Abstract
Background
For some common conditions, pre-operative clinic visits are often of little value to the patient or surgeon with transfer to the waiting list being predictable. In response to local patient feedback, we introduced a single hospital visit laparoscopic hernia surgery pathway with focus on informed consent, patient-reported outcomes and post-operative interaction with primary care services.
Methods
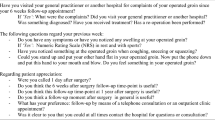
A single hospital visit service for elective hernia repairs was created. Patients were not excluded on age, BMI or co-morbidity. Following referral, patients were telephoned by a surgeon. If considered appropriate, a symptom assessment tool, procedure information and consent form were sent. All patients were operated without attending clinic or pre-operative assessment. Surgeon-led telephone follow-up was made at either 2 or 7 days post-operatively and patient satisfaction assessed at 3 months.
Results
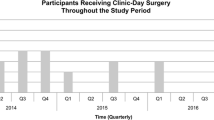
A total of 517 patients were referred for single-stop surgery between 2012 and 2015. Median age was 58 (range 20–92), 91 % were male, and mean BMI was 25.6 (17.4–52.0). No patient refused the single-visit pathway. Single-stop patients had higher knowledge questionnaire scores (mean 16 vs. 10, p = 0.01) than patients who had attended clinic. Nine (1.7 %) were requested to attend clinic to confirm diagnosis, and three (0.8 %) were cancelled by their surgeon on the operative day. A total of 393 hernia repairs (331 TEP, 63 open) were performed under general anaesthetic. 92 % were discharged on day zero. Telephone follow-up day two rather than seven decreased attendance to primary care services (25 % vs. 57 %, p = 0.001). At 3 months, 95 % were satisfied and symptom scores were reduced (median 5–0, p < 0.0001).
Conclusion
Single-visit surgery appears to extend the patient benefits of laparoscopy by reducing hospital visits without compromising safety. Single hospital visit hernia surgery for unselected primary care referrals is possible and acceptable to patients.





Similar content being viewed by others
References
NHS Executive (2005) Treatment centres: delivering faster, quality care for NHS patients. Department of Health, London
Scott-Coombes D (2002) European working time directive for doctors in training. Reduction in juniors’ hours abolishes concept of continuity of care. BMJ 324(7339):736
Maxwell AJ, Crocker M, Jones TL, Bhagawati D, Papadopoulos MC, Bell BA (2010) Implementation of the European working time directive in neurosurgery reduces continuity of care and training opportunities. Acta Neurochir (Wien) 152(7):1207–1210
Tran TT, Kaneva P, Mayo NE, Fried GM, Feldman LS (2014) Short-stay surgery: what really happens after discharge? Surgery 156(1):20–27
van Boxel GI, Hart M, Kiszely A, Appleton S (2013) Elective day-case laparoscopic cholecystectomy: a formal assessment of the need for outpatient follow-up. Ann R Coll Surg Engl 95(8):e142–e146
Franneby U, Gunnarsson U, Andersson M, Heuman R, Nordin P, Nyren O et al (2008) Validation of an Inguinal Pain Questionnaire for assessment of chronic pain after groin hernia repair. Br J Surg 95(4):488–493
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Aylin P, Williams S, Jarman B, Bottle A (2005) Trends in day surgery rates. BMJ 331(7520):803
Paton F, Chambers D, Wilson P, Eastwood A, Craig D, Fox D et al (2014) Effectiveness and implementation of enhanced recovery after surgery programmes: a rapid evidence synthesis. BMJ Open 4(7):e005015
Putnis S, Merville-Tugg R, Atkinson S (2004) ‘One-stop’ inguinal hernia surgery—day-case referral, diagnosis and treatment. Ann R Coll Surg Engl 86(6):425–427
Voorbrood CE, Burgmans JP, Clevers GJ, Davids PH, Verleisdonk EJ, Schouten N et al (2015) One-stop endoscopic hernia surgery: efficient and satisfactory. Hernia 19(3):395–400
Jutte EH, Cense HA, Dur AH, Hunfeld MA, Cramer B, Breederveld RS (2010) A pilot study for one-stop endoscopic total extraperitoneal inguinal hernia repair. Surg Endosc 24(11):2730–2734
Siddique K, Elsayed SE, Cheema R, Mirza S, Basu S (2012) One-stop cholecystectomy clinic: an application of lean thinking—can it improve the outcomes? J Perioper Pract 22(11):360–365
Barnett SJ, Frischer JS, Gaskey JA, Ryckman FC, von Allmen D (2012) Pediatric hernia repair: 1-stop shopping. J Pediatr Surg 47(1):213–216
Tagge EP, Hebra A, Overdyk F, Burt N, Egbert M, Wilder A et al (1999) One-stop surgery: evolving approach to pediatric outpatient surgery. J Pediatr Surg 34(1):129–132
Edwards P, Roberts I, Clarke M, DiGuiseppi C, Pratap S, Wentz R et al (2007) Methods to increase response rates to postal questionnaires. Cochrane Database Syst Rev 2:MR000008
CerdanCarbonero MT, Sanz LR, Martinez RC (2005) Improving communication between levels of health care: direct referral of patients to a one-stop service for major outpatient surgery. Aten Primaria 35(6):283–287
Augestad KM, Revhaug A, Vonen B, Johnsen R, Lindsetmo RO (2008) The one-stop trial: does electronic referral and booking by the general practitioner (GPs) to outpatient day case surgery reduce waiting time and costs? A randomized controlled trial protocol. BMC Surg 8:14
Funding
NHS England Regional Innovation Fund Award 2012.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Carty NJ, Curtis NJ and Ranaboldo CJ have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Carty, N.J., Curtis, N.J. & Ranaboldo, C.J. Single hospital visit day case laparoscopic hernia repair without prior outpatient consultation is safe and acceptable to patients. Surg Endosc 30, 5565–5571 (2016). https://doi.org/10.1007/s00464-016-4929-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-4929-3