Abstract
Background
Although single-port laparoscopic cholecystectomy (SILC) is safe and effective, inherent surgeons’ discomfort has prevented a large-scale adaptation of this technique. Recent advances in robotic technology suggest that da Vinci Single-Site™ cholecystectomy (dVSSC) may overcome this issue by reducing the stress load of the surgeon compared to SILC. However, evidence to objectively assess differences between the two approaches is lacking.
Methods
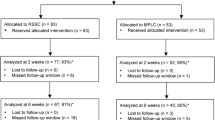
60 patients [36 women, 24 men (mean age 52 years)] with benign gallbladder disease were randomly assigned to dVSSC (n = 30) or SILC (n = 30) in this single-centre, single-blinded controlled trial. The primary endpoint was surgeon’s stress load. Secondary endpoints included operating time, conversion rates, additional trocar placement, blood loss, length of hospital stay, procedure costs, health-related quality of life, cosmesis and complications. Data were collected preoperatively, during the hospital stay, and at 1 and 12 months’ follow-up.
Results
The dVSSC group showed a significant reduction of mental stress load of the surgeon compared to SILC [Subjective Mental Effort Questionnaire (SMEQ) score: median 25.0 (range 8–89) vs. 42.5 (range 13–110) points; p = 0.002] and a trend towards reduced physical stress load [Local Experienced Discomfort (LED) score: median 8 (range 2–27) vs. 12 (range 0–64) points; p = 0.088]. The length of hospital stay was longer in the SILC group [mean 3.06 (median 2; range 1–26) vs. 1.9 (median 2; range 1–4) days, p = 0.034] but overall hospital costs were higher for dVSSC [median 9734 (range 5775–16729) vs. 6900 (range 4156–99977) CHF; p = 0.001]. There were no differences in the rate of postoperative complications that required re-intervention (Dindo–Clavien grade ≥ IIIa; SILC n = 2 vs. dVSSC n = 0, p = 0.492) or other secondary endpoints.
Conclusions
Da Vinci Single-Site™ cholecystectomy provides significant benefits over Single-Port Laparoscopic Cholecystectomy in terms of surgeon’s stress load, matches the standards of the laparoscopic single-incision approach with regard to patients’ outcomes but increases expenses. Clinicaltrials.gov registration-No.: NCT02485392.

Similar content being viewed by others
References
Buchs NC, Addeo P, Bianco FM, Gorodner V, Ayloo SM, Elli EF, Oberholzer J, Benedetti E, Giulianotti PC (2012) Perioperative risk assessment in robotic general surgery: lessons learned from 884 cases at a single institution. Arch Surg 147(8):701–708
Konstantinidis KM, Hirides P, Hirides S, Chrysocheris P, Georgiou M (2012) Cholecystectomy using a novel Single-Site((R)) robotic platform: early experience from 45 consecutive cases. Surg Endosc 26(9):2687–2694
Pietrabissa A, Sbrana F, Morelli L, Badessi F, Pugliese L, Vinci A, Klersy C, Spinoglio G (2012) Overcoming the challenges of single-incision cholecystectomy with robotic single-site technology. Arch Surg 147(8):709–714
Zhong X, Rui YY, Zhou ZG (2012) Laparoendoscopic single-site versus traditional laparoscopic surgery in patients with cholecystectomy: a meta-analysis. J Laparoendosc Adv Surg Tech A 22(5):449–455
Steinemann DC, Raptis DA, Lurje G, Oberkofler CE, Wyss R, Zehnder A, Lesurtel M, Vonlanthen R, Clavien PA, Breitenstein S (2011) Cosmesis and body image after single-port laparoscopic or conventional laparoscopic cholecystectomy: a multicenter double blinded randomised controlled trial (SPOCC-trial). BMC Surg 11:24
Lurje G, Raptis DA, Steinemann DC, Amygdalos I, Kambakamba P, Petrowsky H, Lesurtel M, Zehnder A, Wyss R, Clavien PA, Breitenstein S (2015) Cosmesis and body image in patients undergoing single-port versus conventional laparoscopic cholecystectomy: a multicenter double-blinded randomized controlled trial (SPOCC-trial). Ann Surg 262(5):728–734
van der Schatte Olivier RH, Van’t Hullenaar CD, Ruurda JP, Broeders IA (2012) Ergonomics, user comfort, and performance in standard and robot-assisted laparoscopic surgery. Surg Endosc 23(6):1365–1371
Mirbod SM, Yoshida H, Miyamoto K, Miyashita K, Inaba R, Iwata H (1995) Subjective complaints in orthopedists and general surgeons. Int Arch Occup Environ Health 67(3):179–186
Berguer R, Forkey DL, Smith WD (1999) Ergonomic problems associated with laparoscopic surgery. Surg Endosc 13(5):466–468
Albayrak A, van Veelen MA, Prins JF, Snijders CJ, de Ridder H, Kazemier G (2017) A newly designed ergonomic body support for surgeons. Surg Endosc 21(10):1835–1840
Bagrodia A, Raman JD (2009) Ergonomics considerations of radical prostatectomy: physician perspective of open, laparoscopic, and robot-assisted techniques. J Endourol/Endourol Soc 23(4):627–633
Szeto GP, Ho P, Ting AC, Poon JT, Tsang RC, Cheng SW (2010) A study of surgeons’ postural muscle activity during open, laparoscopic, and endovascular surgery. Surg Endosc 24(7):1712–1721
Grochola LF, Soll C, Zehnder A, Wyss R, Herzog P, Breitenstein S (2017) Robot-assisted single-site compared with laparoscopic single-incision cholecystectomy for benign gallbladder disease: protocol for a randomized controlled trial. BMC Surg 17(1):13
Shanafelt TD, Balch CM, Bechamps G, Russell T, Dyrbye L, Satele D, Collicott P, Novotny PJ, Sloan J, Freischlag J (2010) Burnout and medical errors among American surgeons. Ann Surg 251(6):995–1000
Boutron I, Moher D, Altman DG, Schulz KF, Ravaud P, Group C (2008) Extending the CONSORT statement to randomized trials of nonpharmacologic treatment: explanation and elaboration. Ann Intern Med 148(4):295–309
Corlett EN, Bishop RP (1976) A technique for assessing postural discomfort. Ergonomics 19(2):175–182
Eypasch E, Williams JI, Wood-Dauphinee S, Ure BM, Schmulling C, Neugebauer E, Troidl H (1995) Gastrointestinal quality of life index: development, validation and application of a new instrument. Br J Surg 82(2):216–222
Dunker MS, Stiggelbout AM, van Hogezand RA, Ringers J, Griffioen G, Bemelman WA (1998) Cosmesis and body image after laparoscopic-assisted and open ileocolic resection for Crohn’s disease. Surg Endosc 12(11):1334–1340
Francis NK, Curtis NJ, Conti JA, Foster JD, Bonjer HJ, Hanna GB, EAES committees (2018) EAES classification of intraoperative adverse events in laparoscopic surgery. Surg Endosc. https://doi.org/10.1007/s00464-018-6108-1
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Lee J, Kang SW, Jung JJ, Choi UJ, Yun JH, Nam KH, Soh EY, Chung WY (2011) Multicenter study of robotic thyroidectomy: short-term postoperative outcomes and surgeon ergonomic considerations. Ann Surg Oncol 18(9):2538–2547
Acknowledgements
The authors would like to thank Dimitri Raptis for his help with the power calculations. We would also like to express our gratitude to Nadia Braga, Angela Munson and all the administrative staff at the Cantonal Hospital of Winterthur for their invaluable administrative support. Clinicaltrials.gov registration number: NCT02485392.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Lukasz Filip Grochola, Christopher Soll, Adrian Zehnder, Roland Wyss, Pascal Herzog and Stefan Breitenstein have no conflict of interest or financial ties to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Grochola, L.F., Soll, C., Zehnder, A. et al. Robot-assisted versus laparoscopic single-incision cholecystectomy: results of a randomized controlled trial. Surg Endosc 33, 1482–1490 (2019). https://doi.org/10.1007/s00464-018-6430-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6430-7