Abstract
Disturbances of body orientation perception after brain lesions may specifically relate to only one dimension of space. Stroke patients with “pusher syndrome” suffer from a severe misperception of their body's orientation in the coronal (roll) plane. They experience their body as oriented ‘upright’ when it is in fact markedly tilted to one side. The patients use the unaffected arm or leg to actively push away from the unparalyzed side and resist any attempt to passively correct their tilted body posture. Although pusher patients are unable to correctly determine when their own body is oriented in an upright, vertical position, they seem to have no significant difficulty in determining the orientation of the surrounding visual world in relation to their own body. Pusher syndrome is a distinctive clinical disorder occurring characteristically after unilateral left or right brain lesions in the posterior thalamus and –less frequently– in the insula and postcentral gyrus. These structures thus seem to constitute crucial neural substrates controlling human (upright) body orientation in the coronal (roll) plane. A further disturbance of body orientation that predominantly affects a single dimension of space, namely the transverse (yaw) plane, is observed in stroke patients with spatial neglect. Apparently, our brain has evolved separate neural subsystems for perceiving and controlling body orientation in different dimensions of space.
Similar content being viewed by others
References
Anastasopoulos D, Haslwanter T, Bronstein A, et al. (1997) Dissociation between the performance of body verticality and the visual vertical in acute peripheral vestibular disorder in humans. Neurosci Letters 233:151–153
Arndts F (1924) Zur Frage nach den der Lagewahrnehmung dienenden Sinnesfunktionen. Pflüg Arch Ges Physiol 204:539–540
Azher SN, Jankovic J (2005) Camptocormia: pathogenesis, classification, and response to therapy. Neurology 65:355–359
Beevor CE (1909) Remarks on paralysis of the movements of the trunk in hemiplegia. BMJ:881–885
Bisdorff AR, Wolsley CJ, Anastasopoulos D, et al. (1996) The perception of body verticality (subjective postural vertical) in peripheral and central vestibular disorders. Brain 119:1523–1534
Bjerver K, Silfverskiöld BP (1968) Lateropulsion and imbalance in Wallenberg's syndrome. Acta Neurol Scand 44:91–100
Bohannon RW, Larkin PA (1985) Lower extremity weight bearing under various standing conditions in independently ambulatory patients with hemiparesis. Phys Ther 65:1323–1325
Bohannon RW, Smith MB, Larkin PA (1986) Relationship between independent sitting balance and side of hemiparesis. Phys Ther 66:944–945
Bohning DE, Lomarev MP, Denslow S, et al. (2001) Feasibility of vagus nerve stimulation-synchronized blood oxygenation level-dependent functional MRI. Invest Radiol 36:470–479
Brandt T (1999) Vertigo. Its multisensory syndromes. 2nd Ed. Springer, London
Brandt T, Dieterich M, Danek A (1994) Vestibular cortex lesions affect the perception of verticality. Ann Neurol 35:403–412
Broetz D, Johannsen L, Karnath H-O (2004) Time course of ‘pusher syndrome’ under visual feedback treatment. Physiother Res Int 9:138–143
Brunnstrom S (1970) Movement therapy in hemiplegia. A neurophysiological approach. Harper & Row, New York
Chae JH, Nahas Z, Lomarev M, et al. (2003) A review of functional neuroimaging studies of vagus nerve stimulation (VNS). J Psychiatr Res 37:443–455
Clark B, Graybiel A (1963) Perception of the postural vertical in normals and subjects with labyrinthine defects. J Exp Psychol 65:490–494
Clement G, Gurfinkel VS, Lestienne F, et al. (1984) Adaptation of postural control to weightlessness. Exp Brain Res 57:61–72
Clement G, Vieville T, Lestienne F, et al. (1987) Adaptive modifications of posture and oculomotor reflexes in microgravity. In: Three Decades of Life Science Research. NASA Life Sciences, Washington, pp 216–217
Danells CJ, Black SE, Gladstone DJ, et al. (2004) Poststroke “pushing”: natural history and relationship to motor and functional recovery. Stroke 35:2873–2878
Davies PM (1985, 2000) Steps to follow. A guide to the treatment of adult hemiplegia. Springer, New York
Dettmann MA, Linder MT, Sepic SB (1987) Relationships among walking performance, postural stability, and functional assessment of the hemiplegic patient. Am J Phys Med 66:77–90
Dieterich M, Brandt T (1992) Wallenberg's syndrome: lateropulsion, cyclorotation, and subjective visual vertical in thirty-six patients. Ann Neurol 31:399–408
Dietz V, Berger W (1984) Interlimb coordination of posture in patients with spastic paresis. Impaired function of spinal reflexes. Brain 107:965–978
Engelborghs S, Marien P, Martin JJ, et al. (1998) Functional anatomy, vascularisation and pathology of the human thalamus. Acta Neurol Belg 98:252–265
Friedmann G (1970) The judgement of the visual vertical and horizontal with peripheral and central vestibular lesions. Brain 93:313–328
Garten S (1920) Über die Grundlagen unserer Orientierung im Raume. Abhandl Sächs Akad Wissensch 36:431– 51
Heilman KM, Watson RT, Valenstein E, et al. (1983) Localization of lesions in neglect. In: Kertesz A (ed) Localization in Neuropsychology. Academic Press, New York, pp 471–492
Horak FB, Esselman P, Anderson ME, et al. (1984) The effects of movement velocity, mass displaced, and task certainty on associated postural adjustments made by normal and hemiplegic individuals. J Neurol Neurosurg Psychiatry 47:1020–1028
Johannsen L, Broetz D, Naegele T, et al. (2006) “Pusher syndrome” following cortical lesions that spare the thalamus. J Neurol 253:455–463
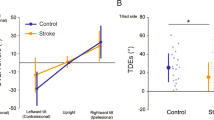
Johannsen L, Fruhmann Berger M, Karnath H-O (2006) Subjective visual vertical (SVV) determined in a representative group of 15 patients with pusher syndrome. J Neurol 253:1367–1369
Johannsen L, Broetz D, Karnath H-O (2006) Leg orientation as a clinical sign. I for pusher syndrome. BMC Neurology 6:30
Jones EG (1985) The Thalamus. Plenum Press, New York
Karnath H-O, Broetz D (2003) Understanding and treating “pusher syndrome”. Phys Ther 83:1119–1125
Karnath H-O, Dieterich M (2006) Spatial neglect - a vestibular disorder? Brain 129:293–305
Karnath H-O, Ferber S, Dichgans J (2000) The neural representation of postural control in humans. Proc Natl Acad Sci USA 97:13931–13936
Karnath H-O, Ferber S, Dichgans J (2000) The origin of contraversive pushing: evidence for a second graviceptive system in humans. Neurology 55:1298–1304
Karnath H-O, Johannsen L, Broetz D, et al. (2002) Prognosis of contraversive pushing. J Neurol 249:1250–1253
Karnath H-O, Fruhmann Berger M, Küker W, et al. (2004) The anatomy of cortical neglect based on voxelwise statistical analysis: a study of 140 patients. Cerebral Cortex 14:1164–1172
Karnath H-O, Johannsen L, Broetz D, et al. (2005) Posterior thalamic hemorrhage induces “pusher syndrome”. Neurology 64:1014–1019, Erratum 65:819
Kerkhoff G, Zoelch C (1998) Disorders of visuospatial orientation in the frontal plane in patients with visual neglect following right or left parietal lesions. Exp Brain Res 122:108–120
Lafosse C, Kerckhofs E, Troch M, et al. (2005) Contraversive pushing and inattention of the contralesional hemispace. J Clin Exp Neuropsychol 27:460–484
Lösslein H, Kolster F (2001) Posturaler Hemineglect – Neubewertung des Pushersyndroms und Vorschläge für die Therapie. Krankengymnastik 53:17–24
Mann CW, Berthelot-Berry NH, Dauterive HJ (1949) The perception of the vertical: I. Visual and non-labyrinthine cues. J Exp Psychol 39:538–547
Masdeu JC, Gorelick PB (1988) Thalamic astasia: inability to stand after unilateral thalamic lesions. Ann Neurol 23:596–603
Massion J, Fabre J-C, Mouchnino L, et al. (1995) Body orientation and regulation of the center of gravity during movement under water. J Vestibul Res 5:211–221
Mittelstaedt H (1992) Somatic versus vestibular gravity reception in man. Ann NY Acad Sci 656:124–139
Mittelstaedt H (1998) Origin and processing of postural information. Neurosci Biobehav Rev 22:473–478
Mort DJ, Malhotra P, Mannan SK, et al. (2003) The anatomy of visual neglect. Brain 126:1986–1997
Narayanan JT, Watts R, Haddad N, et al. (2002) Cerebral activation during vagus nerve stimulation: a functional MR study. Epilepsia 43:1509–1514
Nieves AV, Miyasaki JM, Lang AE (2001) Acute onset dystonic camptocormia caused by lenticular lesions. Mov Disord 16:177–180
Palmer E, Downes L, Ashby P (1996) Associated postural adjustments are impaired by a lesion of the cortex. Neurology 46:471–475
Pedersen PM, Wandel A, Jorgensen HS, et al. (1996) Ipsilateral pushing in stroke: incidence, relation to neuropsychological symptoms, and impact on rehabilitation. The Copenhagen stroke study. Arch Phys Med Rehabil 77:25–28
Pérennou DA, Leblond C, Amblard B, et al. (2000) The polymodal sensory cortex is crucial for controlling lateral postural stability: evidence from stroke patients. Brain Res Bulletin 53:359–365
Pérennou DA, Leblond C, Amblard B, et al. (2001) Transcutaneous electrical nerve stimulation reduces neglect-related postural instability after stroke. Arch Phys Med Rehabil 82:440–448
Pérennou DA, Amblard B, Laassel EM, et al. (2002) Understanding the pusher behavior of some stroke patients with spatial deficits: a pilot study. Arch Phys Med Rehabil 83:570–575
Perry J (1969) The mechanics of walking in hemiplegia. Clin Orthop 63:23–31
Premoselli S, Cesana L, Cerri C (2001) Pusher syndrome in stroke: clinical, neuropsychological and neurophysiological investigation. Eur Med Phys 37:143–151
Punt TD, Riddoch MJ (2002) Towards a theoretical understanding of pushing behaviour in stroke patients. Neuropsych Rehabil 12:455–472
Santos-Pontelli TEG, Pontes-Neto OM, Colafêmina JF, et al. (2004) Contraversive pushing in non-stroke patients. J Neurol 251:1324–1328
Santos-Pontelli TEG, Pontes-Neto OM, Colafêmina JF, et al. (2005) Posture control in pusher syndrome: influence of lateral semicircular canals. Rev Bras Otorrinolaringol 71:448–452
Saj A, Honore J, Coello Y, et al. (2005) The visual vertical in the pusher syndrome: influence of hemispace and body position. J Neurol 252:885–891
Saj A, Honore J, Bernati T, et al. (2005) Subjective visual vertical in pitch and roll in right hemispheric stroke. Stroke 36:588–591
Spinazzola L, Cubelli R, Della Sala S (2003) Impairments of trunk movements following left or right hemisphere lesions: dissociation between apraxic errors and postural instability. Brain 126:2656–2666
Teuber H-L, Mishkin M (1954) Judgment of visual and postural vertical after brain injury. J Psychol 38:161–175
Vibert D, Häusler R, Safran AB (1999) Subjective visual vertical in peripheral unilateral vestibular diseases. J Vestib Res 9:145–152
Wing AM, Goodrich S, Virji-Babul N, et al. (1993) Balance evaluation in hemiparetic stroke patients using lateral forces applied to the hip. Arch Phys Med Rehabil 74:292–299
Yelnik AP, Lebreton FO, Bonan IV, et al. (2002) Perception of verticality after recent cerebral hemispheric stroke. Stroke 33:2247–2253
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Karnath, HO. Pusher Syndrome – a frequent but little-known disturbance of body orientation perception. J Neurol 254, 415–424 (2007). https://doi.org/10.1007/s00415-006-0341-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-006-0341-6