Abstract
Background
Single-incision laparoscopic cholecystectomy evolved from the traditional multiport laparoscopic technique. Prior trials have demonstrated improved cosmesis with the single-incision technique. Robotic single-site surgery minimizes the technical difficulties associated with laparoscopic single-incision approach. This is the first prospective, randomized, controlled study comparing robotic single-site cholecystectomy (RSSC) and multiport laparoscopic cholecystectomy (MPLC) in terms of cosmesis and patient satisfaction.
Methods
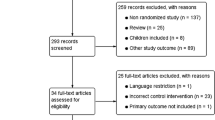
Patients with symptomatic benign gallbladder disease were randomized to RSSC or MPLC. Data included perioperative variables such as operative time, conversion and complications and cosmesis satisfaction, body image perception, quality of life using validated questionnaires, at postoperative visits of 2, 6 weeks and 3 months.
Results
One hundred thirty-six patients were randomized to RSSC (N = 83) and MPLC (N = 53) at 8 institutions. Both cohorts were dominated by higher enrollment of females (RSSC = 78%, MPLC = 92%). The RSSC and MPLC cohorts were otherwise statistically matched. Operative time was longer for RSSC (61 min vs. 44 min, P < 0.0001). There were no differences in complication rates. RSSC demonstrated a significant superiority in cosmesis satisfaction and body image perception (P value < 0.05 at every follow-up). There was no statistically significant difference in patient-reported quality of life. Multivariate analysis of female patients demonstrated significantly higher preference for RSSC over MPLC in cosmesis satisfaction and body image perception with no difference seen in overall quality of life.
Conclusions
Results from this trial show that RSSC is associated with improved cosmesis satisfaction and body image perception without a difference in observed complication rate. The uncompromised safety and the improved cosmesis satisfaction and body image perception provided by RSSC for female patients support consideration of the robotic single-site approach.
ClinicalTrials.gov identifier NCT01932216.

Similar content being viewed by others
References
Lytynski GS (1998) Erich Mühe and the rejection of laparoscopic cholecystectomy (1985): a surgeon ahead of his time. JSLS 2:341–346
Vaughan J, Gurusamy KS, Davidson BR (2013) Day-surgery versus overnight stay surgery for laparoscopic cholecystectomy. Cochrane Database Syst Rev 31(7):CD006798. doi:10.1002/14651858.CD006798.pub4
Vidal O, Valentini M, Espert JJ, Ginesta C, Jimeno J, Martinez A, Benarroch G, Garcia-Valdecasas JC (2009) Laparoendoscopic single-site cholecystectomy: a safe and reproducible alternative. J Laparoendosc Adv Surg Tech A 19(5):599–602. doi:10.1089/lap.2009.0205
Hodgett SE, Hernandez JM, Morton CA, Ross SB, Alvrink M, Rosemurgy AS (2009) Laparoendoscopic single site (LESS) cholecystectomy. J Gastrointest Surg 13(2):188–192. doi:10.1007/s11605-008-0735-0
Marks JM, Phillips MS, Tacchino R, Roberts K, Onders R, DeNoto G, Gecelter G, Rubach E, Islam A, Soper N, Paraskeva P, Rosemurgy A, Ross S, Shah S (2013) Single-incision laparoscopic cholecystectomy is associated with improved cosmesis scoring at the cost of significantly higher hernia rates: 1-year results of a prospective randomized, multicenter, single-blinded trial of traditional multiport laparoscopic cholecystectomy versus single-incision laparoscopic cholecystectomy. J Am Coll Surg 216(6):1037–1047. doi:10.1016/j.jamcollsurg.2013.02.024 (discussion 1047–1048)
Phillips MS, Marks JM, Roberts K, Tacchino R, Onders R, DeNoto Rivas H, Islam A, Soper N, Gecelter G, Rubach E, Paraskeva P, Shah S (2012) Intermediate results of a prospective randomized controlled trial of traditional four-port laparoscopic cholecystectomy versus single-incision laparoscopic cholecystectomy. Surg Endosc 26(5):1296–1303. doi:10.1007/s00464-011-2028-z
Marks J, Tacchino R, Roberts K, Onders R, DeNoto G, Paraskeva P, Rivas H, Soper N, Rosemurgy A, Shah S (2011) Prospective randomized controlled trial of traditional laparoscopic cholecystectomy versus single–incision laparoscopic cholecystectomy: report of preliminary data. Am J Surg 201(3):369–372. doi:10.1016/j.amjsurg.2010.09.012 (discussion 372–373)
Dunker MS, Stiggelbout AM, van Hogezand RA, Ringers J, Griffioen G, Bemelman WA (1998) Cosmesis and body image after laparoscopic-assisted and open ileocolic resection for Crohn’s disease. Surg Endosc 12(11):1334–1340
Bucher P, Pugin F, Buchs NC, Ostermann S, Morel P (2011) Randomized clinical trial of laparoendoscopic single-site versus conventional laparoscopic cholecystectomy. Br J Surg 98(12):1695–1702. doi:10.1002/bjs.7689
Morel P, Hagen ME, Bucher P, Buchs NC, Pugin F (2011) Robotic single–port cholecystectomy using a new platform: initial clinical experience. J Gastrointest Surg 15(12):2182–2186. doi:10.1007/s11605-011-1688-2
Buzad FA, Corne LM, Brown TC, Fagin RS, Hebert AE, Kaczmarek CA, Pack AN, Payne TN (2013) Single-site robotic cholecystectomy: efficiency and cost analysis. Int J Med Robot 9(3):365–370. doi:10.1002/rcs.1507
Morel P, Pugin F, Bucher P, Buchs NC, Hagen ME (2012) Robotic single-incision laparoscopic cholecystectomy. J Robot Surg 6(3):273–274. doi:10.1007/s11701-011-0310-7
Pietrabissa A, Sbrana F, Morelli L, Badessi F, Pugliese L, Vinci A, Klersy C, Spinoglio G (2012) Overcoming the challenges of single-incision cholecystectomy with robotic single-site technology. Arch Surg 147(8):709–714. doi:10.1001/archsurg.2012.508
Wren SM, Curet MJ (2011) Single–port robotic cholecystectomy: results from a first human use clinical study of the new da Vinci Single-Site surgical platform. Arch Surg 146(10):1122–1127. doi:10.1001/archsurg.2011.143
Pietrabissa A, Pugliese L, Vinci A, Peri A, Tinozzi FP, Cavazzi E, Pellegrino E, Klersy C (2016) Short-term outcomes of single-site robotic cholecystectomy versus four-port laparoscopic cholecystectomy: a prospective, randomized, double-blind trial. Surg Endosc. doi:10.1007/s00464-015-4601-3
Geng L, Sun C, Bai J (2013) Single incision versus conventional laparoscopic cholecystectomy outcomes: a meta-analysis of randomized controlled trials. PLoS One 8(10):e76530. doi:10.1371/journal.pone.0076530
Joseph S, Moore BT, Sorensen GB, Earley JW, Tang F, Jones P, Brown KM (2011) Single-incision laparoscopic cholecystectomy: a comparison with the gold standard. Surg Endosc 25(9):3008–3015. doi:10.1007/s00464-011-1661-x
Lai EC, Yang GP, Tang CN, Yih PC, Chan OC, Li MK (2011) Prospective randomized comparative study of single incision laparoscopic cholecystectomy versus conventional four–port laparoscopic cholecystectomy. Am J Surg 202(3):254–258. doi:10.1016/j.amjsurg.2010.12.009
Trastulli S, Cirocchi R, Desiderio J, Guarino S, Santoro A, Parisi A, Noya G, Boselli C (2013) Systematic review and meta-analysis of randomized clinical trials comparing single-incision versus conventional laparoscopic cholecystectomy. Br J Surg 100(2):191–208. doi:10.1002/bjs.8937
Gonzalez A, Hernandez Murcia C, Romero R, Escobar E, Garcia P, Walker G, Gallas M, Dickens E, McIntosh B, Norwood W, Kim K, Rabaza J, Parris D (2016) A multicenter study of initial experience with single-incision robotic cholecystectomies (SIRC) demonstrating a high success rate in 465 cases. Surg Endosc 30(7):2951–2960. doi:10.1007/s00464-015-4583-1
Spinoglio G, Lenti LM, Maglione V, Lucido FS, Priora F, Bianchi PP, Grosso F, Quarati R (2012) Single–site robotic cholecystectomy (SSRC) versus single-incision laparoscopic cholecystectomy (SILC): comparison of learning curves. First European experience. Surg Endosc 26(6):1648–1655. doi:10.1007/s00464-011-2087-1
Acknowledgements
The authors would like to thank the following independent contributors: Mimi Wainwright (Wainwright Medical Communications, Los Gatos, CA USA) for editorial support and Vijaya Bharathi Lingala, Ph.D. (Institute of Clinical Outcomes Research and Education, Woodside CA and Department of Cardiothoracic Surgery, Stanford University, Palo Alto, CA USA) for her contribution toward the statistical study design and study data analysis.
Funding
This study was sponsored and funded by Intuitive Surgical, Inc., Sunnyvale, CA, USA in association with the identified study investigators under a cooperative clinical trial agreement. The authors had full control of the study execution, analysis, and development of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
All authors received research study support from Intuitive Surgical, statistical analysis from the Institute of Clinical Outcomes Research and Education, and editorial support from Wainwright Medical Communications. Dr. Kudsi has received honoraria and research study support outside the scope of this work. Dr. Kaza is a consultant for Intuitive. Dr. Dickens is a consultant for Intuitive and has received grants from Intuitive as well as speakers bureau fees and fees to develop educational presentations. Dr. Martin receives fees as a proctor for Intuitive. Ms. Mehendale is an employee of Intuitive. Dr. Gonzalez receives consultancy fees from Ethicon Endo Surgery, Mallinkrodt Pharmaceuticals, and Minimally Invasive Devices outside the scope of this work. Omar Yusef Kudsi, Andres Castellanos, Srinivas Kaza, Justin McCarty, Eugene Dickens, David Martin, Frederick M. Tiesenga, Konstantinos Konstantinidis, Petros Hirides, Shilpa Mehendale, and Anthony Gonzalez have no other conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Kudsi, O.Y., Castellanos, A., Kaza, S. et al. Cosmesis, patient satisfaction, and quality of life after da Vinci Single-Site cholecystectomy and multiport laparoscopic cholecystectomy: short-term results from a prospective, multicenter, randomized, controlled trial. Surg Endosc 31, 3242–3250 (2017). https://doi.org/10.1007/s00464-016-5353-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-5353-4