Abstract
In Germany, studies on the IgG seroprevalence in pregnancy and in women of childbearing age are rare. Therefore, we retrospectively evaluated the CMV IgG seropositive rate in 40,324 pregnant women as well as in 31,093 female and male bone marrow donors over 15 consecutive years (1996–2010). Furthermore, the result of a study conducted in 1999 investigating 1,305 healthy adolescents with known ethnicity was included. The overall CMV IgG seroprevalence in pregnant women (15–50 years) was 42.3%. Age-dependent analysis revealed a significantly higher seropositive rate (55.6%) in young women (15–25 years) than in those aged 26–40 years (37–42%) and in women older than 40 years (48.3%). Over the study period of 15 years, the rate of seroprevalence in pregnant women declined significantly (χ2 test < 0.01) from 44.3% in the first interval period (1996–2000), to 42.8% (2001–2005) and to 40.9% (2006–2010). The most influencing factor on CMV seropositivity appeared to be the socioeconomic status (SES), which we characterized by type of health insurance: Seroprevalence in women with low, middle and upper SES was 91.8, 46.9 and 33.7%, respectively. Female bone marrow donors of childbearing age (15–45 years) showed a significantly higher seropositive rate of 36.5% than age-matched male donors (28.6%). In adolescents aged 13–16 years, no gender-specific differences were recognized. Concerning ethnicity, youngsters with German descent had a significantly lower seroprevalence (29.9%) than those with non-German descent (67.4%).
Similar content being viewed by others
Introduction
Cytomegalovirus (CMV) infection is the most common viral cause of congenital infection in the United States and in West European countries. Primary CMV infection in pregnancy poses the main risk for congenital infection and disease. The intrauterine transmission rate amounts to 35–40%. Approximately, 13% of all infected live-born infants are afflicted by symptomatic disease at birth, and of them, permanent sequelae can be expected in 40–58%. In addition, of the 87.5% asymptomatic newborns, 13.5% develop late manifestations—particularly sensorineural hearing loss and neurodevelopment disorders [1, 2]. Recurrent maternal infections are caused by reactivation of latent virus or secondary reinfection with a new CMV strain. Recurrences are common especially in populations with high CMV seroprevalence as estimated by the rate of congenital infection (about 1%). However, only <1% of congenitally infected newborns of seroimmune mothers have symptoms at birth, and about 8% develop late sequelae such as unilateral hearing loss [3].
In a review by Dollard et al., the prevalence of congenital CMV infection in industrialized West European and North American countries was reported to be about 0.7% [2]. For Germany, Scholz et al. estimated in 2000 a prevalence of 0.2% based on a 2-year multicenter study by collecting all reports on congenital CMV infection from 363 children’s hospitals [4]. In another evaluation in 2011, Hamprecht et al. reached the same rate of 0.2% in his ongoing “Tübingen congenital CMV study” by screening cord blood of (up to now) 3,418 newborns for CMV DNA [5].
Encouraged by the successful application of rubella vaccination leading to a dramatic reduction of congenital rubella syndrome, the Institute of Medicine (IOM) in the USA announced CMV as a major target for vaccine development [6]. In 2009, a phase 2 clinical trial of the recombinant CMV gycoprotein B (gB) vaccine with MF59 adjuvant in seronegative women showed promising results with an overall 50% efficacy for prevention of infection [7]. However, it will be still a long way until an effective and safe CMV vaccine with a suitable vaccination program is available. In the meantime, the only preventive possibility to lower the risk of CMV infection is hygienic measures, to which women, who know to be susceptible, would adhere more strictly [8]. Therefore, gynecologists and obstetricians should counsel every women—pregnant or planning to become pregnant—about the risk of primary CMV infection, as it is mandatory for the risk of toxoplasmosis. Although obligatory CMV screening is neither performed in Germany nor in any other country worldwide, testing for presence or absence of CMV antibodies is increasingly requested by gynecologists or the informed women themselves.
In our initial retrospective observational study on CMV seroprevalence carried out with blood samples obtained between 1996 and 2001 from 10,539 pregnant women, we found a seronegative rate of 56.7% and in susceptible women a primary infection rate of 1.1% per year [9]. In the present paper, we investigated the trend of CMV seroprevalence during the last 15 years by extending our previous study with the serological data of 29,785 pregnant women up to 2010. In addition—to evaluate the influence of gender and ethnicity on CMV seroprevalence—we included the results of two other study populations—bone marrow donors and adolescents.
Materials and methods
We retrospectively evaluated the CMV IgG seroprevalence in 3 study groups:
Pregnant women
Between 1996 and 2010, serum samples from 40,324 healthy pregnant women in the first trimester aged 15–50 years (median 31) were obtained from gynecologists throughout Germany for obligatory antenatal screening (rubella, syphilis, hepatitis B and blood grouping) including CMV serology on request. The majority of samples came from Baden-Württemberg (29%), followed by North-Rhine-Westphalia (20%) and Bavaria (17%). In 68.1% (27,465/40,324), health insurance status was reported.
Bone marrow donors
Between 1996 and 2010, serum samples from 31,093 healthy bone marrow donors of both sexes aged 18–55 years (median 32) were investigated for CMV-specific IgG and IgM. Information on age was available on a subset of 10,606 samples obtained after 2000.
Adolescents
Serum samples of 1,305 healthy adolescents aged 13–16 years were obtained from pediatricians in the Stuttgart area during a preventive medical check-up (J1-Studie) in 1999 for detection of specific IgG antibodies to various vaccine-preventable infections (e.g. measles, mumps, rubella) as well as non-vaccine-preventable infections including CMV. Ethnicity was reported for all 1,305 adolescents.
Serological method
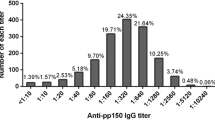
CMV-specific IgG antibody levels were determined with the Enzygnost® Anti-CMV IgG EIA (Siemens/Dade Behring, Marburg, Germany) using the BEPIII ELISA processor (Siemens/Dade Behring, Marburg, Germany) according to the manufacturer’s recommendation. IgG values were expressed as Paul-Ehrlich Institute Units (PEIU) in mPEIU/ml. Sera with an activity of <200 mPEIU/ml (OD corrected <0.100) were considered negative, between 200 and 400 mPEIU/ml (OD corrected 0.1–0.2) equivocal, between >400 and 900 mPEIU/ml (OD corrected >0.2) low positive and >900 mPEIU/ml positive.
In the calculation of seroprevalence equivocal IgG results—detected in 0.42–0.49% of samples—were defined as positive.
Definition of socioeconomic status (SES)
The SES was approximated by the patient’s health insurance: Welfare recipients, who get financial assistance for medical care, are defined as lower SES, patients with statutory health insurance as middle SES and those with private health insurance as upper SES. In Germany, private insurances only admit employees with a salary limit of 45,000 € per year (2010) and self-employed people and public servants.
Statistics
The 95% confidence intervals (95% CI) were calculated, and χ2 test was used for significant differences between age groups and SES. p values <0.05 were considered statistically significant.
Results
CMV IgG seroprevalence
The CMV IgG seropositive rates in the various study groups are presented in Table 1. The CMV seroprevalence for pregnant women was 42.3% with a median IgG antibody level of 5,591 mPEIU/ml (25–75% quantile: 3,172–9,074 mPEIU/ml).
Bone marrow donors with an overall prevalence of 34.3% showed a difference for women and men of 39.5 and 31.6%, respectively (p < 0.0001). For adolescents aged 13–16 years with an overall prevalence of 35.0%, no significant gender-specific difference (p = 0.53) was evident. Concerning ethnicity, an increased rate of 67.4% among adolescents of non-German (mostly Turkish or Italian) descent was apparent.
Age-related CMV IgG seroprevalence
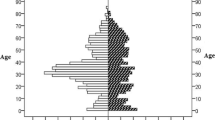
CMV IgG prevalence in pregnant women according to age is shown in Fig. 1a. Young women aged 15–25 years had a significant higher seroprevalence of 55.6% than older women aged 26–40 years. Lowest prevalence (37.0%) was observed between 31 and 35 years. In the following two age groups, prevalence increased to 38.9 (36–40 years) and 48.3% (41–50 years).
a Age-related CMV IgG seroprevalence in pregnant women (n = 40,324, stripped columns). Numbers above columns indicate the total number of sera tested per age group. b Age-related CMV IgG seroprevalence in bone marrow donors (n = 10,606) stratified by gender. Female donors (n = 3,048, white columns), male donors (n = 7,558, black columns). Numbers above columns indicate the total number of sera tested per age group
An age-related increase of IgG seroprevalences in both female and male bone marrow donors is presented in Fig. 1b. Female donors (n = 2,687) of childbearing age (15–45 years) had a significant higher overall seroprevalence of 36.5% than age-matched men (n = 6,888) with 28.6%. Beyond 46 years of age, the gender-specific disparity declined. In female bone marrow donors aged 15–25 years, we found a significantly (χ2 test <0.01) lower CMV seropositive rate of 32.3% compared to pregnant women of the same age (55.6%).
CMV IgG seroprevalence—changes over time?
Table 2 presents the seroprevalences of pregnant women and female bone marrow donors stratified by three 5-year intervals of investigation. In the former, the IgG seropositive rate significantly (χ2 test <0.01) dropped from 44.3% in the first (1996–2000), to 42.8% in second (2001–2005) and 40.9% in the third interval of investigation (2006–2010). Concomitantly, the median age of pregnant women increased between the first, second and third interval from 29 to 31 to 32 years, respectively. For female bone marrow donors, seroprevalences also decreased between the first and second interval from 41.2 to 36.9% (p < 0.01), but remained stable between the second and the third interval (37.4%).
Influence of socioeconomic status on CMV IgG seroprevalence
From Table 3, it is evident that seroprevalence was dependent on socioeconomic status (SES) as defined by type of health insurance. Immunity to CMV was found in 91.8% (95% CI: 88.3–94.5) of women with low SES, in 46.9% (95% CI: 46.2–47.7) of those with middle SES and in 33.7% (95% CI: 32.7–34.7) of those with high SES. These differences were statistically significant (χ2, p < 0.01). The median age in the lower, middle and upper SES groups was 28, 29 and 33 years, respectively. In total, the highest seroprevalence (94.4%) was observed in women of low SES aged 15–25 years, the lowest rate (30.0%) in women of high SES aged 31–35 years.
Discussion
Knowledge on age-specific CMV seroprevalence and the influence of several demographic factors on immunity are essential for the development of preventive measures. Cannon et al. [10] recently reviewed a great number of worldwide studies on CMV seroprevalence in women of reproductive age. Rates varied between 45 and 100%. His review also showed that in general, IgG seroprevalence was higher in women than men, in persons of lower SES than in those of middle/upper SES and in non-whites than in whites [10]. In Europe, seropositive rates in pregnant women and women of childbearing age ranged from 30 to 70% (see Table 4). In the present study, we found an overall prevalence in pregnancy of 42.3%, which is similar to all our former studies [9, 11, 12]. Lübeck et al., however, determined a higher seroprevalence of 60% in female non-pregnant patients (HIV-negative, aged 20–40 year) in the Goethe University Hospital in Frankfurt am Main [13]. An equal rate was already reported in a previous publication for the outpatient setting of the same hospital [14]. It may be due to a high proportion of immigrants among the patients (approx. 21–25%) [13]. Halwachs-Baumann et al. investigated 947 pregnant women in at the University Hospital at Graz in Austria and found a CMV seroprevalence of 51%, with no age-related differences [15].
The factors influencing seroprevalence are age [9, 11–14, 16–23], gender [13, 16, 21, 23], parity [18–20, 24], ethnicity [18–20, 23, 25, 26] and socioeconomic factors [9, 13, 17, 18, 23, 25, 27].
Unfortunately in our group of pregnant women, we had no information on their ethnicity. However, German birth statistic of the last 15 years revealed that 17–18% of puerperal women had foreign nationality [28]. The largest group came from Turkey, a country with a high CMV seroprevalence rate of >94% [29, 30]. In the adolescent group—the only group in our study with known ethnicity—those with non-German descent had a significant higher seropositive rate than those with German descent (67.4% versus 29.9%).
The often reported higher seroprevalence of women compared to men was confirmed by our results in bone marrow donors [13, 16, 21, 23]. This tendency—although statistically not significant—was also seen in our small group of adolescents with non-German descent.
Previous studies found an age-dependent increase of CMV seroprevalence [9, 11–14, 16–23]. This could be supported by our results in the group of female and male bone marrow donors and also in pregnant women older than 30 years.
Notably, young pregnant women (15–25 years) had an increased seropositive rate (55.6%) compared to older pregnant women and to age-matched female bone marrow donors (32.3%). In our previous publication, we also observed a higher seroprevalence rate of 59.5 and 55.1% in younger pregnant women aged 16–20 and 21–25 years, respectively, compared to 39.4–44.2% in women aged 26–40 years by investigating 1,033 blindly selected sera from antenatal screening [9]. This effect may be explained by different demographic factors in the various age groups of pregnant women. Since no data are available on ethnicity, one can only speculate on the reason behind this effect. Probably, the “young-age group” contains a higher proportion of women with foreign descent. Furthermore, according to the population statistics on women who delivered in 2009, those with foreign nationality and unmarried were overrepresented in the younger age groups [31]. In an earlier study in pregnant women (n = 512), Friese et al. already showed that CMV seroprevalence was markedly elevated in the younger age group (<20 years; 73%). They related it to the overrepresentation of women with low socioeconomic status (SES; 69%) as compared to the older age groups (≤30%, [17]). The authors defined SES by education, profession and place of residence, whereas many studies [9, 13, 27], including our own, used health insurance status as a rough indicator of SES. Our results confirmed the findings of various international and German studies showing that with increasing SES, the seropositive rates are lower. The most recent study from Frankfurt, Germany (n = 54,443), reported a higher seroprevalence of 60.1% in women with middle SES compared to 46.8% for women of upper SES [13]. The overall lower rate of seroprevalence in female and male bone marrow donors may be explained by the assumption that donors are mainly of German descent and belong to a higher income group. The latter is based on the fact that costs of registration and typing (50 €) are usually covered by the donors themselves.
In some recent studies, changes of CMV seroprevalence in different populations over up to two decades have been a matter of interest [13, 22, 23]. In another German study, a decline of seroprevalence between two decades (1988–1997 and 1998–2008) in HIV-negative hospitalized patients from 63.8 to 58.7% for women and from 63.5 to 55.5% for men was observed [13]. In a Spanish study, a similar decline from 90.3 to 79.1% has been reported in women aged 31–40 years between 1993 and 1999 [22]. In the United States, however, CMV seroprevalence across most age, sex and racial/ethnic groups showed no significant changes between 1988 and 1994 (n = 21,639) and 1999–2004 (n = 15,310) [23]. We observed a significant decrease of seroprevalence rates in pregnant women from 44.3 to 40.9% over the last 15 years (1996–2010), whereas median pregnancy age increased from 29 to 32 years. To our knowledge, there are no other publications on this subject.
The reasons for the decline of the CMV seroprevalence over the last 15 years in the present study are difficult to elucidate, since it is retrospective and ethnicity is not known. Some factors may have changed, like breastfeeding (low breastfeeding rates in the 1960 and 1970s in contrast to nowadays) or child-rearing practices. Their impact on seroprevalence can, however, not be proven. This can only be achieved by a prospective study design including a questionnaire asking for all important demographic data.
From our results, it is evident that in Germany, the highest susceptibility for primary CMV infection exists in pregnant women of middle age, German descent and middle to high SES. The main routes of acquisition are sexual contact in the younger age groups and contact with CMV-excreting children in women aged >25 years. The increased risk for seronegative multiparous women to acquire CMV from their own infants attending toddler groups or childcare facilities is well documented [32]. This is supported by our observation that in the group of primary infections in pregnancy, second parous women (one live-born child) are more frequent (61%) than nulliparous women (27%; no live-born child; unpublished data).
For prevention of primary infection today, only hygienic and behavioral measures are available [8, 33]. For CMV seronegative pregnant women, who work closely with children <3 years (e.g. as childcare providers or pediatric health care personnel), work release is recommended for total pregnancy based on the German Maternity Protection Act [34]. This is definitely in contrast to other West European countries and the USA, which emphasize only the importance of hygiene practices instead.
During the last few years, the knowledge and awareness of congenital CMV in the general German public has increased, and its public health burden has been recognized.
Despite valid methods for serology and virus detection, obligatory CMV antibody screening is presently not included in antenatal care, since not all preconditions like the availability of an efficient therapy and prophylaxis are fulfilled. Antiviral therapy with ganciclovir, which is used in symptomatic congenitally infected newborns, may have teratogenic effects and is, therefore, not recommended in pregnancy [35].
However, two further treatment options of primary CMV infection in pregnancy are currently the target of research: First of all, passive prophylaxis by application of CMV hyperimmunoglobulin to mother and fetus aimed to prevent fetal infection following primary infection and to treat disease manifestations in infected fetuses was investigated by the study of Nigro et al. [36]. The benefit of this therapeutic option is currently explored by two randomized controlled studies (Biotest 963 Multicenter Study and the blinded placebo-controlled CHIP-Study in Italy). However, women with primary CMV infection in early pregnancy, which cannot be included in the above mentioned studies, request for CMV hyperimmunoglobulin. From 2006 to 2010/2011, more than 200 of such pregnant women have been “off-label” treated with hyperimmunoglobulin after informed consent and were followed up in our institution (G. Enders, unpublished data).
The second treatment option preferred by French researchers is oral valaciclovir, which is less potent against CMV than valganciclovir, but has already been explored in pregnant women with HSV or VZV infection. Valaciclovir was applied to pregnant women with symptomatic CMV-infected fetuses at gestational week 22–34, who desired to continue pregnancy. Treatment achieved therapeutic aciclovir concentrations in the fetus and reduced viral load in fetal blood [37], but not in amniotic fluid. Based on the results of this pilot study, a further randomized placebo-controlled study was started in 2009 (planned completion date June 2013).
Abbreviations
- CMV:
-
Cytomegalovirus
- OD:
-
Optical density
- PEIU:
-
Paul-Ehrlich Institute Units
- 95% CI:
-
95% confidence intervals
- SES:
-
Socioeconomic status
References
Stagno S, Pass FR, Cloud G, Britt EJ, Henderson RE, Walton PD, Veren DA, Page F, Alford CA (1986) Primary cytomegalovirus infection in pregnancy. Incidence, transmission to the fetus, and clinical outcome. JAMA 256:1904–1908
Dollard SC, Grosse SD, Ross DS (2007) New estimates of the prevalence of neurological and sensory sequelae and mortality associated with congenital cytomegalovirus infection. Rev Med Virol 17(5):355–363
Fowler KB, Stagno S, Pass RF, Britt WJ, Boll TJ, Alford CA (1992) The outcome of congenital cytomegalovirus infection in relation to maternal antibody status. N Engl J Med 326(10):663–667
Scholz H (2000) Häufigkeit der konnatalen Zytomegalie in der Bundesrepublik Deutschland. Monatsschr Kinderheilkd 148:887–890
Hamprecht K, Abele H, Goelz R (2011) Tuebingen congenital CMV study: first epidemiological and diagnostic results. 13th International CMV/Betaherpesvirus workshop, Nuremberg, Germany
Stratton K, Durch J, Lawrence R (2001) Vaccines for the 21st century: a tool for decicion-making. National Academy Press, Washington, DC
Pass RF (2009) Development and evidence for efficacy of CMV glycoprotein B vaccine with MF59 adjuvant. J Clin Virol 46:73–76
Vauloup-Fellous C, Picone O, Cordier AG, Parent-du-Châtelet I, Senat MV, Frydman R, Grangeot-Keros L (2009) Does hygiene counseling have an impact on the rate of CMV primary infection during pregnancy? Results of a 3-year prospective study in a French hospital. J Clin Virol 46:49–53
Enders G, Bäder U, Bartelt U et al (2003) Zytomegalievirus—(CMV-) Durchseuchung und Häufigkeit von CMV-Primärinfektionen bei schwangeren Frauen in Deutschland. Bundesgesundheitsbl—Gesundheitsforsch—Gesundheitsschutz 46:426–432
Cannon MJ, Schmid DS, Hyde TB (2010) Review of cytomegalovirus seroprevalence and demographic characteristics associated with infection. Rev Med Virol 20:202–213
Enders G (1985) Vergleich verschiedener Methoden zum Zytomegalieantikörpernachweis. In: Luthardt T (Ersg) Transfusionsbedingte Zytomegalievirusinfectionen, Steinkopff, Darmstadt, pp 53–67
Enders G (1986) Diagnosis of cytomegalovirus infection. In Simon C, Wilkinson P (eds) Diagnosis of infectious diseases—new aspects, 1st edn. Schattauer, Stuttgart, pp 225–235
Lübeck PR, Doerr HW, Rabenau HF (2010) Epidemiology of human cytomegalovirus (HCMV) in an urban region of Germany: what has changed? Med Microbiol Immunol 199(1):53–60
Just-Nübling G, Korn S, Ludwig B, Stephan C, Doerr HW, Preiser W (2003) Primary cytomegalovirus infection in an outpatient setting—laboratory markers and clinical aspects. Infection 31(5):318–323
Halwachs-Baumann G, Genser B (2003) Prävalenz von CMV IgG bei Schwangeren im Einzugsgebiet LKH/Universitätsklinikum Graz. In: Halwachs-Baumann G, Genser B (eds) Die konnatale Zytomegalievirusinfektion, 1st edn. Springer, Wien, pp 43–44
Hecker M, Qiu D, Marquardt K, Bein G, Hackstein H (2004) Continuous cytomegalovirus seroconversion in a large group of healthy blood donors. Vox Sang 86(1):41–44
Friese K, Beichert M, Hof H et al (1991) Incidence of congenital infections. Geburtshilfe Frauenheilkunde 51:890–896
Tookey PA, Ades AE, Peckham CS (1992) Cytomegalovirus prevalence in pregnant women: the influence of parity. Arch Dis Childh 67:779–783
Gambarotto K, Ranger-Rogez S, Aubard Y, Piver P, Duffetelle B, Delpeyroux C, Roussanne MC, Nicot T, Denis F (1997) Primary cytomegalovirus infection and pregnant women: epidemiological study on 1100 women at Limoges. Pathol Biol (Paris) 45(6):453–461
Gratacap-Cavallier B, Bosson JL, Morand P, Dutertre N, Chanzy B, Jouk PS, Vandekerckhove C, Cart-Lamy P, Seigneurin JM (1998) Cytomegalovirus seroprevalence in French pregnant women: parity and place of birth as major predictive factors. Eur J Epidemiol 14:147–152
de Mattia D, Stroffolini T, Arista S, Pistoia D, Giammanco A, Maggio M, Chiaramonte M, Moschen ME, Mura I, Rigo G et al (1991) Prevalence of cytomegalovirus infection in Italy. Epidemiol Infect 107(2):421–427
de Ory F, Ramírez R, García Comas L, León P, Sagües MJ, Sanz JC (2004) Is there a change in cytomegalovirus seroepidemiology in Spain? Eur J Epidemiol 19(1):85–89
Bate SL, Dollard SC, Cannon MJ (2010) Cytomegalovirus seroprevalence in the United States: the national health and nutrition examination surveys, 1988–2004. Clin Infect Dis 50(11):1439–1447
Eskild A, Jenum PA, Bruu AL (2005) Maternal antibodies against cytomegalovirus in pregnancy and the risk of fetal death and low birth weight. Acta Obstet Gynecol Scand 84:1035–1041
Knowles SJ, Grundy K, Cahill I, Cafferkey MT, Geary M (2005) Low cytomegalovirus sero-prevalence in Irish pregnant women. Ir Med J 98:210–212
Gaytant MA, Galama JM, Semmekrot BA, Melchers WJ, Sporken JM, Oosterbaan HP, van Dop PA, Huisman A, Merkus HM, Steegers EA (2005) The incidence of congenital cytomegalovirus infections in The Netherlands. J Med Virol 76:71–75
Mustakangas P, Sarna S, Ämmäiä P, Muttilainen M, Koskela P, Koskiniemi M (2000) Human cytomegalovirus seroprevalence in three socioeconomically different urban areas during the first trimester: a population-based cohort study. Int J Epidemiol 29:587–591
Statistical Office For the Federal Republic of Germany, Wiesbaden; www-genesis.destatis.de
Ocak S, Zeteroglu S, Ozer C, Dolapcioglu K, Gungoren A (2007) Seroprevalence of Toxoplasma gondii, rubella and cytomegalovirus among pregnant women in southern Turkey. Scand J Infect Dis 39(3):231–234
Tamer GS, Dundar D, Caliskan E (2009) Seroprevalence of Toxoplasma gondii, rubella and cytomegalovirus among pregnant women in western region of Turkey. Clin Invest Med 32(1):E43–E47
Federal Statistical Office Wiesbaden; Statistical Yearbook (2011) For the Federal Republic of Germany
Adler SP (1991) Cytomegalovirus and child day care: risk factors for maternal infection. Pediatr Infect Dis J 10(8):590–594
Adler SP, Finney JW, Manganello AM, Best AM (2004) Prevention of child-to-mother transmission of cytomegalovirus among pregnant women. J Pediatr 145:485–491
Enders G (2003) Infektionsgefährdung: Mutterschutz im Krankenhaus—eine Übersicht. Arbeitsmed Sozialmed Umweltmed 38:324–335
Enders G (2006) Labormedizinische Aspekte bei Cytomegalie und Toxoplasmose. gynäkologie + geburtshilfe 1:24–28
Nigro G, Adler SP, La Torre R, Best AM (2005) Congenital Cytomegalovirus Collaborating Group. Passive immunization during pregnancy for congenital cytomegalovirus infection. N Engl J Med 353:1350–1362
Jacquemard F, Yamamoto M, Costa JM, Romand S, Jaqz-Aigrain E, Dejean A, Daffos F, Ville Y (2007) Maternal administration of valaciclovir in symptomatic intrauterine cytomegalovirus infection. BJOG 114(9):1113–1121
Engman ML, Malm G, Engstrom L, Petersson K, Karltorp E, Tear Fahnehjelm K, Uhlen I, Guthenberg C, Lewensohn-Fuchs I (2008) Congenital CMV infection: prevalence in newborns and the impact on hearing deficit. Scand J Infect Dis 40(11–12):935–942
Alanen A, Kahala K, Vahlberg T, Koskela P, Vainionpää R (2005) Seroprevalence, incidence of prenatal infections and reliability of maternal history of varicella zoster virus, cytomegalovirus, herpes simplex virus and parvovirus B19 infection in South-Western Finland. BJOG 12(1):50–56
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Enders, G., Daiminger, A., Lindemann, L. et al. Cytomegalovirus (CMV) seroprevalence in pregnant women, bone marrow donors and adolescents in Germany, 1996–2010. Med Microbiol Immunol 201, 303–309 (2012). https://doi.org/10.1007/s00430-012-0232-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00430-012-0232-7