Abstract
Purpose
To investigate the evolution of vitreomacular adhesion (VMA) to acute vitreofoveal separation with particular emphasis on cases involving the underlying fovea.
Methods
In this observational case series, of 192 cases in the VMA stage, 51 progressed to acute vitreofoveal separation; this subgroup was divided into those with normal separation (Group I) and those with co-existing macular findings (Group II). All patients were examined using spectral domain-optical coherence tomography (SD-OCT) at regular three-month intervals. We recorded the best-corrected visual acuity (BCVA), the vitreomacular angle of the VMA (nasally and temporally), the horizontal diameter of the VMA, the macular thickness, the integrity of the photoreceptor layer and of the external limiting membrane. The Amsler grid test was used in the intermediate examinations in cases where patients developed symptoms.
Results
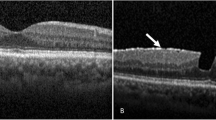
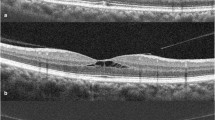
Out of the 51 cases in the VMA stage, 45 (88.2%) progressed to normal spontaneous vitreofoveal separation, while six (11.8%) developed findings of the fovea, such as macular thinning (two cases), an anomalous foveal contour (two cases), a macular tissue defect (one case) and vitreous separation from only the temporal side of the VMA in one case. Foveal findings were the same during the follow-up period in all but one case in which improvement was noted. Differences in BCVA between baseline measurements, those made immediately after vitreofoveal separation, and those made during final examination were not statistically significant. For the whole sample of our study (51 cases), the mean observation time at the VMA stage was 21.8 ±10.6 months, while the mean follow-up time after vitreofoveal separation was 9.7 ±4.9 months. In cases that developed incidents from the fovea, the mean observation time from the baseline to the last examination before vitreofoveal separation was 16.5 ±11.2 months and the mean follow-up time from the diagnosis of vitreofoveal separation to the final examination was 8.5 ±4.4 months.
Conclusions
VMA, excepting its progression to vitreomacular traction or spontaneous release, in a subset of patients can also cause findings associated with the fovea, concomitantly with vitreofoveal separation. Vitreofoveal separation can induce unilateral anatomic distortion of the fovea accompanied by symptoms, such as metamorphopsia or micropsia.







Similar content being viewed by others
References
Bishop PN (2000) Structural macromolecules and supramolecular organization of the vitreous gel. Prog Retin Eye Res 19:323–344
Sebag J (2009) Vitreous: the resplendent enigma. Br J Ophthalmol 93:989–991
Uchino E, Uemura A, Ohba N (2001) Initial stages of posterior vitreous detachment in healthy eyes of older persons evaluated by optical coherence tomography. Arch Ophthalmol 119:1475–1479
Johnson MW (2005) Perifoveal vitreous detachment and its macular complications. Trans Am Ophthalmol Soc 103:537–567
Sebag J (2004) Anomalous posterior vitreous detachment: a unifying concept in vitreo-retinal disease. Graefes Arch Clin Exp Ophthalmol 242:690–698
Girach A, Pakola S (2012) Vitreomacular interface diseases. Pathophysiology, diagnosis and future treatment options. Expert Rev Ophthalmol 7:311–323
Jackson TL, Nicod E, Simpson A, Angelis A, Grimaccia F, Kanavos P (2013) Symptomatic vitreomacular adhesion. Retina 33:1503–1511
Johnson MW (2010) Posterior vitreous detachment: evolution and complications of its early stages. Am J Ophthalmol 149:371–382
Reese AB, Jones IS, Cooper WC (1967) Macular changes secondary to vitreous traction. Am J Ophthalmol 64:544–549
Hikichi T, Yoshida A, Trempe CL (1995) Course of vitreomacular traction syndrome. Am J Ophthalmol 119:55–61
Spaide RF, Wong D, Fisher Y, Goldbaum M (2002) Correlation of vitreous attachment and foveal deformation in early macular hole states. Am J Ophthalmol 133:226–229
Chen TC, Cense B, Pierce MC et al (2005) Spectral domain optical coherence tomography: ultra-high speed, ultra-high resolution ophthalmic imaging. Arch Ophthalmol 123:1715–1720
Bottόs J, Elizalde J, Arevalo JF, Rodrigues EB, Maia M (2012) Vitreomacular traction syndrome. J Ophthalmic Vis Res 7:148–161
Stalmans P, Duker JS, Kaiser PK et al (2013) Oct-based interpretation of the vitreomacular interface and indications for pharmacologic vitreolysis. Retina 33:2003–2011
Duker JS, Kaiser PK, Binder S et al (2013) The international vitreomacular traction study group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology 120:2611–2619
Koizumi H, Spaide RF, Fisher YL et al (2008) Three-dimensional evaluation of vitreomacular traction and epiretinal membrane using spectral-domain optical coherence tomography. Am J Ophthalmol 145:509–517
DeCroos FC, Toth CA, Folgar FA et al (2012) Characterization of vitreoretinal interface disorders using OCT in the interventional phase 3 trials of ocriplasmin. Invest Ophthalmol Vis Sci 53:6504–6511
John VJ, Flynn HW Jr, Smiddy WE et al (2014) Clinical course of vitreomacular adhesion managed by initial observation. Retina 34:442–446
Theodossiadis GP, Grigoropoulos VG, Theodoropoulou S, Datseris I, Theodossiadis PG (2014) Spontaneous resolution of vitreomacular traction demonstrated by spectral-domain optical coherence tomography. Am J Ophthalmol 157:842–851
Gaudric A, Haouchine B, Massin P, Paques M, Blain P, Erginay A (1999) Macular hole formation: new data provided by optical coherence tomography. Arch Ophthalmol 117:744–751
Ma F, Arcinue CA, Barteselli G et al (2014) Optical coherence tomography findings of the vitreoretinal interface in asymptomatic fellow eyes of patients with acute posterior vitreous detachment. Retina 34:447–454
Witkin AJ, Ko TH, Fujimoto JG, Schuman JS, Reichel E, Duker JS (2006) Vitreofoveal attachment causing metamorphopsia: an ultrahigh-resolution optical coherence tomography finding. Retina 26:1085–1087
Theodossiadis PG, Theodossiadis GP, Charonis A, Emfietzoglou I, Grigoropoulos VG, Liarakos VS (2011) The photoreceptor layer as a prognostic factor for visual acuity in the secondary epiretinal membrane after retinal detachment surgery: imaging analysis by spectral-domain optical coherence tomography. Am J Ophthalmol 151:973–980
Grigoropoulos VG, Theodossiadis GP, Theodossiadis PG (2011) Association of the preoperative photoreceptor layer defect as assessed by optical coherence tomography with the functional outcome after macular hole closure: a long follow-up study. Ophthalmologica 225:47–54
Theodossiadis PG, Grigoropoulos VG, Theodossiadis GP (2011) The significance of the external limiting membrane in the recovery of photoreceptor layer after successful macular hole closure: a study by spectral domain optical coherence tomography. Ophthalmologica 225:176–184
Syed YY, Dhillon S (2013) Ocriplasmin: a review of its use in patients with symptomatic vitreomacular adhesion. Drugs 73:1617–1625
de Smet MD, Gandorfer A, Stalmans P et al (2009) Microplasmin intravitreal administration in patients with vitreomacular traction scheduled for vitrectomy: the MIVI I trial. Ophthalmology 116:1349–1355
Stalmans P, Benz MS, Gandorfer A, Kampik A, Girach A, Pakola S, Haller JA, MIVI-TRUST Study Group (2012) Enzymatic vitreolysis with ocriplasmin for vitreomacular traction and macular holes. N Engl J Med 367:606–615
Weng CY, Fortun JA, Carvounis PE, Albini TA (2014) Ocriplasmin and its role in the management of vitreoretinal interface disorders. Int Ophthalmol Clin 54:29–38
Sebag J (2009) Pharmacologic vitreolysis–premise and promise of the first decade. Retina 29:871–874
Conflict of interest
The authors declare no conflict of interest.
There is no need of Clinical Trials.gov registration, as this study is not a trial.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Theodossiadis, G.P., Chatziralli, I.P., Sergentanis, T.N. et al. Evolution of vitreomacular adhesion to acute vitreofoveal separation with special emphasis on a traction-induced foveal pathology. A prospective study of spectral-domain optical coherence tomography. Graefes Arch Clin Exp Ophthalmol 253, 1425–1435 (2015). https://doi.org/10.1007/s00417-014-2826-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-014-2826-9