Abstract
Purpose
Visceral artery aneurysms (VAA) are rare forms of vascular pathology, with an incidence of 0.1% to 0.2% in routine autopsies [1–4]. They frequently present as a life-threatening, often fatal, emergency, if associated with rupture and intra- or retroperitoneal bleeding. The clinical symptoms, natural history, and mortality of VAAs vary depending on the vessels involved. The mortality rates range from 8.5% up to 25% and, in pregnant women, up to 75% [1, 4, 6, 7]. A retrospective analysis of all VAAs diagnosed at our institution from 1991 to 2006 was performed. The presentation, management, and outcome of therapy was evaluated for each patient.
Materials and methods
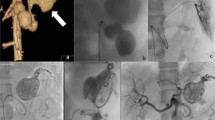
Twenty-three patients (12 men, 11 women, mean age 55.8 years) with 31 VAAs were identified. The anatomical involvement concerned seven regions: celiac (CT) nine, superior mesenteric (SMA) seven, splenic (SA) five, hepatic (HA) six, gastroduodenal (GDA) two, pancreatoduodenal (PDA) one, and one branch of the superior mesenteric artery. Fourteen patients presented symptoms attributable to their aneurysms, which included a total of four ruptures. Nine patients had no symptoms. The etiology of VAAs was atherosclerosis (67.8%), mycotic embolization (12.9%), trauma (9.7%), Marfan Syndrome (3.2%), Klippel–Trenaunay–Weber syndrome (3.2%), and giant cell arteritis (3.2%). Open surgery was performed for 29 aneurysm in 21 patients: partial resection and tailoring in 13 cases (41.9%), resection of the aneurysm with additional autologous vein graft interposition in nine cases and prosthetic graft interposition in 2 cases (35.5%), aneurysm exclusion by ligation in three cases (9.6%) and aneurysm ligation combined with additional autologous bypass procedure in two cases (6.5%). Two patients (6.5%) were treated interventionally with embolization, in one case each with a right hepatic artery aneurysm and in the other with splenic artery aneurysm.
Results
No deaths were observed. The morbidity rate associated with surgical treatment was low. After treatment, a total of 17 patients were followed up for a period ranging from 3 to 154 months (mean 54.6 months). Fifteen patients required no additional procedures. The patency rate of the reconstructed visceral arteries was 90.4%. Six patients were lost for follow-up.
Conclusions
Surgical and interventional therapy of VAAs can be life-saving treatments for the patient with a low periprocedural morbidity. The success rate, defined as the exclusion of VAA rupture and the absence of abdominal discomfort, in our material was 88.2% after a mean follow-up of 54.6 months.





Similar content being viewed by others
References
Lauschke H, Rudolph J, Textor J et al (2002) Das Visceralarterienaneurysma. Zentralbl Chir 127:538–542, doi:10.1055/s-2002-32624
Vollmar J (1996) Arterielle aneurysmata. In: Vollmar J (ed) Rekonstruktive Chirurgie der Arterien, 4th edn. Thieme Verlag, Stuttgart, pp 143–145
Ikeda O, Tamura Y, Nakasone Y et al (2008) Nonoperative management of unruptured visceral artery aneurysms: Treatment by transcatheter coil embolization. J Vasc Surg 47:1212–1219, doi:10.1016/j.jvs.2008.01.032
Carr SC, Mahvi DM, Hoch JR et al (2001) Visceral artery aneurysm rupture. J Vasc Surg 33:806–811, doi:10.1067/mva.2001.112320
Kalko Y, Ugurlucan M, Basaran M et al (2007) Visceral artery aneurysms. Heart Surg Forum 10:E24–E29, doi:10.1532/HSF98.20061130
Rossi M, Rebonato A, Greco L et al (2008) Endovascular exclusion of visceral artery aneurysms with stent-grafts: technique and long-term follow-up. Cardiovasc Intervent Radiol 31:36–42, doi:10.1007/s00270-007-9167-6
Chiesa R, Astore D, Guzzo G et al (2005) Visceral artery aneurysms. Ann Vasc Surg 19:42–48, doi:10.1007/s10016-004-0150-2
Stanley JC, Wakefield TW, Graham LM et al (1986) Clinical importance and management of splanchnic artery aneurysms. J Vasc Surg 3:836–840, doi:10.1067/mva.1986.avs0030836
Beaussier M (1770) Sur un aneurisme de l’artere splinque dont les parois se sont ossifiees. J Med Toulose 32:157
Quincke HI (1871) Ein Fall von Aneurysma der Leberarterie. Berliner klinische Wochenschrift 8:349–352
Kehr H (1903) Der erste Fall von erfolgreicher Unterbindung der A. hepatica propria wegen Aneurysma. Munch Med Wochenschr 50:1861–1867
Lindboe EF (1932) Aneurysm of splenic artery diagnosed by X-rays and operated upon with success. Acta Chir Scand 72:108–114
Tulsyan N, Kashyap VS, Greenberg RK et al (2007) The endovascular management of visceral artery aneurysms and pseudoaneurysms. J Vasc Surg 45:276–283, doi:10.1016/j.jvs.2006.10.049
Hossain A, Reis ED, Dave SP et al (2001) Visceral artery aneurysms: experience in a tertiary-care center. Am Surg 67:432–437
Saltzberg SS, Maldonado TS, Lamparello PJ et al (2005) Is endovascular therapy the preferred treatment of all visceral artery aneurysms? Ann Vasc Surg 19:507–515, doi:10.1007/s10016-005-4725-3
Carroccio A, Jacobs TS, Faries P et al (2007) Endovascular treatment of visceral artery aneurysms. Vasc Endovascular Surg 41:373–382, doi:10.1177/1538574407308552
Mcintyrie TP, Simone ST, Stahlfeld KR (2002) Intraoperative thrombin occlusion of a visceral artery aneurysm. J Vasc Surg 36:393–395, doi:10.1067/mva.2002.125014
Carmeci C, McClenathan J (2000) Visceral artery aneurysms as seen in a community hospital. Am J Surg 179:486–489, doi:10.1016/S0002-9610(00)00380-9
Sessa C, Tinelli G, Porcu P et al (2004) Treatment of visceral aneurysms: description of a retrospective series of 42 aneurysms in 34 patients. Ann Vasc Surg 18:695–703, doi:10.1007/s10016-004-0112-8
Carr SC, Pearce WH, Vogelzang RL et al (1996) Current management of visceral artery aneurysms. Surgery 120:627–634, doi:10.1016/S0039-6060(96)80009-2
Busuttil RW, Brin BJ (1980) The diagnosis and management of visceral artery aneurysms. Surgery 88:619–624
Graham JM, McCollum CH, DeBakey ME (1980) Aneurysms of the splanchnic arteries. Am J Surg 140:797–801, doi:10.1016/0002-9610(80)90120-8
Messina LM, Shanley CJ (1997) Visceral artery aneurysms. Surg Clin North Am 77:425–442, doi:10.1016/S0039-6109(05)70559-4
Tocchii M, Ogino H, Sasaki H et al (2005) Successful surgical treatment for aneurysm of splenic artery with anomalous origin. Ann Thorac Cardiovasc Surg 11:346–349
Ohta M, Hashizume M, Tanoue K et al (1992) Splenic hyperkinetic state and splenic artery aneurysm in portal hypertension. Hepatogastroenterology 39:529–532
Kasirajan K, Greenberg RK, Clair D, Ouriel K (2001) Endovascular management of visceral artery aneurysm. J Endovasc Ther 8:150–155, doi:10.1583/1545-1550(2001)008<0150:EMOVAA>2.0.CO;2
Muscari F, Barret A, Chaufour X et al (2002) Management of visceral artery aneurysms. Retrospective study of 23 cases. Ann Chir 127:281–288, doi:10.1016/S0003-3944(02)00746-0
Rokke O, Sondenaa K, Amundsen SR et al (1997) Successful management of eleven splanchnic artery aneurysms. Eur J Surg 163:411–417
Stone WM, Abbas M, Cherry KJ et al (2002) Superior mesenteric artery aneurysms: Is presence an indication for intervention? J Vasc Surg 36:234–237, doi:10.1067/mva.2002.125027
Neschis DG, Safford SD, Golden MA (1998) Management of pancreaticoduodenal artery aneurysms presenting as catastrophic intraabdominal bleeding. Surgery 123:8–12
Pourhassan S, Grotemeyer D, Klar V, Sandmann W (2007) Das Klippel-Trenaunay Syndrom bei gleichzeitigem Vorliegen von Viszeralarterienaneurysmen. Vasa 36:124–129, doi:10.1024/0301-1526.36.2.124
Grotemeyer D, Pourhassan S, Voshege M, Sandmann W (2008) Proteus’syndrome as a differential diagnosis of vascular malformations. Vasa 37:2, doi:10.1024/0301-1526.37.2.187
Grotemeyer D, Grabitz K, Balzer K et al (2004) Das mykotische Viszeralarterienaneurysma. Klinik, Diagnostik und Differentialtherapie mit Darstellung der Literatur. Chirurg 75:533–540, doi:10.1007/s00104-004-0828-6
Jimenez JC, Lawrence PF, Reil TD (2008) Endovascular exclusion of superior mesenteric artery pseudoaneurysms: an alternative to open laparotomy in high-risk patients. Vasc Endovascular Surg 42:184–186, doi:10.1177/1538574407308367
Gabelmann A, Gorich J, Merkle EM (2002) Endovascular treatment of visceral artery aneurysms. J Endovasc Ther 9:38–47, doi:10.1583/1545-1550(2002)009<0038:ETOVAA>2.0.CO;2
Harvey J, Daedik H, Impeduglia T, Woo D, DeBernardis F (2006) Endovascular management of hepatic artery pseudoaneurysms hemorrhage complicating pancreaticoduodenectomy. J Vasc Surg 43:613–617, doi:10.1016/j.jvs.2005.11.031
Larson RA, Solomon J, Carpenter JP (2002) Stent graft repair of visceral artery aneurysms. J Vasc Surg 36:1260–1263, doi:10.1067/mva.2002.129645
Salam TA, Lumsden AB, Martin LG, Smith RB 3rd (1992) Nonoperative management of visceral aneurysms and pseudoaneurysms. Am J Surg 164:215–219, doi:10.1016/S0002-9610(05)81073-6
Bratby MJ, Lehmann ED, Bottomley J et al (2006) Endovascular embolization of visceral artery aneurysma with ethylene-vinyl alcohol onyx: a case series. Cardiovasc Intervent Radiol 29:1125–1128, doi:10.1007/s00270-005-0148-3
Atkins BZ, Ryan JM, Gray JL (2003) Treatment of a celiac artery aneurysm with endovascular stent grafting. Vasc Endovascular Surg 37:367–373, doi:10.1177/153857440303700510
Sandford RM, Lloyd DM, Ross Naylor A (2006) Laparoscopic ligation of splenic artery aneurysm. Surg Laparosc Endosc Percutan Tech 16:102–103, doi:10.1097/00129689-200604000-00010
Kokkalera U, Bhende S, Ghellai A (2006) Laparoscopic management of splenic artery aneurysms. J Laparoendosc Adv Surg Tech A 16:604–608, doi:10.1089/lap.2006.16.604
Reardon PR, Otah E, Craig ES, Matthews BD, Reardon MJ (2005) Laparoscopic resection of splenic artery aneurysms. Surg Endosc 19:488–493, doi:10.1007/s00464-004-8916-8
Parts of this study have been presented as a poster titled “Langzeitergebnisse nach operativer und interventioneller Therapie von Visceralarterienaneurysmen,” Duran M, Grotemeyer D, Park EJ, Hoffmann N, and Sandmann W on the 24th annual meeting of the Deutsche Gesellschaft für Gefäßchirurgie in Dresden, Germany in September 10 to 13, 2008.
Author information
Authors and Affiliations
Corresponding author
Additional information
Both authors Dirk Grotemeyer and Mansur Duran contributed equally to this manuscript.
Rights and permissions
About this article
Cite this article
Grotemeyer, D., Duran, M., Park, EJ. et al. Visceral artery aneurysms—follow-up of 23 patients with 31 aneurysms after surgical or interventional therapy. Langenbecks Arch Surg 394, 1093–1100 (2009). https://doi.org/10.1007/s00423-009-0482-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-009-0482-z