prospective, randomized comparison of pain, inflammatory response, and short-term outcomes between single port and laparoscopic cholecystectomy. Surg Endosc 27:1254–1259
Lurje G, Raptis DA, Steinemann DC, Amygdalos I, Kambakamba P, Petrowsky H, Lesurtel M, Zehnder A, Wyss R, Clavien PA, Breitenstein S (2015) Cosmesis and body image in patients undergoing single-port versus conventional laparoscopic cholecystectomy: a multicenter double-blinded randomized controlled trial (SPOCC-trial). Ann Surg 262:728–734 (discussion 734–725)
Ma J, Cassera MA, Spaun GO, Hammill CW, Hansen PD, Aliabadi-Wahle S (2011) Randomized controlled trial comparing single-port laparoscopic cholecystectomy and four-port laparoscopic cholecystectomy. Ann Surg 254:22–27
Madureira FA, Manso JE, Madureira Filho D, Iglesias AC (2014) Inflammation in laparoendoscopic single-site surgery versus laparoscopic cholecystectomy. Surg Innov 21:263–268
Marks JM, Phillips MS, Tacchino R, Roberts K, Onders R, DeNoto G, Gecelter G, Rubach E, Rivas H, Islam A, Soper N, Paraskeva P, Rosemurgy A, Ross S, Shah S (2013) Single-incision laparoscopic cholecystectomy is associated with improved cosmesis scoring at the cost of significantly higher hernia rates: 1-year results of a prospective randomized, multicenter, single-blinded trial of traditional multiport laparoscopic cholecystectomy vs single-incision laparoscopic cholecystectomy. J Am Coll Surg 216:1037–1047 (discussion 1047–1038)
Noguera J, Tejada S, Tortajada C, Sanchez A, Munoz J (2013) Prospective, randomized clinical trial comparing the use of a single-port device with that of a flexible endoscope with no other device for transumbilical cholecystectomy: LLATZER-FSIS pilot study. Surg Endosc 27:4284–4290
Ostlie DJ, Juang OO, Iqbal CW, Sharp SW, Snyder CL, Andrews WS, Sharp RJ, Holcomb GW 3rd, St Peter SD (2013) Single incision versus standard 4-port laparoscopic cholecystectomy: a prospective randomized trial. J Pediatr Surg 48:209–214
Pan MX, Jiang ZS, Cheng Y, Xu XP, Zhang Z, Qin JS, He GL, Xu TC, Zhou CJ, Liu HY, Gao Y (2013) Single-incision vs three-port laparoscopic cholecystectomy: prospective randomized study. World J Gastroenterol 19:394–398
Partelli S, Barugola G, Sartori A, Crippa S, Falconi M, Ruffo G (2016) Single-incision laparoscopic cholecystectomy versus traditional laparoscopic cholecystectomy performed by a single surgeon: findings of a randomized trial. Surg Today 46:313–318
Sulu B, Yildiz BD, Ilingi ED, Gunerhan Y, Cakmur H, Anuk T, Yildiz B, Koksal N (2015) Single port vs. four port cholecystectomy-randomized trial on quality of life. Adv Clin Exp Med 24:469–473
Tsimoyiannis EC, Tsimogiannis KE, Pappas-Gogos G, Farantos C, Benetatos N, Mavridou P, Manataki A (2010) Different pain scores in single transumbilical incision laparoscopic cholecystectomy versus classic laparoscopic cholecystectomy: a randomized controlled trial. Surg Endosc 24:1842–1848
Yilmaz H, Arun O, Apiliogullari S, Acar F, Alptekin H, Calisir A, Sahin M (2013) Effect of laparoscopic cholecystectomy techniques on postoperative pain: a prospective randomized study. J Korean Surg Soc 85:149–153
Zapf M, Yetasook A, Leung D, Salabat R, Denham W, Barrera E, Butt Z, Carbray J, Du H, Wang CE, Ujiki M (2013) Single-incision results in similar pain and quality of life scores compared with multi-incision laparoscopic cholecystectomy: a blinded prospective randomized trial of 100 patients. Surgery 154:662–670 (discussion 670–661)
Kumar S, Ahmad Z (2019) Single port laparoscopic cholecystectomy compared to the standard laparoscopic cholecystectomy. Int Surg J 2019(6):4
Cao ZG, Cai W, Qin MF, Zhao HZ, Yue P, Li Y (2011) Randomized clinical trial of single-incision versus conventional laparoscopic cholecystectomy: short-term operative outcomes. Surg Laparosc Endosc Percutan Tech 21:311–313
Rasic Z, Schwarz D, Nesek VA, Zoricic I, Sever M, Rasic D, Lojo N (2010) Single incision laparoscopic cholecystectomy–a new advantage of gallbladder surgery. Coll Antropol 34:595–598
Sasaki A, Ogawa M, Tono C, Obara S, Hosoi N, Wakabayashi G (2012) Single-port versus multiport laparoscopic cholecystectomy: a prospective randomized clinical trial. Surg Laparosc Endosc Percutan Tech 22:396–399
Sinan H, Demirbas S, Ozer MT, Sucullu I, Akyol M (2012) Single-incision laparoscopic cholecystectomy versus laparoscopic cholecystectomy: a prospective randomized study. Surg Laparosc Endosc Percutan Tech 22:12–16
Ye G, Qin Y, Xu S, Wu C, Wang S, Pan D, Wang X (2015) Comparison of transumbilical single-port laparoscopic cholecystectomy and fourth-port laparoscopic cholecystectomy. Int J Clin Exp Med 8:7746–7753
Emre Telciler K, Ilhan E, Yakan S, Cengiz F, Senlikci A, Akturk Hayat E (2014) Single-port laparoscopic cholecystectomy versus the classical four port laparoscopic cholecystectomy: a randomized prospective clinical trial. Minerva Chir 69:1–7
Goel AC, Priyanka Gupta, Kumar Atul, Gupta Shalabh, Agarwal Ayush, Bhardwaj Deepak, Mishra Rajneesh Kumar, Fronek Jiri P J (2016) Comparative study of single-incision laparoscopic cholecystectomy with four-port conventional laparoscopic cholecystectomy: a single-center experience. World J Lap Surg 9:9–12
Ashok Koirala RS, Thakur Dipendra, Agrawal Sunit, Chaudhary Bhuwan Lal, Poudel Sagar (2019) Comparative study of single incision laparoscopic cholecystectomy with standard four port laparoscopic cholecystectomy for symptomatic cholelithiasis. JKISTMC 1:10–15
FAHAD RIZWI MS, KHALID JAVED ABID (2014) Outcome of single incision laparoscopic cholecystectomy (SILC) versus conventional four port laparoscopic cholecystectomy for cholelithiasis—a randomized control trial. PJMHS 8:243–246
Dabbagh N, Soroosh A, Khorgami Z, Shojaeifard A, Jafari M, Abdehgah AG, Mahmudzade H (2015) Single-incision laparoscopic cholecystectomy versus mini-laparoscopic cholecystectomy: a randomized clinical trial study. J Res Med Sci 20:1153–1159
Tyagi S, Sinha R, Tyagi A (2017) Single incision laparoscopic cholecystectomy: less scar, less pain. J Minim Access Surg 13:118–123
Keus F, de Jong JA, Gooszen HG, van Laarhoven CJ (2006) Laparoscopic versus small-incision cholecystectomy for patients with symptomatic cholecystolithiasis. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD006229
Romanelli JR, Roshek TB 3rd, Lynn DC, Earle DB (2010) Single-port laparoscopic cholecystectomy: initial experience. Surg Endosc 24:1374–1379
Podolsky ER, Rottman SJ, Poblete H, King SA, Curcillo PG (2009) Single port access (SPA) cholecystectomy: a completely transumbilical approach. J Laparoendosc Adv Surg Tech A 19:219–222
Kimura T (1998) Laparoscopic cholecystectomy using fine-caliber instruments. Surg Endosc 12:1449
Reardon PR, Kamelgard JI, Applebaum B, Rossman L, Brunicardi FC (1999) Feasibility of laparoscopic cholecystectomy with miniaturized instrumentation in 50 consecutive cases. World J Surg 23:128–131 (discussion 131–122)
Geng L, Sun C, Bai J (2013) Single incision versus conventional laparoscopic cholecystectomy outcomes: a meta-analysis of randomized controlled trials. PLoS ONE 8:e76530
Milas M, Devedija S, Trkulja V (2014) Single incision versus standard multiport laparoscopic cholecystectomy: up-dated systematic review and meta-analysis of randomized trials. Surgeon 12:271–289
Tamini N, Rota M, Bolzonaro E, Nespoli L, Nespoli A, Valsecchi MG, Gianotti L (2014) Single-incision versus standard multiple-incision laparoscopic cholecystectomy: a meta-analysis of experimental and observational studies. Surg Innov 21:528–545
Chuang SH, Lin CS (2016) Single-incision laparoscopic surgery for biliary tract disease. World J Gastroenterol 22:736–747
Canes D, Desai MM, Aron M, Haber GP, Goel RK, Stein RJ, Kaouk JH, Gill IS (2008) Transumbilical single-port surgery: evolution and current status. Eur Urol 54:1020–1029
Gurusamy K, Junnarkar S, Farouk M, Davidson BR (2008) Meta-analysis of randomized controlled trials on the safety and effectiveness of day-case laparoscopic cholecystectomy. Br J Surg 95:161–168
Pasley WHSC (2013) Long-term follow-up shows no difference in port-site hernia incidence: single incision vs. traditional laparoscopic cholecystectomy. Surg Endosc 27:482
Lee PC, Lo C, Lai PS, Chang JJ, Huang SJ, Lin MT, Lee PH (2010) Randomized clinical trial of single-incision laparoscopic cholecystectomy versus minilaparoscopic cholecystectomy. Br J Surg 97:1007–1012
Kilian M, Raue W, Menenakos C, Wassersleben B, Hartmann J (2011) Transvaginal-hybrid vs. single-port-access vs. ‘conventional’ laparoscopic cholecystectomy: a prospective observational study. Langenbecks Arch Surg 396:709–715
Bresadola F, Pasqualucci A, Donini A, Chiarandini P, Anania G, Terrosu G, Sistu MA, Pasetto A (1999) Elective transumbilical compared with standard laparoscopic cholecystectomy. Eur J Surg 165:29–34
Acknowledgements
We thank Jane Charbonneau, DVM from Liwen Bianji, Edanz Group China (www.liwenbianji.cn/ac) for editing the English text of a draft of this manuscript.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Yunxiao Lyu, Yunxiao Cheng, Bin Wang, Sicong Zhao, and Liang Chen have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lyu, Y., Cheng, Y., Wang, B. et al. Single-incision versus conventional multiport laparoscopic cholecystectomy: a current meta-analysis of randomized controlled trials. Surg Endosc 34, 4315–4329 (2020). https://doi.org/10.1007/s00464-019-07198-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07198-8