Abstract
Background
Minimally invasive pancreaticoduodenectomy (PD) remains an uncommon procedure, and the safety and efficacy remain uncertain beyond single institution case series. The aim of this study is to compare outcomes and costs between laparoscopic (LPD) and open PD (OPD) using a large population-based database.
Methods
The Nationwide Inpatient Sample database (a sample of approximately 20 % of all hospital discharges) was analyzed to identify patients who underwent PD from 2000 to 2010. Patient demographics, comorbidities, hospital characteristics, inflation-adjusted total charges, and complications were evaluated using univariate and multivariate logistic regression. Hospitals were categorized as high-volume hospitals (HVH) if more than 20 PD (open and laparoscopic) were performed annually, while those performing fewer than 20 PD were classified as low-volume hospitals.
Results
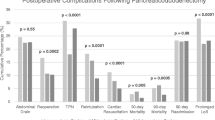
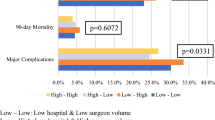
Of the 15,574 PD identified, 681 cases were LPD (4.4 %). Compared to OPD, patients who underwent LPD were slightly older (65 vs. 67 years; p = 0.001) and were more commonly treated at HVH (56.6 vs. 66.1 %; p < 0.001). Higher rates of complications were observed in OPD than LPD (46 vs. 39.4 %; p = 0.001), though mortality rates were comparable (5 vs. 3.8 %, p = 0.27). Inflation-adjusted median hospital charges were similar between OPD and LPD ($87,577 vs. $81,833, p = 0.199). However, hospital stay was slightly longer in the OPD group compared to LPD group (12 vs. 11 days, p < 0.001). Stratifying outcomes by hospital volume, LPD at HVH resulted in shorter hospital stays (9 vs. 13 days, p < 0.001), which translated into significantly lower median hospital charges ($76,572 vs. $106,367, p < 0.001).
Conclusions
Contrary to fears regarding the potential for compromised outcomes early in the learning curve, LPD morbidity in its first decade is modestly reduced, while hospital costs are comparable to OPD. In high-volume pancreatic hospitals, LPD is associated with a reduction in length of stay and hospital costs.

Similar content being viewed by others
References
Haverkamp L, Weijs TJ, van der Sluis PC, van der Tweel I, Ruurda JP, van Hillegersberg R (2013) Laparoscopic total gastrectomy versus open total gastrectomy for cancer: a systematic review and meta-analysis. Surg Endosc 27:1509–1520
Winslow ER, Brunt LM (2003) Perioperative outcomes of laparoscopic versus open splenectomy: a meta-analysis with an emphasis on complications. Surgery 134:647–653 (discussion 654-645)
Cameron JL, He J (2015) Two thousand consecutive pancreaticoduodenectomies. J Am Coll Surg 220:530–536
Schmidt CM, Turrini O, Parikh P, House MG, Zyromski NJ, Nakeeb A, Howard TJ, Pitt HA, Lillemoe KD (2010) Effect of hospital volume, surgeon experience, and surgeon volume on patient outcomes after pancreaticoduodenectomy: a single-institution experience. Arch Surg 145:634–640
Tseng JF, Pisters PW, Lee JE, Wang H, Gomez HF, Sun CC, Evans DB (2007) The learning curve in pancreatic surgery. Surgery 141:694–701
Hardacre JM (2010) Is there a learning curve for pancreaticoduodenectomy after fellowship training? HPB Surg 2010:230287
de la Fuente SG (2013) Laparoscopic pancreaticoduodenectomies: a word of caution. J Am Coll Surg 216:1218
Kooby DA (2006) Laparoscopic surgery for cancer: historical, theoretical, and technical considerations. Oncology (Williston Park) 20:917–927 (discussion 927-918, 931-912)
Gagner M, Palermo M (2009) Laparoscopic whipple procedure: review of the literature. J Hepatobiliary Pancreat Surg 16:726–730
Kendrick ML, Cusati D (2010) Total laparoscopic pancreaticoduodenectomy: feasibility and outcome in an early experience. Arch Surg 145:19–23
Elixhauser A, Steiner C, Harris DR, Coffey RM (1998) Comorbidity measures for use with administrative data. Med Care 36:8–27
Meguid RA, Ahuja N, Chang DC (2008) What constitutes a “high-volume” hospital for pancreatic resection? J Am Coll Surg 206(622):e621–e629
Fong Y, Gonen M, Rubin D, Radzyner M, Brennan MF (2005) Long-term survival is superior after resection for cancer in high-volume centers. Ann Surg 242:540–544 (discussion 544-547)
Birkmeyer JD, Finlayson SR, Tosteson AN, Sharp SM, Warshaw AL, Fisher ES (1999) Effect of hospital volume on in-hospital mortality with pancreaticoduodenectomy. Surgery 125:250–256
Kooby DA, Hawkins WG, Schmidt CM, Weber SM, Bentrem DJ, Gillespie TW, Sellers JB, Merchant NB, Scoggins CR, Martin RC 3rd, Kim HJ, Ahmad S, Cho CS, Parikh AA, Chu CK, Hamilton NA, Doyle CJ, Pinchot S, Hayman A, McClaine R, Nakeeb A, Staley CA, McMasters KM, Lillemoe KD (2010) A multicenter analysis of distal pancreatectomy for adenocarcinoma: is laparoscopic resection appropriate? J Am Coll Surg 210:779–785 (786-777)
Vijan SS, Ahmed KA, Harmsen WS, Que FG, Reid-Lombardo KM, Nagorney DM, Donohue JH, Farnell MB, Kendrick ML (2010) Laparoscopic vs open distal pancreatectomy: a single-institution comparative study. Arch Surg 145:616–621
Rutz DR, Squires MH, Maithel SK, Sarmiento JM, Etra JW, Perez SD, Knechtle W, Cardona K, Russell MC, Staley CA 3rd, Sweeney JF, Kooby DA (2014) Cost comparison analysis of open versus laparoscopic distal pancreatectomy. HPB (Oxford) 16:907–914
Limongelli P, Belli A, Russo G, Cioffi L, D’Agostino A, Fantini C, Belli G (2012) Laparoscopic and open surgical treatment of left-sided pancreatic lesions: clinical outcomes and cost-effectiveness analysis. Surg Endosc 26:1830–1836
Xourafas D, Tavakkoli A, Clancy TE, Ashley SW (2015) Distal pancreatic resection for neuroendocrine tumors: Is laparoscopic really better than open?. J Gastrointest Surg 19(5):831–840. doi: 10.1007/s11605-015-2788-1
Palanivelu C, Jani K, Senthilnathan P, Parthasarathi R, Rajapandian S, Madhankumar MV (2007) Laparoscopic pancreaticoduodenectomy: technique and outcomes. J Am Coll Surg 205:222–230
Zureikat AH, Breaux JA, Steel JL, Hughes SJ (2011) Can laparoscopic pancreaticoduodenectomy be safely implemented? J Gastrointest Surg 15(7):1151–1157
Song KB, Kim SC, Hwang DW, Lee JH, Lee DJ, Lee JW, Park KM, Lee YJ (2015) Matched case–control analysis comparing laparoscopic and open pylorus-preserving pancreaticoduodenectomy in patients with periampullary tumors. Ann Surg 262(1):146–155. doi:10.1097/SLA.0000000000001079
Dokmak S, Fteriche FS, Aussilhou B, Bensafta Y, Levy P, Ruszniewski P, Belghiti J, Sauvanet A (2015) Laparoscopic Pancreaticoduodenectomy Should Not Be Routine for Resection of Periampullary Tumors. J Am Coll Surg
Strasberg SM, Ludbrook PA (2003) Who oversees innovative practice? Is there a structure that meets the monitoring needs of new techniques? J Am Coll Surg 196:938–948
Mesleh MG, Stauffer JA, Bowers SP, Asbun HJ (2013) Cost analysis of open and laparoscopic pancreaticoduodenectomy: a single institution comparison. Surg Endosc 27:4518–4523
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Tran, Dua, Worhunsky, Poultsides, Norton, and Visser have no relevant conflict of interests.
Rights and permissions
About this article
Cite this article
Tran, T.B., Dua, M.M., Worhunsky, D.J. et al. The First Decade of Laparoscopic Pancreaticoduodenectomy in the United States: Costs and Outcomes Using the Nationwide Inpatient Sample. Surg Endosc 30, 1778–1783 (2016). https://doi.org/10.1007/s00464-015-4444-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4444-y