Abstract
Background
Peripancreatic fluid collections (PFCs) occur in up to 30 % of patients following partial pancreatic resections. Traditionally, postoperative PFCs are managed via percutaneous drainage (PD). EUS-guided transgastric drainage has been shown to be effective for the management of PFCs secondary to acute pancreatitis. However, there are limited data on the use of EUS-guided drainage (EUSD) for the management of postoperative PFCs.
Objective
To compare the safety and efficacy of PD versus EUSD of PFCs in patients who have undergone partial pancreatic resections.
Design
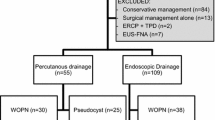
Retrospective analysis of patients with symptomatic PFCs following pancreatic enucleation or distal pancreatectomy at MSKCC between January 2008 and December 2010. Patients were identified using an electronic medical records query in addition to a prospectively maintained pancreatic surgery complications database.
Setting
Single, academic, tertiary referral center.
Patients
Twenty-three patients with symptomatic PFCs following pancreatic enucleation or distal pancreatectomy were retrospectively identified.
Interventions
CT-guided PD versus endoscopic ultrasound-guided drainage (EUSD)
Main outcome measures
Outcomes included technical success, clinical success, number of interventions, and complications. Technical success was defined as successful localization of the PFC by fine-needle aspiration and placement of a drainage catheter or stent. Clinical success was defined as radiographic resolution of the PFC and removal of the drain or stent, without the need for an alternative drainage procedure or surgery.
Results
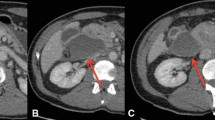
PD was initially performed in 14 patients and EUSD initially in 9 patients. Three patients with initial PD had recurrence of PFC after removal of the external drain and underwent subsequent EUSD. The mean size of the fluid collections was 10.0 cm in the PD group and 8.9 cm in the EUSD group. Technical success was achieved in all patients in both groups. Clinical success was achieved in 11 of 14 (79 %) patients in the PD group compared with 11 of 11 (100 %) in the EUSD group, with one patient in the EUSD group lost to follow-up. One patient with initial PD required two additional percutaneous procedures before complete PFC resolution. Five EUSD patients required repeat endoscopy for stent revision or necrosectomy. The median number of interventions was two [range 1–5] in the PD group and two [range 1–5] in the EUSD group. The median number of days the drainage catheters were in place was 44.5 [range 2–87] in the PD group versus 57 [range 32–217] in the EUSD group. There were no procedure-related complications in either group. Adverse events in the PD group included splenic artery stump bleeding, pleural effusion, cysto-colonic and cysto-cutaneous fistulae, and persistent catheter site pain. One patient in the EUSD group developed a small-bowel obstruction and bleeding gastric ulcer.
Limitations
Retrospective, nonrandomized study and small numbers.
Conclusions
EUSD of postoperative PFCs appears to be safe and technically feasible. This technique appears to be as successful as PD for the management of PFCs with the advantage of not requiring an external drainage apparatus and should be considered as a therapeutic option in this group of patients. Further evaluation, with analysis of cost and quality of life, should be considered in a prospective, randomized trial.
Similar content being viewed by others
References
Lillemoe KD et al (1999) Distal pancreatectomy: indications and outcomes in 235 patients. Ann Surg 229(5):693–698 discussion 698–700
Jayaraman S et al (2010) Laparoscopic distal pancreatectomy: evolution of a technique at a single institution. J Am Coll Surg 211(4):503–509
Goh BK et al (2008) Critical appraisal of 232 consecutive distal pancreatectomies with emphasis on risk factors, outcome, and management of the postoperative pancreatic fistula: a 21-year experience at a single institution. Arch Surg 143(10):956–965
Kleeff J et al (2007) Distal pancreatectomy: risk factors for surgical failure in 302 consecutive cases. Ann Surg 245(4):573–582
Ferrone CR et al (2008) Pancreatic fistula rates after 462 distal pancreatectomies: staplers do not decrease fistula rates. J Gastrointest Surg 12(10):1691–1697 discussion 1697-1698
Kooby DA et al (2008) Left-sided pancreatectomy: a multicenter comparison of laparoscopic and open approaches. Ann Surg 248(3):438–446
Freeny PC et al (1998) Percutaneous CT-guided catheter drainage of infected acute necrotizing pancreatitis: techniques and results. AJR Am J Roentgenol 170(4):969–975
Matthews JB (2011) Prevention, evaluation, and treatment of leaks after pancreatic surgery. J Gastrointest Surg 15(8):1327–1328
Vin Y et al (2008) Management and outcomes of postpancreatectomy fistula, leak, and abscess: results of 908 patients resected at a single institution between 2000 and 2005. J Am Coll Surg 207(4):490–498
Giovannini M et al (2001) Endoscopic ultrasound-guided drainage of pancreatic pseudocysts or pancreatic abscesses using a therapeutic echo endoscope. Endoscopy 33(6):473–477
Smits ME et al (1995) The efficacy of endoscopic treatment of pancreatic pseudocysts. Gastrointest Endosc 42(3):202–207
Varadarajulu S, Trevino JM, Christein JD (2009) EUS for the management of peripancreatic fluid collections after distal pancreatectomy. Gastrointest Endosc 70(6):1260–1265
Varadarajulu S, Wilcox CM, Christein JD (2011) EUS-guided therapy for management of peripancreatic fluid collections after distal pancreatectomy in 20 consecutive patients. Gastrointest Endosc 74(2):418–423
Bassi C et al (2005) Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 138(1):8–13
Adams DB, Anderson MC (1992) Percutaneous catheter drainage compared with internal drainage in the management of pancreatic pseudocyst. Ann Surg 215(6):571–576 discussion 576-578
Varadarajulu S et al (2011) Endoscopic transmural drainage of peripancreatic fluid collections: outcomes and predictors of treatment success in 211 consecutive patients. J Gastrointest Surg 15(11):2080–2088
Hookey LC et al (2006) Endoscopic drainage of pancreatic-fluid collections in 116 patients: a comparison of etiologies, drainage techniques, and outcomes. Gastrointest Endosc 63(4):635–643
Baron TH et al (2002) Outcome differences after endoscopic drainage of pancreatic necrosis, acute pancreatic pseudocysts, and chronic pancreatic pseudocysts. Gastrointest Endosc 56(1):7–17
Seifert H et al (2000) Retroperitoneal endoscopic debridement for infected peripancreatic necrosis. Lancet 356(9230):653–655
Mathew A, Biswas A, Meitz KP (2008) Endoscopic necrosectomy as primary treatment for infected peripancreatic fluid collections (with video). Gastrointest Endosc 68(4):776–782
Seewald S et al (2005) Aggressive endoscopic therapy for pancreatic necrosis and pancreatic abscess: a new safe and effective treatment algorithm (videos). Gastrointest Endosc 62(1):92–100
Rau B, Bothe A, Beger HG (2005) Surgical treatment of necrotizing pancreatitis by necrosectomy and closed lavage: changing patient characteristics and outcome in a 19-year, single-center series. Surgery 138(1):28–39
Rodriguez JR et al (2008) Debridement and closed packing for sterile or infected necrotizing pancreatitis: insights into indications and outcomes in 167 patients. Ann Surg 247(2):294–299
Connor S et al (2005) Early and late complications after pancreatic necrosectomy. Surgery 137(5):499–505
van Santvoort HC et al (2010) A step-up approach or open necrosectomy for necrotizing pancreatitis. N Engl J Med 362(16):1491–1502
Grobmyer SR et al (2009) Pancreatic stent placement is associated with resolution of refractory grade C pancreatic fistula after left-sided pancreatectomy. Am Surg 75(8):654–657 discussion 657–658
Varadarajulu S, Christein JD, Wilcox CM (2011) Frequency of complications during EUS-guided drainage of pancreatic fluid collections in 148 consecutive patients. J Gastroenterol Hepatol 26(10):1504–1508
Disclosures
Drs. DiMaio and Schattner serve as consultants for Boston Scientific. Dr. Gerdes is a consultant for Helsinn Pharmaceuticals.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kwon, Y.M., Gerdes, H., Schattner, M.A. et al. Management of peripancreatic fluid collections following partial pancreatectomy: a comparison of percutaneous versus EUS-guided drainage. Surg Endosc 27, 2422–2427 (2013). https://doi.org/10.1007/s00464-012-2752-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2752-z