Abstract
Purpose
Increased intraoperative parathyroid hormone excretion (“PTH spikes”) due to unintended manipulation of parathyroid adenoma can be observed frequently during surgery for primary hyperparathyroidism. This may lead to difficulties in interpreting intraoperative PTH curves. The aim of this study was to elucidate possible risk factors for PTH spikes and to evaluate the impact on different interpretation criteria of intraoperative PTH curves.
Methods
Eight hundred forty-seven patients with primary hyperparathyroidism were included. The probability of PTH spikes was analyzed regarding preoperative PTH- and creatinine levels, and size of adenoma and their impact on the Vienna, Miami, and Halle criteria was evaluated.
Results
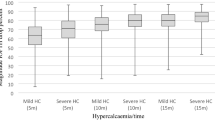
PTH spikes occurred in 102 patients (12 %) and revealed to be independent of PTH- and creatinine levels (p = 0.13) preoperatively. There was a significant negative correlation between “manipulation PTH” and “baseline PTH” values and the gland volume, respectively. Patients presenting with smaller adenomas and those with low-baseline PTH values show significantly higher manipulation values. No risk factor for manipulation was exposed and no significantly higher risk of misclassification as “false positive” in case of PTH spikes was detected for any interpretation criterion. For the “Vienna Criterion,” however, a significant increase in the risk of “false negative” misclassification was observed with increasing manipulation values.
Conclusions
In patients with PTH spikes, none of the analyzed criteria show a significant increase in missed adenomas. Nevertheless, the Vienna criterion shows a higher rate of potentially unnecessary explorations with increasing manipulation values. Thus, caution is warranted in detecting PTH spikes and in individual interpretations of specific PTH curves is recommended. The Miami criterion seems to be favorable in this group of patients.

Similar content being viewed by others
References
Jaskowiak NT, Sugg SL, Helke J, Koka MR, Kaplan EL (2002) Pitfalls of intraoperative quick parathyroid hormone monitoring and gamma probe localization in surgery for primary hyperparathyroidism. Arch Surg 137:659–668, discussion 668–9
Horanyi J, Duffek L, Szlavik R, Darvas K, Lakatos P, Toth M, Racz K (2003) Parathyroid surgical failures with misleading falls of intraoperative parathyroid hormone levels. J Endocrinol Investig 26:1095–1099
Phillips IJ, Kurzawinski TR, Honour JW (2005) Potential pitfalls in intraoperative parathyroid hormone measurements during parathyroid surgery. Ann Clin Biochem 42:453–458
Riss P, Kaczirek K, Bieglmayer C, Niederle B (2007) PTH spikes during parathyroid exploration—a possible pitfall during PTH monitoring? Langenbeck’s arch surg/Deutsche Gesellschaft für Chirurgie 392:427–430
Sidell D, Wang J, Sercarz J (2010) Spurious decline in intraoperative parathyroid hormone: false positives in parathyroid surgery. Am J Otolaryngol 31:479–481
Harrison BJ, Triponez F (2009) Intraoperative adjuncts in surgery for primary hyperparathyroidism. Langenbeck’s arch surg/Deutsche Gesellschaft für Chirurgie 394:799–809
Lepage R, Roy L, Brossard JH, Rousseau L, Dorais C, Lazure C, D’Amour P (1998) A non-(1–84) circulating parathyroid hormone (PTH) fragment interferes significantly with intact PTH commercial assay measurements in uremic samples. Clin Chem 44:805–809
Miller BS, England BG, Nehs M, Burney RE, Doherty GM, Gauger PG (2006) Interpretation of intraoperative parathyroid hormone monitoring in patients with baseline parathyroid hormone levels of <100 pg/mL. Surgery 140:883–889, discussion 889–90
Cook MR, Pitt SC, Schaefer S, Sippel R, Chen H (2010) A rising ioPTH level immediately after parathyroid resection: are additional hyperfunctioning glands always present? An application of the Wisconsin Criteria. Ann Surg 251:1127–1130
Yang GP, Levine S, Weigel RJ (2001) A spike in parathyroid hormone during neck exploration may cause a false-negative intraoperative assay result. Arch Surg 136:945–949, Chicago, Ill : 1960
Riss P, Asari R, Scheuba C, Bieglmayer C, Niederle B (2009) PTH secretion of “manipulated” parathyroid adenomas. Langenbeck’s arch surg/Deutsche Gesellschaft für Chirurgie 394:891–895
Prager G, Czerny C, Kurtaran A, Passler C, Scheuba C, Niederle B (1999) The value of preoperative localization studies in primary hyperparathyroidism. Der Chirurg; Zeitschrift für alle Gebiete der operativen Medizen 70:1082–1088
Prager G, Czerny C, Kurtaran A, Passler C, Scheuba C, Bieglmayer C, Niederle B (2001) Minimally invasive open parathyroidectomy in an endemic goiter area: a prospective study. Arch Surg 136:810–816, Chicago, Ill : 1960
Prager G, Czerny C, Ofluoglu S, Kurtaran A, Passler C, Kaczirek K, Scheuba C, Niederle B (2003) Impact of localization studies on feasibility of minimally invasive parathyroidectomy in an endemic goiter region. J Am Coll Surg 196:541–548
Riss P, Kaczirek K, Heinz G, Bieglmayer C, Niederle B (2007) A “defined baseline” in PTH monitoring increases surgical success in patients with multiple gland disease. Surgery 142:398–404
Bieglmayer C, Prager G, Niederle B (2002) Kinetic analyses of parathyroid hormone clearance as measured by three rapid immunoassays during parathyroidectomy. Clin Chem 48:1731–1738
Woodrum DT, Saunders BD, England BG, Burney RE, Doherty GM, Gauger PG (2004) The influence of sample site on intraoperative PTH monitoring during parathyroidectomy. Surgery 136:1169–1175
Irvin GL, Dembrow VD, Prudhomme DL (1991) Operative monitoring of parathyroid gland hyperfunction. Am J Surg 162:299–302
Lorenz K, Dralle H (2010) Intraoperative parathyroid hormone determination for primary hyperparathyroidism. Der Chirurg; Zeitschrift für alle Gebiete der operativen Medizen 81(636):638–642
Nussbaum SR, Thompson AR, Hutcheson KA, Gaz RD, Wang CA (1988) Intraoperative measurement of parathyroid hormone in the surgical management of hyperparathyroidism. Surgery 104:1121–1127
Riss P, Scheuba C, Asari R, Bieglmayer C, Niederle B (2009) Is minimally invasive parathyroidectomy without QPTH monitoring justified? Langenbeck’s arch surg/Deutsche Gesellschaft für Chirurgie 394:875–880
Hwang RS, Morris LF, Ro K, Park S, Ituarte PHG, Hong JC, Yeh MW (2010) A selective, Bayesian approach to intraoperative PTH monitoring. Ann Surg 251:1122–1126
Bachar G, Mizrachi A, Hadar T, Feinmesser R, Shpitzer T (2011) Role of parathyroid hormone monitoring during parathyroidectomy. Head & neck 33:1754–1757
Morris LF, Zanocco K, Ituarte PHG, Ro K, Duh Q-Y, Sturgeon C, Yeh MW (2010) The value of intraoperative parathyroid hormone monitoring in localized primary hyperparathyroidism: a cost analysis. Ann Surg Oncol 17:679–685
Hong JC, Morris LF, Park EJ, Ituarte PHG, Lee CH, Yeh MW (2011) Transient increases in intraoperative parathyroid levels related to anesthetic technique. Surgery 150:1069–1075
Cayo AK, Sippel RS, Schaefer S, Chen H (2009) Utility of intraoperative PTH for primary hyperparathyroidism due to multigland disease. Ann Surg Oncol 16:3450–3454
Riss P, Niederle B, Bieglmayer C (2011) A rising ioPTH level immediately after parathyroid resection: are additional hyperfunctioning glands always present? An application of the Wisconsin Criteria. Ann Surg 254:670–671
Barczynski M, Konturek A, Hubalewska-Dydejczyk A, Cichon S, Nowak W (2009) Evaluation of Halle, Miami, Rome, and Vienna intraoperative iPTH assay criteria in guiding minimally invasive parathyroidectomy. Langenbeck’s arch surg/Deutsche Gesellschaft fur Chirurgie 394:843–849
Reiher AE, Schaefer S, Chen H, Sippel RS (2012) Does the final intraoperative PTH level really have to fall into the normal range to signify cure? Ann Surg Oncol 19:1862–1867
Emmolo I, Corso HD, Borretta G, Visconti G, Piovesan A, Cesario F, Borghi F (2005) Unexpected results using rapid intraoperative parathyroid hormone monitoring during parathyroidectomy for primary hyperparathyroidism. World J surg 29:785–788
Richards ML, Thompson GB, Farley DR, Grant CS (2011) An optimal algorithm for intraoperative parathyroid hormone monitoring. Arch Surg 146:280–285, Chicago, Ill : 1960
Kandil E, Majid DS, Carson KA, Tufano RP (2012) A comparison of outcomes for younger and older adult patients undergoing surgery for primary hyperparathyroidism. Ann Surg Oncol 19:1897–1901
Adler JT, Sippel RS, Chen H (2010) 25-hydroxyvitamin D status does not affect intraoperative parathyroid hormone dynamics in patients with primary hyperparathyroidism. Ann Surg Oncol 17:2958–2962
Acknowledgments
The study was supported by the “Jubilaeumsfonds der Österreichischen Nationalbank” Grant 9307.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Riss, P., Krall, C., Scheuba, C. et al. Risk factors for “PTH spikes” during surgery for primary hyperparathyroidism. Langenbecks Arch Surg 398, 881–886 (2013). https://doi.org/10.1007/s00423-013-1097-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-013-1097-y