Abstract
Background
Controversy exists as to what constitutes a learning curve to achieve competency, and how the initial learning period of robotic thoracic surgery should be approached.
Methods
We conducted a systematic review of the literature published prior to December 2018 using PubMed/MEDLINE for studies of surgeons adopting the robotic approach for anatomic lung resection or thymectomy. Changes in operating room time and outcomes based on number of cases performed, type of procedure, and existing proficiency with video-assisted thoracoscopic surgery (VATS) were examined.
Results
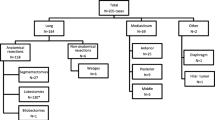
Twelve observational studies were analyzed, including nine studies on robotic lung resection and three studies on thymectomy. All studies showed a reduction in operative time with an increasing number of cases performed. A steep learning curve was described for thymectomy, with a decrease in operating room time in the first 15 cases and a plateau after 15–20 cases. For anatomic lung resection, the number of cases to achieve a plateau in operative time ranged between 15–20 cases and 40–60 cases. All but two studies had at least some VATS experience. Six studies reported on experience of over one hundred cases and showed continued gradual improvements in operating room time.
Conclusion
The learning curve for robotic thoracic surgery appears to be rapid with most studies indicating the steepest improvement in operating time occurring in the initial 15–20 cases for thymectomy and 20–40 cases for anatomic lung resection. Existing data can guide a standardized robotic curriculum for rapid adaptation, and aid credentialing and quality monitoring for robotic thoracic surgery programs.

Similar content being viewed by others
References
Long H et al (2018) Thoracoscopic versus thoracotomy for lung cancer: short-term outcomes of a randomized trial. Ann Thorac Surg 105(2):386–392
Bendixen M et al (2019) Cost-utility analysis of minimally invasive surgery for lung cancer: a randomized controlled trial. Eur J Cardiothorac Surg. https://doi.org/10.1093/ejcts/ezz064
Demmy T et al (2018) Oncologic equivalence of minimally invasive lobectomy: the scientific and practical arguments. Ann Thorac Surg 106(2):609–617
Baldonado J et al (2018) Credentialing for robotic lobectomy: what is the learning curve? A retrospective analysis of 272 cases by a single surgeon. J Robot Surg. https://doi.org/10.1007/s11701-018-00902-1
Rajaram R et al (2017) Nationwide assessment of robotic lobectomy for non-small cell lung cancer. Ann Thorac Surg 103(4):1092–1100
Wei B, Eldaif S, Cerfolio R (2016) Robotic lung resection for non-small cell lung cancer. Surg Oncol Clin N Am 25(3):515–531
Veronesi G (2015) Robotic lobectomy and segmentectomy for lung cancer: results and operating technique. J Thorac Dis 7:122–130
Hernandez J et al (2012) Robotic lobectomy: flattening the learning curve. J Robot Surg 6(1):41–45
Gallagher SP et al (2018) Learning curve of robotic lobectomy for early stage non-small cell lung cancer by a thoracic surgeon adept in open lobectomy. Innovations 13(5):321–327
Stewart L et al (2015) Preferred reporting items for systematic review and meta-analyses of individual participant data. JAMA 313:1657–1665
Downs S, Black N (1998) The feasibility of creating a checklist for the assessment of the methodological quality both of randomized and non-randomized studies of health care interventions. J Epidemiol Community Health 52:377–384
Fahim C et al (2017) Robotic-assisted thoracoscopic surgery for lung resection: the first Canadian series. Can J Surg 60(4):260–265
Huang P et al (2014) Experience with the “da Vinci” robotic system for early-stage thymomas: report of 23 cases. Thorac Cancer 5(4):325–329
Ro C et al (2006) Three-year experience with totally endoscopic robotic thymectomy. Innovations 1(3):111–114
Kamel M et al (2017) Robotic thymectomy: learning curve and associated perioperative outcomes. J Laparoendosc Adv Surg Tech 27(7):685–690
Cheufou D et al (2011) Starting a robotic program in general thoracic surgery: how, why, and lessons learned. Ann Thorac Surg 91(6):1729–1737
Veronesi G et al (2011) Experience with robotic lobectomy for lung cancer. Innovations 6(6):355–360
Meyer M et al (2012) The learning curve of robotic lobectomy. Int J Med Robot Comput Assisted Surg 8:448–452
Toker A et al (2016) Robotic anatomic lung resections: the initial learning experience and description of learning in 102 cases. Surg Endosc 30:676–683
Zhang Y et al (2018) Robotic anatomical segmentectomy: an analysis of the learning curve. Ann Thorac Surg 107(5):1515–1522
Gonsenhauser I et al (2012) Developing a multidisciplinary robotic surgery quality assessment program. J Healthc Qual 34(3):43–53
Li X, Wang J, Ferguson M (2014) Competence versus mastery: the time course for developing proficiency in video-assisted thoracoscopic lobectomy. J Thorac Cardiovasc Surg 147(4):1150–1154
Zhao H et al (2010) Video-assisted thoracoscopic surgery lobectomy for lung cancer: the learning curve. World J Surg 34(10):2368–2372
Mazzella A et al (2016) Video-assisted thoracoscopic lobectomy: which the learning curve of an experienced consultant? J Thorac Dis 8(9):2444–2453
Cerfolio R, Bryant A (2013) How to teach robotic pulmonary resection. Semin Thorac Cardiovasc Surg 25(1):76–82
Estes S et al (2017) Best practices for robotic surgery programs. JSLS 21(2):e2016.00102
Funding
This research was not solicited and did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Merritt is a speaker for intuitive Surgical. Dr. D’Souza is a Proctor for Intuitive Surgical. Drs. Power, Moffatt-Bruce, and Kneuertz have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Power, A.D., D’Souza, D.M., Moffatt-Bruce, S.D. et al. Defining the learning curve of robotic thoracic surgery: what does it take?. Surg Endosc 33, 3880–3888 (2019). https://doi.org/10.1007/s00464-019-07035-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07035-y