Abstract
Background
Biologic implants have been recommended for reinforcement in routine and challenging hernia repair. However, experimental and clinical studies have reported adverse effects (e.g., slow implant integration and pronounced foreign body reaction). To evaluate the impact of different material processing methods (cross-linking vs. non-cross-linking of collagen) and implant design, four different biologic hernia implants were compared directly in experimental intraperitoneal onlay mesh plasty (IPOM). Tissue integration, shrinkage, and foreign body reaction were primary outcome parameters.
Methods
In this study, 48 Sprague–Dawley rats were randomized to four treatment groups. Open IPOM repair was performed. One peritoneal defect per animal was covered with 2 × 2 cm patches of cross-linked or non-cross-linked implants including CollaMend (n = 12), Peripatch (n = 12), Surgisis (n = 12), and Tutomesh (n = 12). In half of the animals, fibrin sealant was applied for additional fixation and to cover sutures. The observation period was 60 days. The primary outcome parameters were implant integration, shrinkage, and foreign body reaction. Macroscopic and histologic assessments were performed.
Results
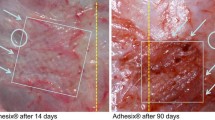
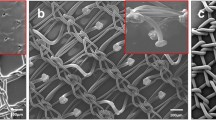
The integration of implants was insufficient in all the groups. The implants could be detached easily from the underlying tissue, and the penetration of fibroblasts and vessels was limited to the perforations. Foreign body reaction was pronounced with CollaMend and Surgisis, leading to persistent granulomatous inflammation. Shrinkage was excessive with Surgisis, whereas Tutomesh and Peripatch yielded sufficient anti-adhesion and elicited no foreign body reaction.
Conclusion
At 2 months, cross-linked and non-cross-linked biologic hernia implants were poorly integrated. Cross-linking led to a more pronounced foreign body reaction. Less inflammatory response may reduce local complications, but did not enhance implant integration in this study.







Similar content being viewed by others
References
Catena F, Ansaloni L, Leone A, De CA, Gagliardi S, Gazzotti F, Peruzzi S, Agrusti S, D’Alessandro L, Taffurelli M (2005) Lichtenstein repair of inguinal hernia with Surgisis inguinal hernia matrix soft-tissue graft in immunodepressed patients. Hernia 9:29–31
Agresta F, Bedin N (2008) Transabdominal laparoscopic inguinal hernia repair: is there a place for biological mesh? Hernia 12:609–612
Brown P (2009) Abdominal wall reconstruction using biological tissue grafts. AORN J 90:513–520
Wisbach G, Peterson T, Thoman D (2006) Early results of the use of acellular dermal allograft in type III paraesophageal hernia repair. JSLS 10:184–187
Cavallaro A, Lo ME, Di VM, Zanghi A, Cavallaro V, Veroux PF, Cappellani A (2010) Use of biological meshes for abdominal wall reconstruction in highly contaminated fields. World J Gastroenterol 16:1928–1933
Sailes FC, Walls J, Guelig D, Mirzabeigi M, Long WD, Crawford A, Moore JH Jr, Copit SE, Tuma GA, Fox J (2010) Synthetic and biological mesh in component separation: a 10-year single institution review. Ann Plast Surg 64:696–698
Gupta A, Zahriya K, Mullens PL, Salmassi S, Keshishian A (2006) Ventral herniorrhaphy: experience with two different biosynthetic mesh materials, Surgisis and Alloderm. Hernia 10:419–425
Rosen MJ (2010) Biologic mesh for abdominal wall reconstruction: a critical appraisal. Am Surg 76:1–6
Hiles M, Record Ritchie RD, Altizer AM (2009) Are biologic grafts effective for hernia repair? A systematic review of the literature. Surg Innov 16:26–37
Petter-Puchner AH, Fortelny RH, Walder N, Morales-Conde S, Gruber-Blum S, Ohlinger W, Redl H (2010) Small intestine submucosa (SIS) implants in experimental IPOM repair. J Surg Res 161:264–271
Petter-Puchner AH, Walder N, Redl H, Schwab R, Ohlinger W, Gruber-Blum S, Fortelny RH (2008) Fibrin sealant (Tissucol) enhances tissue integration of condensed polytetrafluoroethylene meshes and reduces early adhesion formation in experimental intraabdominal peritoneal onlay mesh repair. J Surg Res 150:190–195
Petter-Puchner A, Fortelny R, Walder N, Mittermayr R, Öhinger W, van Griensven M, Redl H (2007) Adverse effects associated with the use of porcine cross-linked collagen implants in an experimental model of incisional hernia repair. J Surg Res 145:105–110
Gruber-Blum S, Petter-Puchner AH, Mika K, Brand J, Redl H, Ohlinger W, Benesch T, Fortelny RH (2010) A comparison of a bovine albumin/glutaraldehyde glue versus fibrin sealant for hernia mesh fixation in experimental onlay and IPOM repair in rats. Surg Endosc 24(12):3086–3094
Prieto-Diaz-Chavez E, Medina-Chavez JL, Ramirez-Barba EJ, Trujillo-Hernandez B, Millan-Guerrero RO, Vasquez C (2008) Reduction of peritoneal adhesion to polypropylene mesh with the application of fibrin glue. Acta Chir Belg 108:433–437
Schug-Pass C, Lippert H, Kockerling F (2010) Mesh fixation with fibrin glue (Tissucol/Tisseel[R]) in hernia repair dependent on the mesh structure: is there an optimum fibrin–mesh combination? Investigations on a biomechanical model. Langenbecks Arch Surg 395:569–574
Sandor M, Xu H, Connor J, Lombardi J, Harper JR, Silverman RP, McQuillan DJ (2008) Host response to implanted porcine-derived biologic materials in a primate model of abdominal wall repair. Tissue Eng Part A 14:2021–2031
Marreco PR, da Luz MP, Genari SC, Moraes AM (2004) Effects of different sterilization methods on the morphology, mechanical properties, and cytotoxicity of chitosan membranes used as wound dressings. J Biomed Mater Res B Appl Biomater 71:268–277
Rueter A, Schleicher JB (1969) Elimination of toxicity from polyvinyl trays after sterilization with ethylene oxide. Appl Microbiol 18:1057–1059
Poulose BK, Scholz S, Moore DE, Schmidt CR, Grogan EL, Lao OB, Nanney L, Davidson J, Holzman MD (2005) Physiologic properties of small intestine submucosa. J Surg Res 123:262–267
Gilbert TW, Freund JM, Badylak SF (2009) Quantification of DNA in biologic scaffold materials. J Surg Res 152:135–139
Ansaloni L, Cambrini P, Catena F, Saverio SD, Gagliardi S, Gazzotti F, Hodde JP, Metzger DW, D’Alessandro L, Pinna AD (2007) Immune response to small intestinal submucosa (Surgisis) implant in humans: preliminary observations. J Invest Surg 20:237–241
Konstantinovic ML, Ozog Y, Spelzini F, Pottier C, De RD, Deprest J (2010) Biomechanical findings in rats undergoing fascial reconstruction with graft materials suggested as an alternative to polypropylene. Neurourol Urodyn 29:488–493
Helton WS, Fisichella PM, Berger R, Horgan S, Espat NJ, Abcarian H (2005) Short-term outcomes with small intestinal submucosa for ventral abdominal hernia. Arch Surg 140:549–560
Burger JW, Halm JA, Wijsmuller AR, ten Raa S, Jeekel J (2006) Evaluation of new prosthetic meshes for ventral hernia repair. Surg Endosc 20:1320–1325
Disclosures
H. Redl works as a senior consultant for Baxter. A. H. Petter-Puchner, R. H. Fortelny, K. Silic, J. Brand, and S. Gruber-Blum have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Petter-Puchner, A.H., Fortelny, R.H., Silic, K. et al. Biologic hernia implants in experimental intraperitoneal onlay mesh plasty repair: the impact of proprietary collagen processing methods and fibrin sealant application on tissue integration. Surg Endosc 25, 3245–3252 (2011). https://doi.org/10.1007/s00464-011-1700-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-011-1700-7