Abstract
Background
Sphincter augmentation with the LINX® Reflux Management System is a surgical option for patients with chronic gastroesophageal disease (GERD) and an inadequate response to proton pump inhibitors (PPIs). Clinical experience with sphincter augmentation is now available out to 4 years.
Methods
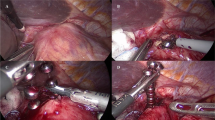
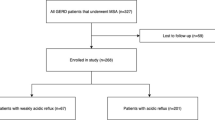
In a multicenter, prospective, single-arm study, 44 patients underwent a laparoscopic surgical procedure for placement of the LINX System around the gastroesophageal junction (GEJ). Each patient’s baseline GERD status served as the control for evaluations post implant. Long-term efficacy measures included esophageal acid exposure, GERD quality-of-life measures, and use of PPIs. Adverse events and long-term complications were closely monitored.
Results
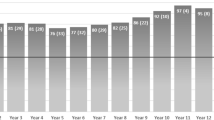
For esophageal acid exposure, the mean total % time pH < 4 was reduced from 11.9 % at baseline to 3.8 % at 3 years (p < 0.001), with 80 % (18/20) of patients achieving pH normalization (≤5.3 %). At ≥4 years, 100 % (23/23) of the patients had improved quality-of-life measures for GERD, and 80 % (20/25) had complete cessation of the use of PPIs. There have been no reports of death or long-term device-related complications such as migration or erosion.
Conclusions
Sphincter augmentation with the LINX Reflux Management System provided long-term clinical benefits with no safety issues, as demonstrated by reduced esophageal acid exposure, improved GERD-related quality of life, and cessation of dependence on PPIs, with minimal side effects and no safety issues. Patients with inadequate symptom control with acid suppression therapy may benefit from treatment with sphincter augmentation.


Similar content being viewed by others
References
Everhart JE, Ruhl CE (2009) The burden of digestive diseases in the United States part I: overall and upper gastrointestinal diseases. Gastroenterology 136:376–386
Shaheen NJ, Hansen RA, Morgan DR (2006) The burden of gastrointestinal and liver diseases. Am J Gastroenterol 101:2128–2138
Kahrilas PJ (2008) Clinical practice. Gastroesophageal reflux disease. N Engl J Med 359:1700–1707
Mainie I, Tutuian R, Shay S, Vela M, Zhang X, Sifrim D, Castell DO (2006) Acid and non-acid reflux in patients with persistent symptoms despite acid suppressive therapy: a multicentre study using combined ambulatory impedance-pH monitoring. Gut 55:1398–1402
Samelson SL, Wieser HF, Bombeck CT (1983) A new concept in the surgical treatment of gastroesophageal reflux. Ann Surg 197:254–259
Kwiatek MA, Pandolfino JE, Hirano I, Kahrilas PJ (2010) Esophagogastric junction distensibility assessed with an endoscopic functional luminal imaging probe (EndoFLIP). Gastrointest Endosc 2:272–278
Pandolfino JE, Zhang Q, Ghosh SK (2006) Transient lower esophageal sphincter relaxations and reflux: mechanistic analysis using concurrent fluoroscopy and high-resolution manometry. Gastroenterology 131:1725–1733
Velanovich V (1998) Comparison of generic (SF-36) vs. disease-specific (GERD–HRQL) quality of life scales for gastroesophageal reflux disease. J Gastrointest Surg 2:141–145
Bonavina L, Saino GI, Bona D, DeMeester TR, Lipham JC, Ganz R, Dunn D, Fockens P, Bemelman W (2008) Magnetic augmentation of the lower esophageal sphincter: results of a feasibility clinical trial. J Gastrointest Surg 12:2133–2140
Bonavina L, DeMeester T, Fockens P, Saino GI, Bona D, DeMeester TR, Lipham JC, Ganz R, Dunn D, Bemelman W (2010) Laparoscopic sphincter augmentation device eliminates reflux symptoms and normalizes esophageal acid exposure: one and two-year results of a feasibility trial. Ann Surg 252:857–862
Ganz R, Gostout C, Grudem J, Berg T, DeMeester TR (2008) Use of a magnetic sphincter for the treatment of GERD: a feasibility study. Gastrointest Endosc 67:287–294
Chen D, Barber C, McLoughlin P, Thavaneswaran P, Jamieson GG, Maddern GJ (2009) Systematic review of endoscopic treatments for gastro-oesophageal reflux disease. Br J Surg 96:128–136
Johnson LF, DeMeester TR (1986) Development of the 24-hour intraesophageal pH monitoring composite scoring system. J Clin Gastroenterol 8(Suppl):52–58
Fumagalli RU, Barbera R, Repici A, Porta M, Malesci A, Rosati R (2011) Nissen fundoplication after failure of endoluminal fundoplication: short-term results. J Gastrointest Surg 15:439–443
Hunter JG, Smith CD, Braunum GD (1999) Laparoscopic fundoplication failures: patterns of failure and response to fundoplication revision. Ann Surg 230:595–606
Little AG, Ferguson MK, Skinner DB (1986) Reoperation for failed antireflux operations. J Thorac Cardiovasc Surg 91:511–517
Disclosures
Drs. Tom DeMeester, Luigi Bonavina, Robert Ganz, and Paul Fockens have been or currently are consultants for Torax Medical. Drs. John Lipham, Greta Saino, Daniel Dunn, and Willem Bemelman have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lipham, J.C., DeMeester, T.R., Ganz, R.A. et al. The LINX® reflux management system: confirmed safety and efficacy now at 4 years. Surg Endosc 26, 2944–2949 (2012). https://doi.org/10.1007/s00464-012-2289-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2289-1