Abstract
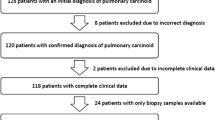
Optimal histopathological analysis of biopsies from metastases of neuroendocrine tumor (NET) of the lung requires more than morphology only. Additional parameters such as Ki-67 labeling index are required for adequate diagnosis, but few studies have compared reproducibility of different counting protocols and modalities of reporting on biopsies of lung NET. We compared the results of four different manual counting techniques to establish Ki-67 LI. On 47 paired biopsies and surgical specimens from 22 typical carcinoids (TCs), 14 atypical carcinoids (ACs), six large cell neuroendocrine carcinomas (LCNECs), and five small cell carcinomas (SCCs) immunohistochemical staining of Ki-67 antigen was performed. We counted, in regions of highest nuclear staining (HSR), a full ×40-high-power field (diameter = 0.55 mm), 500 or 2000 cells, or 2 mm2 surface area, including the HSR or the entire biopsy fragment(s). Mitoses and necrosis were evaluated in an area of 2 mm2 or the entire biopsy fragment(s). Between the four counting methods, no differences in Ki-67 LI were observed. However, a Ki-67 LI higher than 5% was found in only four cases when in an HSR, 500 cells were counted (18%), five (23%) when in an HSR 2000 cells were counted, four (18%) when 2 mm2 were counted, and one (5%) TC case when the entire biopsy was counted. A 20% cutoff distinguished TC and AC from LCNEC and SCC with 100% specificity and sensitivity, while mitoses and necrosis failed to a large extent. Ki-67 LI in biopsy samples was concordant with that in resection specimens when 2000 cells, 2 mm2, or the entire biopsy fragment(s) were counted. Our results are important for clinical management of patients with metastases of a lung NET.


Similar content being viewed by others
References
Caplin ME, Baudin E, Ferolla P, Filosso P, Garcia-Yuste M, Lim E, Oberg K, Pelosi G, Perren A, Rossi RE, Travis WD, ENETS consensus conference participants (2015) Pulmonary neuroendocrine (carcinoid) tumors: European neuroendocrine tumor society expert consensus and recommendations for best practice for typical and atypical pulmonary carcinoids. Ann Oncol 26:1604–1620
Rekhtman N (2010) Neuroendocrine tumors of the lung: an update. Arch Pathol Lab Med 134:1628–1638
Travis W, Brambilla E, Burke A, Marx A, Nicholson A, (2015) WHO classification of tumours of the lung, pleura, thymus and heart. Fourth Ed. edn. IARC Press, Lyon
Pelosi G, Fabbri A, Cossa M, Sonzogni A, Valeri B, Righi L, Papotti M (2015) What clinicians are asking pathologists when dealing with lung neuroendocrine neoplasms? Semin Diagn Pathol 32:469–479
Pelosi G, Hiroshima K, Mino-Kenudson M (2014) Controversial issues and new discoveries in lung neuroendocrine tumors. Diagn Histopathol 20:392–397
Pelosi G, Papotti M, Rindi G, Scarpa A (2014) Unraveling tumor grading and genomic landscape in lung neuroendocrine tumors. Endocr Pathol 25(2):151–164
Travis W, Brambilla E, Muller-Hermelink H, Harris C (2004) Tumours of the lung, pleura, thymus and heart. IARC Press, Lyon
Travis W, Colby T, Corrin B, Shimosato Y, Brambilla E (1999) Histological typing of lung and pleural tumours. Springer, Berlin Heidelberg New York
Axiotis C (2002) The neuroendocrine lung. In: Li Volsi V, Asa S (eds) Endocrine pathology. Churchill Livingstone, New York Edinburgh, pp 261–296
Capella C, Heitz PU, Hofler H, Solcia E, Kloppel G (1995) Revised classification of neuroendocrine tumours of the lung, pancreas and gut. Virchows Arch 425:547–560
Huang Q, Muzitansky A, Mark EJ (2002) Pulmonary neuroendocrine carcinomas. A review of 234 cases and a statistical analysis of 50 cases treated at one institution using a simple clinicopathologic classification. Arch Pathol Lab Med 126:545–553
Moran CA, Suster S, Coppola D, Wick MR (2009) Neuroendocrine carcinomas of the lung: a critical analysis. Am J Clin Pathol 131:206–221
den Bakker MA, Thunnissen FB (2013) Neuroendocrine tumours—challenges in the diagnosis and classification of pulmonary neuroendocrine tumours. J Clin Pathol 66:862–869
den Bakker MA, Willemsen S, Grunberg K, Noorduijn LA, van Oosterhout MF, van Suylen RJ, Timens W, Vrugt B, Wiersma-van Tilburg A, Thunnissen FB (2010) Small cell carcinoma of the lung and large cell neuroendocrine carcinoma interobserver variability. Histopathology 56:356–363
Ha SY, Han J, Kim WS, Suh BS, Roh MS (2012) Interobserver variability in diagnosing high-grade neuroendocrine carcinoma of the lung and comparing it with the morphometric analysis. Korean J Pathol 46:42–47
Marchevsky AM, Gal AA, Shah S, Koss MN (2001) Morphometry confirms the presence of considerable nuclear size overlap between "small cells" and "large cells" in high-grade pulmonary neuroendocrine neoplasms. Am J Clin Pathol 116:466–472
Swarts DR, van Suylen RJ, den Bakker MA, van Oosterhout MF, Thunnissen FB, Volante M, Dingemans AM, Scheltinga MR, Bootsma GP, Pouwels HM, van den Borne BE, Ramaekers FC, Speel EJ (2014) Interobserver variability for the WHO classification of pulmonary carcinoids. Am J Surg Pathol 38:1429–1436
Travis WD, Gal AA, Colby TV, Klimstra DS, Falk R, Koss MN (1998) Reproducibility of neuroendocrine lung tumor classification. Hum Pathol 29:272–279
Warth A, Fink L, Fisseler-Eckhoff A, Jonigk D, Keller M, Ott G, Rieker RJ, Sinn P, Soder S, Soltermann A, Willenbrock K, Weichert W (2013) Interobserver agreement of proliferation index (Ki-67) outperforms mitotic count in pulmonary carcinoids. Virchows Arch 462:507–513
Derks JL, Speel EJ, Thunnissen E, van Suylen RJ, Buikhuisen WA, van Velthuysen ML, Dingemans AM (2016) Neuroendocrine cancer of the lung: a diagnostic puzzle. J Thorac Oncol 11:e35–e38
Pusceddu S, Lo Russo G, Macerelli M, Proto C, Vitali M, Signorelli D, Ganzinelli M, Scanagatta P, Duranti L, Trama A, Buzzoni R, Pelosi G, Pastorino U, de Braud F, Garassino MC (2016) Diagnosis and management of typical and atypical lung carcinoids. Crit Rev Oncol Hematol 100:167–176
Gustafsson BI, Kidd M, Chan A, Malfertheiner MV, Modlin IM (2008) Bronchopulmonary neuroendocrine tumors. Cancer 113:5–21
Yao JC, Hassan M, Phan A, Dagohoy C, Leary C, Mares JE, Abdalla EK, Fleming JB, Vauthey JN, Rashid A, Evans DB (2008) One hundred years after "carcinoid": epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol 26:3063–3072
Rindi G, Falconi M, Klersy C, Albarello L, Boninsegna L, Buchler MW, Capella C, Caplin M, Couvelard A, Doglioni C, Delle Fave G, Fischer L, Fusai G, de Herder WW, Jann H, Komminoth P, de Krijger RR, La Rosa S, Luong TV, Pape U, Perren A, Ruszniewski P, Scarpa A, Schmitt A, Solcia E, Wiedenmann B (2012) TNM staging of neoplasms of the endocrine pancreas: results from a large international cohort study. J Natl Cancer Inst 104:764–777
Rindi G, Kloppel G, Alhman H, Caplin M, Couvelard A, de Herder WW, Erikssson B, Falchetti A, Falconi M, Komminoth P, Korner M, Lopes JM, McNicol AM, Nilsson O, Perren A, Scarpa A, Scoazec JY, Wiedenmann B (2006) TNM staging of foregut (neuro)endocrine tumors: a consensus proposal including a grading system. Virchows Arch 449:395–401
Rindi G, Petrone G, Inzani F (2014) The 2010 WHO classification of digestive neuroendocrine neoplasms: a critical appraisal four years after its introduction. Endocr Pathol 25:186–192
Sobin L, Gospodarowicz M, Wittekind C (2010) TNM classification of malignant tumours. Wiley-Blackwell, New York
Pelosi G, Bresaola E, Bogina G, Pasini F, Rodella S, Castelli P, Iacono C, Serio G, Zamboni G (1996) Endocrine tumors of the pancreas: Ki-67 immunoreactivity on paraffin sections is an independent predictor for malignancy: a comparative study with proliferating-cell nuclear antigen and progesterone receptor protein immunostaining, mitotic index, and other clinicopathologic variables. Hum Pathol 27:1124–1134
Pelosi G, Zamboni G (1996) Proliferation markers and their uses in the study of endocrine tumors. Endocr Pathol 7:103–119
Pelosi G, Rindi G, Travis WD, Papotti M (2014) Ki-67 antigen in lung neuroendocrine tumors: unraveling a role in clinical practice. J Thorac Oncol 9:273–284
Pelosi G, Rodriguez J, Viale G, Rosai J (2005) Typical and atypical pulmonary carcinoid tumor overdiagnosed as small-cell carcinoma on biopsy specimens: a major pitfall in the management of lung cancer patients. Am J Surg Pathol 29:179–187
Rindi G, Klersy C, Inzani F, Fellegara G, Ampollini L, Ardizzoni A, Campanini N, Carbognani P, De Pas TM, Galetta D, Granone PL, Righi L, Rusca M, Spaggiari L, Tiseo M, Viale G, Volante M, Papotti M, Pelosi G (2014) Grading the neuroendocrine tumors of the lung: an evidence-based proposal. Endocr Relat Cancer 21:1–16
Pelosi G, Pattini L, Morana G, Fabbri A, Faccinetto A, Fazio N, Valeri B, Sonzogni A (2016) Grading lung neuroendocrine tumors: controversies in search of a solution. Neuroendocrinology (submitted)
Yang Z, Tang LH, Klimstra DS (2013) Gastroenteropancreatic neuroendocrine neoplasms: historical context and current issues. Semin Diagn Pathol 30:186–196
Travis WD, Brambilla E, Noguchi M, Nicholson AG, Geisinger K, Yatabe Y, Ishikawa Y, Wistuba I, Flieder DB, Franklin W, Gazdar A, Hasleton PS, Henderson DW, Kerr KM, Petersen I, Roggli V, Thunnissen E, Tsao M (2013) Diagnosis of lung cancer in small biopsies and cytology: implications of the 2011 International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society classification. Arch Pathol Lab Med 137:668–684
Pelosi G, Fabbri A, Bianchi F, Maisonneuve P, Rossi G, Barbareschi M, Graziano P, Cavazza A, Rekhtman N, Pastorino U, Scanagatta P, Papotti M (2012) DeltaNp63 (p40) and thyroid transcription factor-1 immunoreactivity on small biopsies or cellblocks for typing non-small cell lung cancer: a novel two-hit, sparing-material approach. J Thorac Oncol 7:281–290
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1:307–310
Gridelli C, Rossi A, Airoma G, Bianco R, Costanzo R, Daniele B, Chiara GD, Grimaldi G, Irtelli L, Maione P, Morabito A, Piantedosi FV, Riccardi F (2013) Treatment of pulmonary neuroendocrine tumours: state of the art and future developments. Cancer Treat Rev 39:466–472
Swarts DR, Van Neste L, Henfling ME, Eijkenboom I, Eijk PP, van Velthuysen ML, Vink A, Volante M, Ylstra B, Van Criekinge W, van Engeland M, Ramaekers FC, Speel EJ (2013) An exploration of pathways involved in lung carcinoid progression using gene expression profiling. Carcinogenesis 34:2726–2737
Walts AE, Ines D, Marchevsky AM (2012) Limited role of Ki-67 proliferative index in predicting overall short-term survival in patients with typical and atypical pulmonary carcinoid tumors. Mod Pathol 25:1258–1264
Costes V, Marty-Ane C, Picot MC, Serre I, Pujol JL, Mary H, Baldet P (1995) Typical and atypical bronchopulmonary carcinoid tumors: a clinicopathologic and KI-67-labeling study. Hum Pathol 26:740–745
Fazio N, Granberg D, Grossman A, Saletan S, Klimovsky J, Panneerselvam A, Wolin EM (2013) Everolimus plus octreotide long-acting repeatable in patients with advanced lung neuroendocrine tumors: analysis of the phase 3, randomized, placebo-controlled RADIANT-2 study. Chest 143:955–962
Ferolla P (2015) Medical therapy of pulmonary neuroendocrine neoplasms: targeted, symptomatic and chemotherapy. Front Horm Res 44:193–197
Righi L, Volante M, Rapa I, Vatrano S, Pelosi G, Papotti M (2014) Therapeutic biomarkers in lung neuroendocrine neoplasia. Endocr Pathol 25:371–377
Yao JC, Fazio N, Singh S, Buzzoni R, Carnaghi C, Wolin E, Tomasek J, Raderer M, Lahner H, Voi M, Pacaud LB, Rouyrre N, Sachs C, Valle JW, Delle Fave G, Van Cutsem E, Tesselaar M, Shimada Y, Oh DY, Strosberg J, Kulke MH, Pavel ME, Rad001 in Advanced Neuroendocrine Tumours FTSG (2016) Everolimus for the treatment of advanced, non-functional neuroendocrine tumours of the lung or gastrointestinal tract (RADIANT-4): a randomised, placebo-controlled, phase 3 study. Lancet 387:968–977
Naidoo J, Santos-Zabala ML, Iyriboz T, Woo KM, Sima CS, Fiore JJ, Kris MG, Riely GJ, Lito P, Iqbal A, Veach S, Smith-Marrone S, Sarkaria IS, Krug LM, Rudin CM, Travis WD, Rekhtman N, Pietanza MC (2016) Large cell neuroendocrine carcinoma of the lung: clinico-pathologic features, treatment, and outcomes. Clin Lung Cancer
Rekhtman N, Pietanza MC, Hellmann MD, Naidoo J, Arora A, Won H, Halpenny DF, Wang H, Tian SK, Litvak AM, Paik PK, Drilon A, Socci N, Poirier JT, Shen R, Berger MF, Moreira AL, Travis WD, Rudin CM, Ladanyi M (2016) Next-generation sequencing of pulmonary large cell neuroendocrine carcinoma reveals small cell carcinoma-like and non-small cell carcinoma-like subsets. Clin Cancer Res
Swarts DR, Henfling ME, Van Neste L, van Suylen RJ, Dingemans AM, Dinjens WN, Haesevoets A, Rudelius M, Thunnissen E, Volante M, Van Criekinge W, van Engeland M, Ramaekers FC, Speel EJ (2013) CD44 and OTP are strong prognostic markers for pulmonary carcinoids. Clin Cancer Res 19:2197–2207
Swarts DR, Ramaekers FC, Speel EJ (2012) Molecular and cellular biology of neuroendocrine lung tumors: evidence for separate biological entities. Biochim Biophys Acta 1826:255–271
Swarts DR, Scarpa A, Corbo V, Van Criekinge W, van Engeland M, Gatti G, Henfling ME, Papotti M, Perren A, Ramaekers FC, Speel EJ, Volante M (2014) MEN1 gene mutation and reduced expression are associated with poor prognosis in pulmonary carcinoids. J Clin Endocrinol Metab 99:E374–E378
Basturk O, Tang L, Hruban RH, Adsay V, Yang Z, Krasinskas AM, Vakiani E, La Rosa S, Jang KT, Frankel WL, Liu X, Zhang L, Giordano TJ, Bellizzi AM, Chen JH, Shi C, Allen P, Reidy DL, Wolfgang CL, Saka B, Rezaee N, Deshpande V, Klimstra DS (2014) Poorly differentiated neuroendocrine carcinomas of the pancreas: a clinicopathologic analysis of 44 cases. Am J Surg Pathol
Basturk O, Yang Z, Tang LH, Hruban RH, Adsay V, McCall CM, Krasinskas AM, Jang KT, Frankel WL, Balci S, Sigel C, Klimstra DS (2015) The high-grade (WHO G3) pancreatic neuroendocrine tumor category is morphologically and biologically heterogenous and includes both well differentiated and poorly differentiated neoplasms. Am J Surg Pathol 39:683–690
Hijioka S, Hosoda W, Mizuno N, Hara K, Imaoka H, Bhatia V, Mekky MA, Tajika M, Tanaka T, Ishihara M, Yogi T, Tsutumi H, Fujiyoshi T, Sato T, Hieda N, Yoshida T, Okuno N, Shimizu Y, Yatabe Y, Niwa Y, Yamao K (2015) Does the WHO 2010 classification of pancreatic neuroendocrine neoplasms accurately characterize pancreatic neuroendocrine carcinomas? J Gastroenterol 50:564–572
Sorbye H, Welin S, Langer SW, Vestermark LW, Holt N, Osterlund P, Dueland S, Hofsli E, Guren MG, Ohrling K, Birkemeyer E, Thiis-Evensen E, Biagini M, Gronbaek H, Soveri LM, Olsen IH, Federspiel B, Assmus J, Janson ET, Knigge U (2013) Predictive and prognostic factors for treatment and survival in 305 patients with advanced gastrointestinal neuroendocrine carcinoma (WHO G3): the NORDIC NEC study. Ann Oncol 24:152–160
Tang LH, Untch BR, Reidy DL, O’Reilly E, Dhall D, Jih L, Basturk O, Allen PJ, Klimstra DS (2016) Well-differentiated neuroendocrine tumors with a morphologically apparent high-grade component: a pathway distinct from poorly differentiated neuroendocrine carcinomas. Clin Cancer Res 22:1011–1017
Velayoudom-Cephise FL, Duvillard P, Foucan L, Hadoux J, Chougnet CN, Leboulleux S, Malka D, Guigay J, Goere D, Debaere T, Caramella C, Schlumberger M, Planchard D, Elias D, Ducreux M, Scoazec JY, Baudin E (2013) Are G3 ENETS neuroendocrine neoplasms heterogeneous? Endocr Relat Cancer 20:649–657
Fernandez-Cuesta L, McKay JD (2016) Genomic architecture of lung cancers. Curr Opin Oncol 28:52–57
Seidel D, Zander T, Heukamp L, Peifer M, Bos M, Fernández-Cuesta L, Leenders F, Lu X, Ansén SGM, Nguyen C, Berg J, Russell P, Wainer Z, Schildhaus HU, Rogers TM, Solomon B, Pao W, Carter SL, Getz G, Hayes D, Wilkerson MD, Thunnissen E, Travis WD, Perner S, Wright G, Brambilla E, Büttner R, Wolf J, Thomas RK, Gabler F, Wilkening I, Müller C, Dahmen I, Menon R, König K, Albus K, Merkelbach-Bruse S, Fassunke J, Schmitz K, Kuenstlinger H, Kleine MA, Binot E, Querings S, Altmüller J, Bäßmann I, Nürnberg P, Schneider PM, Bogus M, Büttner R, Perner S, Russell P, Thunnissen E, Travis WD, Brambilla E, Soltermann A, Moch H, Brustugun OT, Solberg S, Lund-Iversen M, Helland Å, Muley T, Hoffmann H, Schnabel PA, Chen Y, Groen H, Timens W, Sietsma H, Clement JH, Weder W, Sänger J, Stoelben E, Ludwig C, Engel-Riedel W, Smit E, Heideman DA, Snijders PJ, Nogova L, Sos ML, Mattonet C, Töpelt K, Scheffler M, Goekkurt E, Kappes R, Krüger S, Kambartel K, Behringer D, Schulte W, Galetke W, Randerath W, Heldwein M, Schlesinger A, Serke M, Hekmat K, Frank KF, Schnell R, Reiser M, Hünerlitürkoglu AN, Schmitz S, Meffert L, Ko YD, Litt-Lampe M, Gerigk U, Fricke R, Besse B, Brambilla C, Lantuejoul S, Lorimier P, Moro-Sibilot D, Cappuzzo F, Ligorio C, Damiani S, Field JK, Hyde R, Validire P, Girard P, Muscarella LA, Fazio VM, Hallek M, Soria JC, Carter SL, Getz G, Hayes D, Wilkerson MD, Achter V, Lang U, Seidel D, Zander T, Heukamp LC, Peifer M, Bos M, Pao W, Travis WD, Brambilla E, Büttner R, Wolf J, Thomas RK, Büttner R, Wolf J, Thomas RK (2013) A genomics-based classification of human lung tumors. Sci Transl Med 5:209ra153
Karlsson A, Brunnstrom H, Lindquist KE, Jirstrom K, Jonsson M, Rosengren F, Reutersward C, Cirenajwis H, Borg A, Jonsson P, Planck M, Jonsson G, Staaf J (2015) Mutational and gene fusion analyses of primary large cell and large cell neuroendocrine lung cancer. Oncotarget 6:22028–22037
Travis WD, Linnoila RI, Tsokos MG, Hitchcock CL, Cutler GB Jr, Nieman L, Chrousos G, Pass H, Doppman J (1991) Neuroendocrine tumors of the lung with proposed criteria for large-cell neuroendocrine carcinoma. An ultrastructural, immunohistochemical, and flow cytometric study of 35 cases. Am J Surg Pathol 15:529–553
Travis WD, Rush W, Flieder DB, Falk R, Fleming MV, Gal AA, Koss MN (1998) Survival analysis of 200 pulmonary neuroendocrine tumors with clarification of criteria for atypical carcinoid and its separation from typical carcinoid. Am J Surg Pathol 22:934–944
Travis WD, Brambilla E, Nicholson AG, Yatabe Y, Austin JH, Beasley MB, Chirieac LR, Dacic S, Duhig E, Flieder DB, Geisinger K, Hirsch FR, Ishikawa Y, Kerr KM, Noguchi M, Pelosi G, Powell CA, Tsao MS, Wistuba I (2015) The 2015 World Health Organization classification of lung tumors: impact of genetic, clinical and radiologic advances since the 2004 classification. J Thorac Oncol 10:1243–1260
Aslan DL, Gulbahce HE, Pambuccian SE, Manivel JC, Jessurun J (2005) Ki-67 immunoreactivity in the differential diagnosis of pulmonary neuroendocrine neoplasms in specimens with extensive crush artifact. Am J Clin Pathol 123:874–878
Granberg D, Wilander E, Oberg K, Skogseid B (2000) Prognostic markers in patients with typical bronchial carcinoid tumors. J Clin Endocrinol Metab 85:3425–3430
Li F, Ye B, Hong L, Xu H, Fishbein MC (2011) Epigenetic modifications of histone h4 in lung neuroendocrine tumors. Appl Immunohistochem Mol Morphol 19:389–394
Lin O, Olgac S, Green I, Zakowski MF, Klimstra DS (2003) Immunohistochemical staining of cytologic smears with MIB-1 helps distinguish low-grade from high-grade neuroendocrine neoplasms. Am J Clin Pathol 120:209–216
Skov BG, Krasnik M, Lantuejoul S, Skov T, Brambilla E (2008) Reclassification of neuroendocrine tumors improves the separation of carcinoids and the prediction of survival. J Thorac Oncol 3:1410–1415
Van Eeden S, Quaedvlieg PF, Taal BG, Offerhaus GJ, Lamers CB, Van Velthuysen ML (2002) Classification of low-grade neuroendocrine tumors of midgut and unknown origin. Hum Pathol 33:1126–1132
Zheng G, Ettinger DS, Maleki Z (2013) Utility of the quantitative Ki-67 proliferation index and CD56 together in the cytologic diagnosis of small cell lung carcinoma and other lung neuroendocrine tumors. Acta Cytol 57:281–290
Pelosi G, Zamboni G, Doglioni C, Rodella S, Bresaola E, Iacono C, Serio G, Iannucci A, Scarpa A (1992) Immunodetection of proliferating cell nuclear antigen assesses the growth fraction and predicts malignancy in endocrine tumors of the pancreas. Am J Surg Pathol 16:1215–1225
Das-Neves-Pereira JC, Bagan P, Milanez-de-Campos JR, Capelozzi VL, Danel C, Jatene FB, Bernaudin JF, Riquet M (2008) Individual risk prediction of nodal and distant metastasis for patients with typical bronchial carcinoid tumors. Eur J Cardiothorac Surg 34:473–477 discussion 477-8
Helpap B, Kollermann J (2001) Immunohistochemical analysis of the proliferative activity of neuroendocrine tumors from various organs. Are there indications for a neuroendocrine tumor-carcinoma sequence? Virchows Arch 438:86–91
Pelosi G, Pasini F, Fraggetta F, Pastorino U, Iannucci A, Maisonneuve P, Arrigoni G, De Manzoni G, Bresaola E, Viale G (2003) Independent value of fascin immunoreactivity for predicting lymph node metastases in typical and atypical pulmonary carcinoids. Lung Cancer 42:203–213
Pelosi G, Pasini F, Sonzogni A, Maffini F, Maisonneuve P, Iannucci A, Terzi A, De Manzoni G, Bresaola E, Viale G (2003) Prognostic implications of neuroendocrine differentiation and hormone production in patients with stage I nonsmall cell lung carcinoma. Cancer 97:2487–2497
Tsuta K, Liu DC, Kalhor N, Wistuba II, Moran CA (2011) Using the mitosis-specific marker anti-phosphohistone H3 to assess mitosis in pulmonary neuroendocrine carcinomas. Am J Clin Pathol 136:252–259
Zahel T, Krysa S, Herpel E, Stenzinger A, Goeppert B, Schirmacher P, Hoffmann H, Schnabel PA, Warth A (2012) Phenotyping of pulmonary carcinoids and a Ki-67-based grading approach. Virchows Arch 460:299–308
Hamanaka W, Motoi N, Ishikawa S, Ushijima M, Inamura K, Hatano S, Uehara H, Okumura S, Nakagawa K, Nishio M, Horai T, Aburatani H, Matsuura M, Iwasaki A, Ishikawa Y (2014) A subset of small cell lung cancer with low neuroendocrine expression and good prognosis: a comparison study of surgical and inoperable cases with biopsy. Hum Pathol 45:1045–1056
Yang Z, Tang LH, Klimstra DS (2011) Effect of tumor heterogeneity on the assessment of Ki67 labeling index in well-differentiated neuroendocrine tumors metastatic to the liver: implications for prognostic stratification. Am J Surg Pathol 35:853–860
Tang LH, Gonen M, Hedvat C, Modlin IM, Klimstra DS (2012) Objective quantification of the Ki67 proliferative index in neuroendocrine tumors of the gastroenteropancreatic system: a comparison of digital image analysis with manual methods. Am J Surg Pathol 36:1761–1770
Acknowledgements
This work was supported by Novartis Novartis Farma Italia, Milan, Italy. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript, which are the responsibilities of the authors only. The paper has been professionally proofread by PRS (Proof-Reading-Service.com Ltd., Devonshire Business Centre, Works Road, Letchworth Garden City, Herts SG6 1GJ, UK).
This work is dedicated to the memory of Carlotta, an extraordinarily lively girl who untimely died of cancer in the prime of life.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethics
The study was approved by the independent ethics committee of the National Tumor Institute IRCCS Foundation, Milan, Italy (accession number INT-18/16). All patients gave written consent for diagnosis and research activities when they were admitted to the hospital.
Electronic supplementary material
Supplemental Material A
Antibody panel used in the current study: all immunoreactions were performed using Envision Flex + DAKO (Flex Plus Polymers with horseradish peroxidase and 3–3′-diaminobenzidine), Dako, Glostrup Denmark. (DOCX 44 kb)
Supplemental Material B
Intraclass correlation coefficient analysis between biopsy samples and surgical specimens. (DOCX 77 kb)
Supplemental Material C
Deming regression on the left and Bland-Altman plots on the right for the evaluation of Ki-67 LI on 500 cells, chromogranin A (%), synaptophysin (%) and mitotic count on 2 mm2 on pre-surgical biopsy samples against surgical specimens. (GIF 3 kb)
Rights and permissions
About this article
Cite this article
Fabbri, A., Cossa, M., Sonzogni, A. et al. Ki-67 labeling index of neuroendocrine tumors of the lung has a high level of correspondence between biopsy samples and surgical specimens when strict counting guidelines are applied. Virchows Arch 470, 153–164 (2017). https://doi.org/10.1007/s00428-016-2062-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-016-2062-2