Abstract
Background
Although laparoscopic cholecystectomy is recommended as standard treatment for acute cholecystitis, in 10–30 % a conversion to open cholecystectomy is required. Among some surgeons, this is still perceived as a “complication.” The aim of our study was to define characteristics and outcome of patients with acute cholecystitis undergoing conversion cholecystectomy.
Methods
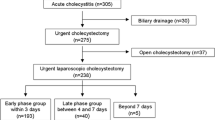
Over a 9-year period, 464 consecutive patients undergoing cholecystectomy for acute cholecystitis were analyzed for demographic, preoperative, intraoperative, histopathological, and laboratory findings and surgical outcome parameters.
Results
Patients with conversion cholecystectomy were characterized by younger age, lower American Society of Anesthesiologists (ASA) score, and less cardiac comorbidities compared to patients with primary open cholecystectomy. Severity of inflammation on the clinical and histopathological level was similar and comparable. Overall complication rate, mortality, and median hospital stay were significantly lower compared to those of primary open cholecystectomy group.
Conclusions
There are no disadvantages for patients undergoing conversion cholecystectomy compared to primary open cholecystectomy. The outcome is influenced by general condition and comorbidities rather than by the surgical approach. Underlying fear of conversion should not avoid a laparoscopic approach in patients with acute cholecystitis.

Similar content being viewed by others
References
Gutt CN et al (2013) Acute cholecystitis: early versus delayed cholecystectomy, a multicenter randomized trial (ACDC Study, NCT00447304). Ann Surg 258(3):385–393
Strasberg SM (2008) Clinical practice. Acute calculous cholecystitis. N Engl J Med 358(26):2804–2811
Yokoe M et al (2012) New diagnostic criteria and severity assessment of acute cholecystitis in revised Tokyo guidelines. J Hepatobiliary Pancreat Sci 19(5):578–585
Yokoe M et al (2013) TG13 diagnostic criteria and severity grading of acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci 20(1):35–46
Takada T et al (2013) TG13: updated Tokyo guidelines for the management of acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci 20(1):1–7
Gadacz TR, Talamini MA (1991) Traditional versus laparoscopic cholecystectomy. Am J Surg 161(3):336–338
van der Steeg HJ et al (2011) Risk factors for conversion during laparoscopic cholecystectomy - experiences from a general teaching hospital. Scand J Surg 100(3):169–173
Giger UF et al (2006) Risk factors for perioperative complications in patients undergoing laparoscopic cholecystectomy: analysis of 22,953 consecutive cases from the swiss association of laparoscopic and thoracoscopic surgery database. J Am Coll Surg 203(5):723–728
Wolf AS et al (2009) Surgical outcomes of open cholecystectomy in the laparoscopic era. Am J Surg 197(6):781–784
Zacks SL et al (2002) A population-based cohort study comparing laparoscopic cholecystectomy and open cholecystectomy. Am J Gastroenterol 97(2):334–340
Carbonell AM et al (2005) Do patient or hospital demographics predict cholecystectomy outcomes? A nationwide study of 93,578 patients. Surg Endosc 19(6):767–773
Alponat A et al (1997) Predictive factors for conversion of laparoscopic cholecystectomy. World J Surg 21(6):629–633
Visser BC, Parks RW, Garden OJ (2008) Open cholecystectomy in the laparoendoscopic era. Am J Surg 195(1):108–114
Peitzman AB, Watson GA, Marsh JW (2015) Acute cholecystitis: when to operate and how to do it safely. J Trauma Acute Care Surg 78(1):1–12
Licciardello A et al (2014) Preoperative risk factors for conversion from laparoscopic to open cholecystectomy. Eur Rev Med Pharmacol Sci 18(2 Suppl):60–68
Madan AK et al (2002) How early is early laparoscopic treatment of acute cholecystitis? Am J Surg 183(3):232–236
Lo CM et al (1997) Early decision for conversion of laparoscopic to open cholecystectomy for treatment of acute cholecystitis. Am J Surg 173(6):513–517
Goonawardena J, GunnarssonR, de Costa A Predicting conversion from laparoscopic to open cholecystectomy presented as a probability nomogram based on preoperative patient risk factors. Am J Surg
Gourgiotis S et al (2007) Laparoscopic cholecystectomy: a safe approach for management of acute cholecystitis. JSLS 11(2):219–224
Tang B, Cuschieri A (2006) Conversions during laparoscopic cholecystectomy: risk factors and effects on patient outcome. J Gastrointest Surg 10(7):1081–1091
Livingston EH, Rege RV (2004) A nationwide study of conversion from laparoscopic to open cholecystectomy. Am J Surg 188(3):205–211
Araujo-Teixeira JP et al (1999) Laparoscopy or laparotomy in acute cholecystitis (200 cases). Comparison of the results and factors predictive of conversion. Chirurgie 124(5):529–535
Wevers KP, van Westreenen HL, Patijn GA (2013) Laparoscopic cholecystectomy in acute cholecystitis: C-reactive protein level combined with age predicts conversion. Surg Laparosc Endosc Percutan Tech 23(2):163–166
Lengyel BI et al (2012) Laparoscopic cholecystectomy: what is the price of conversion? Surgery 152(2):173–178
Litynski GS (1998) Erich Muhe and the rejection of laparoscopic cholecystectomy (1985): a surgeon ahead of his time. JSLS 2(4):341–346
McMahon AJ et al (2000) Impact of laparoscopic cholecystectomy: a population-based study. Lancet 356(9242):1632–1637
Shamim M et al (2009) Reasons of conversion of laparoscopic to open cholecystectomy in a tertiary care institution. J Pak Med Assoc 59(7):456–460
Sain AH (1996) Laparoscopic cholecystectomy is the current “gold standard” for the treatment of gallstone disease. Ann Surg 224(5):689–690
Begos DG, Modlin IM (1994) Laparoscopic cholecystectomy: from gimmick to gold standard. J Clin Gastroenterol 19(4):325–330
Lengyel BI et al (2012) Laparoscopic cholecystectomy after a quarter century: why do we still convert? Surg Endosc 26(2):508–513
Chandio A et al (2009) Factors influencing the successful completion of laparoscopic cholecystectomy. JSLS 13(4):581–586
Shapiro AJ et al (1999) Predicting conversion of laparoscopic cholecystectomy for acute cholecystitis. JSLS 3(2):127–130
Kum CK et al (1996) Laparoscopic cholecystectomy for acute cholecystitis: is it really safe? World J Surg 20(1):43–48, discussion 48–9
Banz V et al (2011) Population-based analysis of 4113 patients with acute cholecystitis: defining the optimal time-point for laparoscopic cholecystectomy. Ann Surg 254(6):964–970
Acknowledgments
This study was presented at the annual meeting of the German Surgical Society in 2013 (130. Kongress der Deutschen Gesellschaft für Chirurgie, ID: 978).
Authors’ contributions
Study conception and design: Johannes Spohnholz, Ansgar Chromik, and Waldemar Uhl
Acquisition of data: Johannes Spohnholz (all data except histopathological findings) and Johanna Munding (histopathological findings)
Analysis and interpretation of data: Johannes Spohnholz and Ansgar Chromik
Drafting of manuscript: Johannes Spohnholz, Ansgar Chromik, and Torsten Herzog
Critical revision of manuscript: Johannes Spohnholz, Ansgar Chromik, Johanna Munding, Torsten Herzog, Chris Braumann, Orlin Belyaev, and Waldemar Uhl
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The protocol of this retrospective cohort study was approved by the ethics committee of the Ruhr-University Bochum, Germany (Permission no. 5059–14).
Because this was a retrospective analysis and the names of the patients were anonymized, informed consent from all individual participants was not needed.
Conflict of interest
All authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Spohnholz, J., Herzog, T., Munding, J. et al. Conversion cholecystectomy in patients with acute cholecystitis—it’s not as black as it’s painted!. Langenbecks Arch Surg 401, 479–488 (2016). https://doi.org/10.1007/s00423-016-1394-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-016-1394-3