Abstract
Background
Concerns have been raised regarding outcome after laparoscopic resection of hepatic neoplasms. This prospective study compared morbidity and adequacy of surgical margins in laparoscopic (LLR) versus open liver resection (OLR).
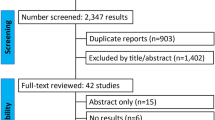
Methods
Outcome in 359 consecutive patients [male/female ratio 187/172; median age 60 years (range 18–84 years)] who underwent partial hepatectomy was analysed. Cirrhosis was present in 32 patients and preoperative chemotherapy was administered in 141 patients. Comparative analyses were performed using propensity scores for all and for matched patients (n = 76 per group).
Results
Complications occurred in 68/250 (27.2%) patients after OLR and in 6/109 (5.5%) after LLR [odds ratio (OR) 0.16; 95% confidence interval (CI) 0.07–0.37; p < 0.0001]. Median intraoperative blood loss was 500 ml (range 10–7,000 ml) in OLR and 100 ml (range 5–4,000 ml) in LLR (p < 0.0001). Postoperative hospital stay was 8 days (range 0–155 days) after OLR and 6 days (range 0–41 days) after LLR (p < 0.0001). In patients treated for liver malignancy, the surgical resection margin was positive on histopathological examination in 5/237 after OLR and in 1/77 after LLR. The magnitude of the resection margin was 7.5 mm (range 0–45 mm) in OLR and 10.0 mm (range 0–30 mm) in LLR (p = 0.087).
Conclusions
LLR for hepatic neoplasms seems to be noninferior to OLR regarding adequacy of surgical margins, and superior to OLR regarding short-term postoperative outcome.


Similar content being viewed by others
References
Buell JF, Thomas MJ, Doty TC, Gersin KS, Merchen TD, Gupta M, Rudich SM, Woodle ES (2004) An initial experience and evolution of laparoscopic resectional surgery. Surgery 136:804–811
Cherqui D, Laurent A, Tayar C, Chang S, Van Nhieu JT, Loriau J, Karoui M, Duvoux C, Dhumeaux D, Fagniez PL (2006) Laparoscopic liver resection for peripheral hepatocellular carcinoma in patients with chronic liver disease: midterm results and perspectives. Ann Surg 243:499–506
Gigot JF, Glineur D, Santiago Azagra J, Goergen M, Ceuterick M, Morino M, Etienne J, Marescaux J, Mutter D, van Krunckelsven L, Descottes B, Valleix D, Lachachi F, Bertrand C, Mansvelt B, Hubens G, Saey JP, Schockmel R; Hepatobiliary, Pancreatic Section of the Royal Belgian Society of Surgery and the Belgian Group for Endoscopic Surgery (2002) Laparoscopic liver resection for malignant liver tumors. Preliminary results of a multicenter European study. Ann Surg 236:90–97
Hompes D, Aerts R, Penninckx F, Topal B (2007) Laparoscopic liver resection using radiofrequency coagulation. Surg Endosc 21:175–180
Koffron AJ, Auffenberg G, Kung R, Abecassis M (2007) Evaluation of 300 minimally invasive liver resections at a single institution. Less is more. Ann Surg 246:385–394
Vibert E, Perniceni T, Levard H, Denet C, Shahri NK, Gayet B (2006) Laparoscopic liver resection. Br J Surg 93:67–72
Chang S, Laurent A, Tayar C, Karoui M, Cherqui D (2007) Laparoscopy as a routine approach for left lateral sectionectomy. Br J Surg 94:58–63
Strasberg SM (2005) Nomenclature of hepatic anatomy and resections: a review of the Brisbane 2000 system. J Hepatobiliairy Pancreat Surg 12:351–355
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:214–215
D’Agostino (1998) Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med 17:2265–2281
Parsons LS (2001) Reducing bias in a propensity score matched-pair sample using greedy matching techniques. SAS SUGI Proc 26:214–226
Simillis C, Constantinides VA, Tekkis PP, Darzi A, Lovegrove R, Jiao L, Antoniou A (2007) Laparoscopic versus open hepatic resections for benign and malignant neoplasms – a meta-analysis. Surgery 141:203–211
Shapiro S (1994) Meta-analysis/Shmeta-analysis. Am J Epidemiol 140:771–778
Koffron A, Geller D, Gamblin C, Abecassis M (2006) Laparoscopic liver surgery: shifting the management of liver tumors. Hepatology 44:1694–1700
Karoui M, Penna C, Amin-Hashem M, Mitry E, Benoist S, Franc B, Rougier P, Nordlinger B (2006) Influence of preoperative chemotherapy on the risk of major hepatectomy for colorectal liver metastases. Ann Surg 243:1–7
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Topal, B., Fieuws, S., Aerts, R. et al. Laparoscopic versus open liver resection of hepatic neoplasms: comparative analysis of short-term results. Surg Endosc 22, 2208–2213 (2008). https://doi.org/10.1007/s00464-008-0023-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-008-0023-9