Abstract
Purpose
To compare myopia progression in children randomized to MiSight contact lenses (CLs) versus children corrected with single-vision spectacles (SV) over a 2-year period.
Methods
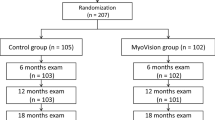
Subjects aged 8 to 12 with myopia (−0.75 to −4.00 D sphere) and astigmatism (< −1.00 D cylinder) were assigned to the lens study group (MiSight) or the control group (single vision). Measurements of visual acuity and subjective refraction were taken at 6-month intervals, and axial length, anterior chamber, corneal power, and cycloplegic autorefraction were measured at the baseline, 12-month, and 24-month visits.
Results
Eighty-nine subjects were recruited. Forty-fix children were assigned to the MiSight group, and 33 to the single-vision spectacle group. In total, 74 children completed the clinical trial, with the following parameters at the beginning of the study: n = 41 in the MiSight group (age: 11.01 ± 1.23 years, spherical equivalent: −2.16 ± 0.94 D, gender: male: 21, female: 20) and n = 33 in the single-vision group (age: 10.12 ± 1.38 years, spherical equivalent: −1.75 ± 0.94 D, gender: male: 12, female: 21). After 2 years of follow-up, myopia progressed slowly in the MiSight group compared to the control group (0.45 D vs 0.74 D, p < 0.001) and there was less axial elongation in the MiSight group compared to the single-vision group (0.28 mm vs 0.44 mm, p < 0.001). Therefore, use of MiSight CLs produced lower myopia progression (39.32%) and lower axial growth of the eye (36.04%) at 2 years compared to spectacle use.
Conclusions
MiSight contact lens wear reduces axial elongation and myopia progression in comparison to distance single-vision spectacles in children.
ClinicalTrials.gov Identifier: NCT01917110.



Similar content being viewed by others
References
Gifford P, Gifford KL (2016) The future of myopia control contact lenses. Optom Vis Sci 93:336–343. https://doi.org/10.1097/OPX.0000000000000762
Pan C, Ramamurthy D, Saw S (2012) Worldwide prevalence and risk factors for myopia. Ophthalmic Physiol Opt 32:3–16. https://doi.org/10.1111/j.1475-1313.2011.00884.x
Pan C, Dirani M, Cheng C, Wong T, Saw S (2015) The age-specific prevalence of myopia in Asia: a meta-analysis. Optom Vis Sci 92:258–266. https://doi.org/10.1097/OPX.0000000000000516
Foster PJ, Jiang Y (2014) Epidemiology of myopia. Eye (Lond) 28:202–208. https://doi.org/10.1038/eye.2013.280
Saw S, Gazzard G, Shih-Yen E, Chua W (2005) Myopia and associated pathological complications. Ophthalmic Physiol Opt 25:381–391
Leung CK, Mohamed S, Leung KS et al (2006) Retinal nerve fiber layer measurements in myopia: an optical coherence tomography study. Invest Ophthalmol Vis Sci 47:5171–5176
McBrien NA, Gentle A (2003) Role of the sclera in the development and pathological complications of myopia. Prog Retin Eye Res 22:307–338
Lim R, Mitchell P, Cumming RG (1999) Refractive associations with cataract: the Blue Mountains eye study. Invest Ophthalmol Vis Sci 40:3021–3026
Younan C, Mitchell P, Cumming RG, Rochtchina E, Wang JJ (2002) Myopia and incident cataract and cataract surgery: the Blue Mountains Eye Study. Invest Ophthalmol Vis Sci 43:3625–3632
Miller DG, Singerman LJ (2001) Natural history of choroidal neovascularization in high myopia. Curr Opin Ophthalmol 12:222–224
Chen S, Lu P, Zhang W, Lu J (2012) High myopia as a risk factor in primary open angle glaucoma. Int J Ophthalmol 5:750–753. https://doi.org/10.3980/j.issn.2222-3959.2012.06.18
Perera SA, Wong TY, Tay W, Foster PJ, Saw S, Aung T (2010) Refractive error, axial dimensions, and primary open-angle glaucoma: the Singapore Malay Eye Study. Arch Ophthalmol 128:900–905. https://doi.org/10.1001/archophthalmol.2010.125
Logan NS, Gilmartin B, Marr JE, Stevenson MR, Ainsworth JR (2004) Community-based study of the association of high myopia in children with ocular and systemic disease. Optom Vis Sci 81:11–13
Cheng SC, Lam CS, Yap MK (2013) Prevalence of myopia-related retinal changes among 12–18-year-old Hong Kong Chinese high myopes. Ophthalmic Physiol Opt 33:652–360
Huang J, Wen D, Wang Q et al (2016) Efficacy comparison of 16 interventions for myopia control in children: a network meta-analysis. Ophthalmology 123:697–708. https://doi.org/10.1016/j.ophtha.2015.11.010
Walline J, Lindsley K, Vedula S, Cotter SA, Mutti DO, Twelker JD (2011) Interventions to slow progression of myopia in children. Cochrane Database Syst Rev CD004916. doi:https://doi.org/10.1002/14651858.CD004916.pub3
Chia A, Chua W, Cheung Y et al (2012) Atropine for the treatment of childhood myopia: safety and efficacy of 0.5%, 0.1%, and 0.01% doses (atropine for the treatment of myopia 2). Ophthalmology 119:347–354. https://doi.org/10.1016/j.ophtha.2011.07.031
Fang P, Chung M, Yu H, Wu P (2010) Prevention of myopia onset with 0.025% atropine in premyopic children. J Ocul Pharmacol Ther 26:341–245
Siatkowski RM, Cotter S, Miller JM, Scher CA, Crockett RS, Novack GD (2004) Safety and efficacy of 2% pirenzepine ophthalmic gel in children with myopia: a 1-year, multicenter, double-masked, placebo-controlled parallel study. Arch Ophthalmol 122:1667–1674
Siatkowski RM, Cotter SA, Crockett RS, Miller JM, Novack GD, Zadnik K (2008) Two-year multicenter, randomized, double-masked, placebo-controlled, parallel safety and efficacy study of 2% pirenzepine ophthalmic gel in children with myopia. J AAPOS 12:332–339
Del Tacca M, Danesi R, Blandizzi C, Bernardini MC (1989) A selective antimuscarinic agent: pirenzepine. Review of its pharmacologic and clinical properties. Minerva Dietol Gastroenterol 35:175–189
Wen D, Huang J, Chen H et al (2015) Efficacy and acceptability of orthokeratology for slowing myopic progression in children: systematic review and meta-analysis. J Ophthalmol 2015:360806. https://doi.org/10.1155/2015/360806
Si J, Tang K, Bi H, Guo D, Guo J, Wang X (2005) Orthokeratology for myopia control: a meta-analysis. Optom Vis Sci 92:252–257. https://doi.org/10.1097/OPX.0000000000000505
Sun Y, Xu F, Zhang T et al (2015). Orthokeratology to control myopia progression: a meta-analysis. PLoS ONE 10(4): e0124535. doi:https://doi.org/10.1371/journal.pone.0124535
Li S, Kang M, Wu S et al (2015) Efficacy, safety and acceptability of orthokeratology on slowing axial elongation in myopic children by meta-analysis. Curr Eye Res 41(5):600–608. https://doi.org/10.3109/02713683.2015.1050743
Aller TA, Liu M, Wildsoet CF (2016) Myopia control with bifocal contact lenses: a randomized clinical trial. Optom Vis Sci 93:344–352. https://doi.org/10.1097/OPX.0000000000000808
Anstice NS, Phillips JR (2011) Effect of dual-focus soft contact lens wear on axial myopia progression in children. Ophthalmology 118:1152–1161. https://doi.org/10.1016/j.ophtha.2010.10.035
Lam CSY, Tang WC, Tse DY, Tang YY, TO CH (2014) Defocus incorporated soft contact (DISC) lens slows myopia progression in Hong Kong Chinese schoolchildren: a 2-year randomized clinical trial. Br J Ophthalmol 98:40–45. https://doi.org/10.1136/bjophthalmol-2013-303914
Chamberlain P, Back A, Lazon P, et al (2017) 3-year effectiveness of a dual-focus 1 day soft contact lens for myopia control. Paper presented at British Contact Lens Association 40th Clinical Conference. Liverpool, UK. June 10, 2017
Walline JJ, Greiner KL, McVey ME, Jones-Jordan LA (2013) Multifocal contact lens myopia control. Optom Vis Sci 90:1207–1214. https://doi.org/10.1097/OPX.0000000000000036
Sankaridurg P, Holden B, Smith E et al (2011) Decrease in rate of myopia progression with a contact lens designed to reduce relative peripheral hyperopia: one-year results. Invest Ophthalmol Vis Sci 52:9362–9367. https://doi.org/10.1167/iovs.11-7260
Fujikado T, Ninomiya S, Kobayashi T, Suzaki A, Nakada M, Nishida K (2014) Effect of low-addition soft contact lenses with decentered optical design on myopia progression in children: a pilot study. Clin Ophthalmol 8:1947–1956. https://doi.org/10.2147/OPTH.S66884
Pauné J, Morales H, Armengol J, Quevedo L, Faria-Ribeiro M, González-Méijome JM (2015) Myopia control with a novel peripheral gradient soft lens and orthokeratology: a 2-year clinical trial. Biomed Res Int 2015:507572. doi:https://doi.org/10.1155/2015/507572
Santodomingo-Rubido J, Villa-Collar C (2016) Optical treatments to reduce the progression of myopia. In: González-Méijome JM, Villa-Collar C (eds) Eye surface and contact lenses. 1st ed. Foundation for Visual Health, Optometry Development, and Audiology Development, Madrid, pp 542–567
Kollbaum PS, Jansen ME, Tan J, Meyer DM, Rickert ME (2013) Vision performance with a contact lens designed to slow myopia progression. Optom Vis Sci 90:205–214. https://doi.org/10.1097/OPX.0b013e3182812205
Norton T, Siegwart J, Amedo A (2006) Effectiveness of hyperopic defocus, minimal defocus, or myopic defocus in competition with a myopiagenic stimulus in tree shrew eyes. Invest Ophthalmol Vis Sci 47:4687–4699
Schaeffel F, Howland HC (1991) Properties of the feedback loops controlling eye growth and refractive state in the chicken. Vis Res 31:717–734
Smith EL 3rd, Hung LF, Huang J (2009) Relative peripheral hyperopic defocus alters central refractive development in infant monkeys. Vis Res 49:2386–2392. https://doi.org/10.1016/j.visres.2009.07.011
Smith EL 3rd, Kee CS, Ramamirtham R, Hung L (2005) Peripheral vision can influence eye growth and refractive development in infant monkeys. Invest Ophthalmol Vis Sci 46:3965–3972
Smith EL 3rd, Ramamirtham R, Qiao-Grider Y et al (2007) Effects of foveal ablation on emmetropization and form-deprivation myopia. Invest Ophthalmol Vis Sci 48:3914–3922
Linke S, Baviera J, Munzer G, Steinberg J, Richard G, Katz T (2011) Association between ocular dominance and spherical/astigmatic anisometropia, age, and sex: analysis of 10,264 myopic individuals. Invest Ophthalmol Vis Sci 52:9166–9173. https://doi.org/10.1167/iovs.11-8131
Thibos LN, Wheeler W, Horner D (1997) Power vectors: an application of Fourier analysis to the description and statistical analysis of refractive error. Optom Vis Sci 74:367–375
Walline JJ, Jones LA, Sinnott LT (2009) Corneal reshaping and myopia progression. Br J Ophthalmol 93:1181–1185. https://doi.org/10.1136/bjo.2008.151365
Cho P, Cheung SW, Edwards M (2005) The longitudinal orthokeratology research in children (LORIC) in Hong Kong: a pilot study on refractive changes and myopic control. Curr Eye Res 30:71–80
Edwards MH, Li RW, Lam CS, Lew JK, Yu BS (2002) The Hong Kong progressive lens myopia control study: study design and main findings. Invest Ophthalmol Vis Sci 43:2852–2858
Ip JM, Huynh SC, Robaei D et al (2008) Ethnic differences in refraction and ocular biometry in a population-based sample of 11–15-year-old Australian children. Eye (Lond) 22:649–656
Saw SM, Nieto FJ, Katz J, Schein OD, Levy B, Chew SJ (2000) Factors related to the progression of myopia in Singaporean children. Optom Vis Sci 77:549–554
Correction of Myopia Evaluation Trial 2 Study Group for the Pediatric Eye Disease Investigator Group; Gwiazda J, Chandler DL, Cotter SA et al (2011) Progressive-addition lenses versus single-vision lenses for slowing progression of myopia in children with high accommodative lag and near esophoria. Invest Ophthalmol Vis Sci 52:2749–2757. https://doi.org/10.1167/iovs.10-6631
Berntsen DA, Sinnott LT, Mutti DO, Zadnik K (2012) A randomized trial using progressive addition lenses to evaluate theories of myopia progression in children with a high lag of accommodation. Invest Ophthalmol Vis Sci 53:640–649. https://doi.org/10.1167/iovs.11-7769
Shen J, Clark CA, Soni PS, Thibos LN (2010) Peripheral refraction with and without contact lens correction. Optom Vis Sci 87:642–655. https://doi.org/10.1097/OPX.0b013e3181ea16ea
Acknowledgments
The authors would like to thank Peter Bonney for proofreading the article.
Funding
CooperVision S.L. Spain provided financial support. CooperVision S.L. provided the study contact lenses and the funding to carry out the clinical trial.
The sponsor had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (CEI-R, Regional Research Ethics Committee of the Community of Madrid, Spain) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Ruiz-Pomeda, A., Pérez-Sánchez, B., Valls, I. et al. MiSight Assessment Study Spain (MASS). A 2-year randomized clinical trial. Graefes Arch Clin Exp Ophthalmol 256, 1011–1021 (2018). https://doi.org/10.1007/s00417-018-3906-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-018-3906-z