Abstract
Objective
In a difficult and demanding environment such as the operating room, the individual workload response of physicians is of particular importance. The aim of this study was to examine the specific effects of intraoperative stress on the cardiovascular system by measuring heart rate (HR) and heart rate variability (HRV).
Methods
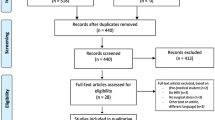
In a cross-sectional study, the effect of intraoperative stress on autonomic balance, measured by HRV, among surgeons differing with respect to their intraoperative stress levels was studied. Based on their perceived stress (State Trait Anxiety Inventory), surgeons were classified into a stressed and a non-stressed sample. Data on HR and HRV were collected by means of ambulatory ECG-recordings. Changes in autonomic nervous system activity were quantified by frequency and time domain analysis of R–R interval variability. Demographic, anthropometric, and surgery-related group differences were assessed by non-parametric Mann–Whitney U test, differences between relative changes of HR and HRV by Wilcoxon signed-ranks test. In multivariate linear analysis of covariance, group differences were adjusted for possible confounding factors.
Results
There was a significant difference in intraoperative HR for stressed and non-stressed surgeons (median: 99.3 vs. 63.7; P < 0.05). During sleep, HRV indices indicated a reduced autonomic recovery in stressed participants.
Conclusions
Our results reveal that higher perceived stress in the operating room is associated with increased intraoperative HR and decreased HRV at night. Non-stressed surgeons show greater relaxation during sleep compared to their stressed colleagues.

Similar content being viewed by others
References
Acharya UR, Kannathal N, Sing OW, Ping LY, Chua T (2004) Heart rate analysis in normal subjects of various age groups. Biomed Eng Online 3:8
Agelink MW, Malessa R, Baumann B, Majewski T, Akila F, Zeit T, Ziegler D (2001) Standardized tests of heart rate variability: normal ranges obtained from 309 healthy humans, and effects of age, gender, and heart rate. Clin Auton Res 11:99–108
Araujo F, Antelmi I, Pereira AC, Latorre MR, Grupi CJ, Krieger JE, Mansur AJ (2006) Lower heart rate variability is associated with higher serum high-sensitivity C-reactive protein concentration in healthy individuals aged 46 years or more. Int J Cardiol 107:333–337
Arora S, Sevdalis N, Nestel D, Woloshynowych M, Darzi A, Kneebone R (2010a) The impact of stress on surgical performance: a systematic review of the literature. Surgery 147:318–330
Arora S, Tierney T, Sevdalis N, Aggarwal R, Nestel D, Woloshynowych M, Darzi A, Kneebone R (2010b) The imperial stress assessment tool (ISAT): a feasible, reliable and valid approach to measuring stress in the operating room. World J Surg 34:1756–1763
Balanos GM, Phillips AC, Frenneaux MP, McIntyre D, Lykidis C, Griffin HS, Carroll D (2010) Metabolically exaggerated cardiac reactions to acute psychological stress: the effects of resting blood pressure status and possible underlying mechanisms. Biol Psychol 85:104–111
Balch CM, Shanafelt TD, Dyrbye L, Sloan JA, Russell TR, Bechamps GJ, Freischlag JA (2010) Surgeon distress as calibrated by hours worked and nights on call. J Am Coll Surgeons 211:609–619
Belkic KL, Landsbergis PA, Schnall PL, Baker D (2004) Is job strain a major source of cardiovascular disease risk? Scand J Work Environ Health 30:85–128
Bernardi L, Passino C, Spadacini G, Valle F, Leuzzi S, Piepoli M, Leight P (1997) Arterial Baroreceptors as determinants of 0.1 Hz and respiration-related changes in blood pressure and heart rate spectra. In: Mancia GPGZA (ed) Frontiers of blood pressure and heart rate analysis. IOC Press, Netherlands, pp 241–252
Bigger JT Jr, Fleiss JL, Steinman RC, Rolnitzky LM, Kleiger RE, Rottman JN (1992) Frequency domain measures of heart period variability and mortality after myocardial infarction. Circulation 85:164–171
Binici Z, Mouridsen MR, Køber L, Sajadieh A (2011) Decreased nighttime heart rate variability is associated with increased stroke risk. Stroke 42:3196–3201
Böckelmann I (2012) Analysis of heart rate variability—relevance for practice. Analyse der Herzfrequenzvariabilität (HRV)—praktische Relevanz. Zlb Arbeitsmed 62:275–279
Böhm B, Rotting N, Schwenk W, Grebe S, Mansmann U (2001) A prospective randomized trial on heart rate variability of the surgical team during laparoscopic and conventional sigmoid resection. Arch Surg 136:305–310
Borchini R, Ferrario MM (2012) Job strain and heart rate variability. New evidence and new perspectives. Job strain e heart rate variability. Nuove evidenze e nuove prospettive. G Ital Med Lav Ergon 34:174–176
Boutcher SH, Nugent FW, McLaren PF, Weltman AL (1998) Heart period variability of trained and untrained men at rest and during mental challenge. Psychophysiol 35:16–22
Brosschot JF, Van Dijk E, Thayer JF (2007) Daily worry is related to low heart rate variability during waking and the subsequent nocturnal sleep period. Int J Psychophysiol 63:39–47
Brotman DJ, Golden SH, Wittstein IS (2007) The cardiovascular toll of stress. Lancet 370:1089–1100
Brunner EJ, Hemingway H, Walker BR, Page M, Clarke P, Juneja M, Shipley MJ, Kumari M, Andrew R, Seckl JR, Papadopoulos A, Checkley S, Rumley A, Lowe GDO, Stansfeld SA, Marmot MG (2002) Adrenocortical, autonomic, and inflammatory causes of the metabolic syndrome: nested case-control study. Circulation 106:2659–2665
Buddeberg-Fischer B, Klaghofer R, Stamm M, Siegrist J, Buddeberg C (2008) Work stress and reduced health in young physicians: prospective evidence from Swiss residents. Int Arch Occup Environ Health 82:31–38
Cacioppo JT, Malarkey WB, Kiecoltglaser JK, Uchino BN, Sgoutasemch SA, Sheridan JF, Berntson GG, Glaser R (1995) Heterogeneity in neuroendocrine and immune-responses to brief psychological stressors as a function of autonomic cardiac activation. Psychosom Med 57:154–164
Camm AJ, Fei L (1995) Risk stratification following myocardial infarction: heart rate variability and other risk factors. In: Malik M, Camm AJ (eds) Heart rate variability. Futura, Armonk, pp 369–393
Chandola T, Britton A, Brunner E, Hemingway H, Malik M, Kumari M, Badrick E, Kivimaki M, Marmot M (2008) Work stress and coronary heart disease: what are the mechanisms? Eur Heart J 29:640–648
Clays E, De Bacquer D, Crasset V, Kittel F, De Smet P, Kornitzer M, Karasek R, De Backer G (2011) The perception of work stressors is related to reduced parasympathetic activity. Int Arch Occ Environ Health 84:185–191
Cook S, Togni M, Schaub MC, Wenaweser P, Hess OM (2006) High heart rate: a cardiovascular risk factor? Eur Heart J 27:2387–2393
Cooney MT, Vartiainen E, Laakitainen T, Juolevi A, Dudina A, Graham IM (2010) Elevated resting heart rate is an independent risk factor for cardiovascular disease in healthy men and women. Am Heart J 159:612–619
Czyzewska E, Kiczka K, Czarnecki A, Pokinko P (1983) The surgeon’s mental load during decision making at various stages of operations. Eur J Appl Physiol Occup Physiol 51:441–446
Diène E, Fouquet A, Esquirol Y (2012) Cardiovascular diseases and psychosocial factors at work. Arch Cardiovasc Dis 105:33–39
Dietrich DF, Schindler C, Schwartz J, Barthelemy JC, Tschopp JM, Roche F, von Eckardstein A, Brändli O, Leuenberger P, Gold DR, Gaspoz JM, Ackermann-Liebrich U (2006) Heart rate variability in an ageing population and its association with lifestyle and cardiovascular risk factors: results of the SAPALDIA study. Europace 8:521–529
Fontana GA, Pantaleo T, Bongianni F, Cresci F, Manconi R, Panuccio P (1993) Respiratory and cardiovascular responses to static handgrip exercise in humans. J Appl Physiol 75:2789–2796
Gianaros PJ, Salomon K, Zhou F, Owens JF, Edmundowicz D, Kuller LH, Matthews KA (2005) A greater reduction in high-frequency heart rate variability to a psychological stressor is associated with subclinical coronary and aortic calcification in postmenopausal women. Psychosom Med 67:553–560
Gillman MW, Kannel WB, Belanger A, D’Agostino RB (1993) Influence of heart rate on mortality among persons with hypertension: the Framingham study. Am Heart J 125:1148–1154
Grandjean E (1991) Physiologische Arbeitsgestaltung. Ecomed, Landsberg
Grasso R, Schena F, Gulli G, Cevese A (1997) Does low-frequency variability of heart period reflect a specific parasympathetic mechanism? J Auton Nerv Syst 63:30–38
Hansen TW, Thijs L, Boggia J, Li Y, Kikuya M, Bjorklund-Bodegard K, Richart T, Ohkubo T, Jeppesen J, Torp-Pedersen C, Lind L, Sandoya E, Imai Y, Wang J, Ibsen H, O’Brien E, Staessen JA (2008) Prognostic value of ambulatory heart rate revisited in 6928 subjects from 6 populations. Hypertension 52:229–235
Hayano J, Sakakibara Y, Yamada M, Ohte N, Fujinami T, Yokoyama K, Watanabe Y, Takata K (1990) Decreased magnitude of heart rate spectral components in coronary artery disease: its relation to angiographic severity. Circulation 81:1217–1224
Hiemisch A, Kiess W, Brähler E (2011) Mental job strain in a university children’s hospital a study on stress experience and the resulting employee health. Psychische Arbeitsbelastung an einer Universitätskinderklinik—Ergebnisse einer Umfrage zum Belastungserleben und der resultierenden Mitarbeitergesundheit. Klin Padiatr 223:236–241
Hintsanen M, Elovainio M, Puttonen S, Kivimaki M, Koskinen T, Raitakari OT, Keltikangas-Jarvinen L (2007) Effort-reward imbalance, heart rate, and heart rate variability: the cardiovascular risk in young Finns study. Int J Behav Med 14:202–212
Horner RD, Matthews G, Yi MS (2012) A conceptual model of physician work intensity: guidance for evaluating policies and practices to improve health care delivery. Med Care 50:654–661
Iellamo F, Legramante JM, Raimondi G, Castrucci F, Damiani C, Foti C, Peruzzi G, Caruso I (1997) Effects of isokinetic, isotonic and isometric submaximal exercise on heart rate and blood pressure. Eur J Appl Physiol Occup Physiol 75:89–96
Jose AD, Collins D (1970) The normal range and determinants of intrinsic heart rate in man. Cardiovasc Res 4:160–167
Kannel WB, Wilson P, Blair SN (1985) Epidemiological assessment of the role of physical activity and fitness in development of cardiovascular disease. Am Heart J 109:876–885
Kivimaki M, Leino-Arjas P, Luukkonen R, Riihimaki H, Vahtera J, Kirjonen J (2002) Work stress and risk of cardiovascular mortality: prospective cohort study of industrial employees. BMJ 325:857
Klein J, Frie KG, Blum K, Von Dem Knesebeck O (2011) Psychosocial stress at work and perceived quality of care among clinicians in surgery. Health Serv Res 11:109
Kuo TBJ, Lin T, Yang CCH, Li CL, Chen CF, Chou P (1999) Effect of aging on gender differences in neural control of heart rate. Am J Physiol-Heart C 277:H2233–H2239
Lind AR (1970) Cardiovascular responses to static exercise (Isometrics, anyone?). Circulation 41:173–176
Malmberg B, Persson R, Flisberg P, Orbaek P (2011) Heart rate variability changes in physicians working on night call. Int Arch Occup Environ Health 84:293–301
Marteau TM, Bekker H (1992) The development of a six-item short-form of the state scale of the Spielberger state-trait anxiety inventory (STAI). Brit J Clin Psychol 31:301–306
Mathiassen SE (1993) The influence of exercise/rest schedule on the physiological and psychophysical response to isometric shoulder-neck exercise. Eur J Appl Physiol 67:528–539
Neubert S, Arndt D, Thurow K, Stoll R (2010) Mobile real-time data acquisition system for application in preventive medicine. Telemed eHealth 16:504–509
Pieper S, Brosschot JF, van der Leeden R, Thayer JF (2007) Cardiac effects of momentary assessed worry episodes and stressful events. Psychosom Med 69:901–909
Rieger A, Neubert S, Behrendt S, Weippert M, Kreuzfeld S, Stoll R (2012) 24-hour ambulatory monitoring of complex physiological parameters with a wireless health system. In: Proceedings of the 9th IEEE international multiconference on systems, signals and devices (SSD), Chemnitz, Germany, 2012. Published online. doi:10.1109/SSD.2012.6198016
Schuld J, Bobkowski M, Shayesteh-Kheslat R, Kollmar O, Richter S, Schilling MK (in press) Benchmarking surgical resources—a work sampling analysis at a german university hospital. Ärztliche Ressourcennutzung in der Chirurgie auf dem Prüfstand—eine Worksampling-Analyse an einer deutschen Universitätsklinik. Zbl Chirurgie
Smolander J, Aminoff T, Korhonen I, Tervo M, Shen N, Korhonen O, Louhevaara V (1998) Heart rate and blood pressure responses to isometric exercise in young and older men. Eur J Appl Physiol Occup Physiol 77:439–444
Snyder F, Hobson JA, Morrison DF, Goldfrank F (1964) Changes in respiration, heart rate, and systolic blood pressure in human sleep. J Appl Physiol 19:417–422
Song MH, Tokuda Y, Nakayama T, Sato M, Hattori K (2009) Intraoperative heart rate variability of a cardiac surgeon himself in coronary artery bypass grafting surgery. Interact Cardiovasc Thorac Surg 8:639–641
Spalding TW, Jeffers LS, Porges SW, Hatfield BD (2000) Vagal and cardiac reactivity to psychological stressors in trained and untrained men. Med Sci Sports Exerc 32:581–591
Stein PK, Barzilay JI, Chaves PHM, Domitrovich PP, Gottdiener JS (2009) Heart rate variability and its changes over 5 years in older adults. Age Ageing 38:212–218
Steptoe A, Kivimäki M (2012) Stress and cardiovascular disease. Nat Rev Cardiol 9:360–370
Task Force of the European Society of Cardiology, North American Society of Pacing and Electrophysiology (1996) Heart rate variability: standards of measurement, physiological interpretation and clinical use. Circulation 93:1043–1065
Thayer JF (2005) Neurovisceral integration, emotions, and health. J Psychosom Res 58:S9
Thayer JF, Yamamoto SS, Brosschot JF (2010) The relationship of autonomic imbalance, heart rate variability and cardiovascular disease risk factors. Int J Cardiol 141:122–131
Togo F, Takahashi M (2009) Heart rate variability in occupational health—a systematic review. Ind Health 47:589–602
Tsuji H, Larson MG, Venditti FJ Jr, Manders ES, Evans JC, Feldman CL, Levy D (1996) Impact of reduced heart rate variability on risk for cardiac events: the Framingham heart study. Circulation 94:2850–2855
Umetani K, Singer DH, McCraty R, Atkinson M (1998) Twenty-four hour time domain heart rate variability and heart rate: relations to age and gender over nine decades. J Am Coll Cardiol 31:593–601
Vanoli E, Adamson PB, Ba L, Pinna GD, Lazzara R, Orr WC (1995) Heart rate variability during specific sleep stages: a comparison of healthy subjects with patients after myocardial infarction. Circulation 91:1918–1922
Virtanen R, Jula A, Kuusela T, Helenius H, Voipio-Pulkki LM (2003) Reduced heart rate variability in hypertension: associations with lifestyle factors and plasma renin activity. J Hum Hypertens 17:171–179
Weber CS, Thayer JF, Rudat M, Wirtz PH, Zimmermann-Viehoff F, Thomas A, Perschel FH, Arck PC, Deter HC (2010) Low vagal tone is associated with impaired post stress recovery of cardiovascular, endocrine, and immune markers. Eur J Appl Physiol 109:201–211
Wennerblom B, Lurje L, Karlsson T, Tygesen H, Vahisalo R, Hjalmarson A (2001) Circadian variation of heart rate variability and the rate of autonomic change in the morning hours in healthy subjects and angina patients. Int J Cardiol 79:61–69
Wetzel CM, George A, Hanna GB, Athanasiou T, Black SA, Kneebone RL, Nestel D, Woloshynowych M (2011) Stress management training for surgeons-a randomized, controlled, intervention study. Ann Surg 253:488–494
Wong GWSJ (2008) Doctors and stress. Hongkong Medical Diary 13:4–7
Conflict of interest
The authors declare that there is no conflict of interest in the present study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rieger, A., Stoll, R., Kreuzfeld, S. et al. Heart rate and heart rate variability as indirect markers of surgeons’ intraoperative stress. Int Arch Occup Environ Health 87, 165–174 (2014). https://doi.org/10.1007/s00420-013-0847-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-013-0847-z