Abstract
Purpose
To investigate, whether capsulorhexis training on the EYESi surgical simulator improves wet-lab operating performance of surgical novices.
Methods
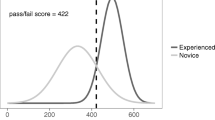
Randomized, masked experimental study. Thirty-one medical students and 32 ophthalmological residents were randomized to either virtual reality (VR) training, or control. Initially and after 3 weeks each participant performed three capsulorhexis tasks in a porcine wet-lab. In between, participants from the VR training groups completed two training trials on the EYESi surgical simulator (VRmagic, Mannheim, Germany). VR training consisted of basic skill tasks and capsulorhexis tasks of increasing difficulty, and preset performance goals had to be reached for each task. All wet-lab procedures (n = 372) were recorded on DVD, and assessed by a masked observer. Each wet-lab capsulorhexis was evaluated with regard to five criteria (circularity, size, centering, time, tissue protection) using a predefined scoring system with a maximum overall score of 10 points (2 per criterion). The primary outcome measure was the intra-individual difference in the average overall performance score between the first and second wet-lab capsulorhexis procedures. Ten operation videos were additionally assessed by three further investigators to determine interobserver agreement.
Results
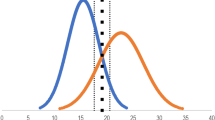
Inter-observer agreement regarding the overall performance score was high (ICC = 0.91). Compared to control groups, VR-trained students and residents showed significant improvement in their median wet-lab capsulorhexis overall performance score compared to controls (+3.67 vs +0.33 points, P = 0.001 and +3.33 vs ±0.00 points, P < 0.0001). The capsulorhexis performance of VR-trained students and residents was also more consistent with a lower standard deviation of scores compared to controls (SD 1.3 vs 2.1 and 1.2 vs 1.7 points respectively).
Conclusions
Structured capsulorhexis training on the EYESi to reach specific target criteria significantly improved wet-lab capsulorhexis performance.




Similar content being viewed by others
References
Feldman BH, Ake JM, Geist CE (2007) Virtual reality simulation. Ophthalmology 114:828
Gallagher AG, Ritter EM, Champion H, Higgins G, Fried MP, Moses G, Smith CD, Satava RM (2005) Virtual reality simulation for the operating room: proficiency-based training as a paradigm shift in surgical skills training. Ann Surg 241:364–372, doi:10.1097/01.sla.0000151982.85062.80
Gerson LB, Van Dam J (2003) A prospective randomized trial comparing a virtual reality simulator to bedside teaching for training in sigmoidoscopy. Endoscopy 35:569–575, doi:10.1055/s-2003-40243
Hahimoto C, Kurosaka D, Uetsuki Y (2001) Teaching continuous curvilinear capsulorhexis using a post-mortem pig eye with simulated cataract. J Cataract Refract Surg 27:814–816, doi:10.1016/S0886-3350(00)00728-8
Hikichi T, Yoshida A, Igarashi S, Mukai N, Harada M, Muroi K, Terada T (2000) Vitreous surgery simulator. Arch Ophthalmol 118:1679–1681
Jonas JB, Rabethge S, Bender HJ (2003) Computer-assisted training system for pars plana vitrectomy. Acta Ophthalmol Scand 81:600–604, doi:10.1046/j.1395-3907.2003.0078.x
Khalifa YM, Bogorad D, Gibson V, Peifer J, Nussbaum J (2006) Virtual reality in ophthalmology training. Surv Ophthalmol 51:259–273, doi:10.1016/j.survophthal.2006.02.005
Laurell CG, Söderberg P, Nordh L, Skarman E, Nordqvist P (2004) Computer-simulated phacoemulsification. Ophthalmology 111:693–698
Mahr MA, Hodge DO (2008) Construct validity of anterior segment anti-tremor and forceps surgical simulator training modules. Attending versus resident surgeon performance. J Cataract Refract Surg 34:980–985, doi:10.1016/j.jcrs.2008.02.015
McClusky DA 3rd, Ritter EM, Lederman AB, Gallagher AG, Smith CD (2005) Correlation between perceptual, visuo-spatial, and psychomotor aptitude to duration of training required to reach performance goals on the MIST-VR surgical simulator. Am Surg 71:13–20 [discussion 20–21]
Merril JR, Notaroberto NF, Laby DM, Rabinowitz AM, Piemme TE (1992) The Ophthalmic Retrobulbar Injection Simulator (ORIS): an application of virtual reality to medical education. Proc Annu Symp Comput Appl Med Care 1992:702–706
Peugnet F, Dubois P, Rouland JF (1998) Virtual reality versus conventional training in retinal photocoagulation: a first clinical assessment. Comput Aided Surg 3:20–26
Ritter EM, McClusky DA 3rd, Gallagher AG, Enochsson L, Smith CD (2006) Perceptual, visuospatial, and psychomotor abilities correlate with duration of training required on a virtual-reality flexible endoscopy simulator. Am J Surg 192:379–384, doi:10.1016/j.amjsurg.2006.03.003
Rossi JV, Verma D, Fujii GY, Lakhanpal RR, Wu SL, Humayun MS, De Juan E Jr (2004) Virtual vitreoretinal surgical simulator as a training tool. Retina 24:231–236, doi:10.1097/00006982-200404000-00007
Rouland JF, Dubois P, Chaillou C, Meseuree P, Karpf S, Godin S, Duquenoy F (1995) SOPHOCLE (Ophthalmologic Simulator of Laser PHOtocoagulation): contribution to virtual reality. J Fr Ophtalmol 18:536–541 [in French]
Schill MA, Wagner C, Hennen M (1999) Eyesi - a simulator for intra-ocular surgery. In: Taylor C, Colchester ACF (eds) Proceedings of the Second International Conference on Medical Image Computing and Computer-Assisted Intervention. Springer Press, Cambridge, UK, p 1679 1166–74
Seymour NE, Gallagher AG, Roman SA, O’Brien MK, Bansal VK, Andersen DK, Satava RM (2002) Virtual reality training improves operating room performance: results of a randomized, double-blinded study. Ann Surg 236:458–463 discussion 463–464, doi:10.1097/00000658-200210000-00008
Shrout PE, Fleiss JL (1979) Intraclass correlations: uses in assessing rater reliability. Psychol Bull 2:420–428, doi:10.1037/0033-2909.86.2.420
Sinclair MJ, Peifer JW, Haleblian R, Luxenberg MN, Green K, Hull DS (1995) Computer-simulated eye surgery. A novel teaching method for residents and practitioners. Ophthalmology 102:517–521
Sugiura T, Kurosaka D, Uezuki Y, Eguchi S, Obata H, Takahashi T (1999) Creating cataract in pig eye. J Cataract Refract Surg 25:615–624
Van Vreeswijk H, Pameyer JH (1998) Inducing cataract in post-mortem pig eyes for cataract surgery training purposes. J Cataract Refract Surg 24:17–18
Verma D, Wills D, Verma M (2003) Virtual reality simulator for vitreoretinal surgery. Eye 17:71–73, doi:10.1038/sj.eye.6700166
Webster R, Sassani J, Shenk R, Good N (2004) A haptic surgical simulator for the continuous curvilinear capsulorhexis procedure during cataract surgery. Stud Health Technol Inform 98:404–406
Webster R, Sassani J, Shenk R, Harris M, Gerber J, Benson A, Blumenstock J, Billman C, Haluck R (2005) Simulating the continuous curvilinear capsulorhexis procedure during cataract surgery on the EYESI system. Stud Health Technol Inform 111:592–595
Author information
Authors and Affiliations
Corresponding author
Additional information
Financial support: VRmagic GmbH, Mannheim, Germany. The sponsor had no role in the design or conduct of this research.
No conflicting relationship exists for any author.
The authors have full control of all primary data, and agree to allow Graefe's Archive for Clinical and Experimental Ophthalmology to review their data upon request.
Rights and permissions
About this article
Cite this article
Feudner, E.M., Engel, C., Neuhann, I.M. et al. Virtual reality training improves wet-lab performance of capsulorhexis: results of a randomized, controlled study. Graefes Arch Clin Exp Ophthalmol 247, 955–963 (2009). https://doi.org/10.1007/s00417-008-1029-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-008-1029-7