Abstract
Purpose
Pulmonary aspiration of gastric refluxate is one of the indications for anti-reflux surgery. Effectiveness of surgery in preventing pulmonary aspiration post-operatively has not been previously tested. The aim of this project is to assess effectiveness of anti-reflux surgery on preventing pulmonary aspiration of gastric refluxate.
Methods
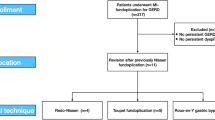
Retrospective analysis of prospectively populated database of patients with confirmed aspiration of gastric refluxate on scintigraphy. Patients that have undergone anti-reflux surgery between 01/01/2014 and 31/12/2015 and had scintigraphy post-operatively were included. Objective data such as resolution of aspiration, degree of proximal aero-digestive contamination, surgical complications and oesophageal dysmotility as well as patient quality of life data were analysed.
Results
Inclusion criteria were satisfied by 39 patients (11 male and 28 female). Pulmonary aspiration was prevented in 24 out of 39 patients (61.5%) post-operatively. Significant reduction of isotope contamination of upper oesophagus supine and upright (p = 0.002) and pharynx supine and upright (p = 0.027) was confirmed on scintigraphy post-operatively. Severe oesophageal dysmotility was strongly associated with continued aspiration post-operatively OR 15.3 (95% CI 2.459–95.194; p = 0.02). Majority (24/31, 77%) of patients were satisfied or very satisfied with surgery, whilst 7/31 (23%) were dissatisfied. Pre-operative GIQLI scores were low (mean 89.77, SD 20.5), modest improvements at 6 months (mean 98.4, SD 21.97) and deterioration at 12 months (mean 88.41, SD 28.07) were not significant (p = 0.07).
Conclusion
Surgery is partially effective in reversing pulmonary aspiration of gastric refluxate on short-term follow-up. Severe oesophageal dysmotility is a predictor of inferior control of aspiration with surgery.



Similar content being viewed by others

References
Barry DW, Vaezi MF (2010) Laryngopharyngeal reflux: more questions than answers. Clevel Clin J Med 77(5):327–334. https://doi.org/10.3949/ccjm.77a.09121
Falk GL, Beattie J, Ing A, Falk SE, Magee M, Burton L, Van der Wall H (2015) Scintigraphy in laryngopharyngeal and gastroesophageal reflux disease: a definitive diagnostic test? World J Gastroenterol 21(12):3619–3627. https://doi.org/10.3748/wjg.v21.i12.3619
Postma GN, Halum SL (2006) Laryngeal and pharyngeal complications of gastroesophageal reflux disease. GI Motil Online. https://doi.org/10.1038/gimo46
Koufman JA, Aviv JE, Casiano RR, Shaw GY (2002) Laryngopharyngeal reflux: position statement of the committee on speech, voice, and swallowing disorders of the American Academy of Otolaryngology-Head and Neck Surgery. Otolaryngology 127(1):32–35
Blondeau K, Mertens V, Vanaudenaerde BA, Verleden GM, Van Raemdonck DE, Sifrim D, Dupont LJ (2008) Gastro-oesophageal reflux and gastric aspiration in lung transplant patients with or without chronic rejection. Eur Respir J 31(4):707–713. https://doi.org/10.1183/09031936.00064807
Lee JS, Collard HR, Raghu G, Sweet MP, Hays SR, Campos GM, Golden JA, King TE (2010) Does chronic microaspiration cause idiopathic pulmonary fibrosis? Am J Med 123(4):304–311. https://doi.org/10.1016/j.amjmed.2009.07.033
Vaezi MF (2009) Extraesophageal Reflux. Plural Publishing, San Diego
Luketich JD (2014) Master techniques in surgery: esophageal surgery. Wolters Kluwer Health, Philadelphia
Martinucci I, de Bortoli N, Savarino E, Nacci A, Romeo SO, Bellini M, Savarino V, Fattori B, Marchi S (2013) Optimal treatment of laryngopharyngeal reflux disease. Ther Adv Chronic Dis 4(6):287–301. https://doi.org/10.1177/2040622313503485
Eypasch E, Williams JI, Wood-Dauphinee S, Ure BM, Schmulling C, Neugebauer E, Troidl H (1995) Gastrointestinal Quality of Life Index: development, validation and application of a new instrument. Br J Surg 82(2):216–222
Belafsky PC, Postma GN, Koufman JA (2001) The validity and reliability of the reflux finding score (RFS). Laryngoscope 111(8):1313–1317. https://doi.org/10.1097/00005537-200108000-00001
Gibson SC, Wong SK, Dixon AC, Falk GL (2013) Laparoscopic repair of giant hiatus hernia: prosthesis is not required for successful outcome. Surg Endosc 27(2):618–623. https://doi.org/10.1007/s00464-012-2501-3
Falk M, Van der Wall H, Falk GL (2015) Differences between scintigraphic reflux studies in gastrointestinal reflux disease and laryngopharyngeal reflux disease and correlation with symptoms. Nucl Med Commun 36(6):625–630. https://doi.org/10.1097/mnm.0000000000000289
Kahrilas PJ, Dodds WJ, Hogan WJ, Kern M, Arndorfer RC, Reece A (1986) Esophageal peristaltic dysfunction in peptic esophagitis. Gastroenterology 91(4):897–904
Khoma O, Burton L, VanderWall H, Falk M, Falk GL (2017) Pathophysiology of laryngopharyngeal reflux disease: association with pulmonary aspiration on scintigraphy and abnormal oesophageal motility disease (under review)
McShane PJ, Naureckas ET, Tino G, Strek ME (2013) Non-cystic fibrosis bronchiectasis. Am J Respir Crit Care Med 188(6):647–656. https://doi.org/10.1164/rccm.201303-0411CI
Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R (2006) The montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol 101(8):1900–1920. https://doi.org/10.1111/j.1572-0241.2006.00630.x (quiz 1943)
Catania RA, Kavic SM, Roth JS, Lee TH, Meyer T, Fantry GT, Castellanos PF, Park A (2007) Laparoscopic Nissen fundoplication effectively relieves symptoms in patients with laryngopharyngeal reflux. J Gastrointest Surg 11(12):1579–1587. https://doi.org/10.1007/s11605-007-0318-5 (discussion 1587–1578)
Garg SK, Gurusamy KS (2015) Laparoscopic fundoplication surgery versus medical management for gastro-oesophageal reflux disease (GORD) in adults. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD003243.pub3
Pearson JP, Parikh S, Orlando RC, Johnston N, Allen J, Tinling SP, Johnston N, Belafsky P, Arevalo LF, Sharma N, Castell DO, Fox M, Harding SM, Morice AH, Watson MG, Shields MD, Bateman N, McCallion WA, van Wijk MP, Wenzl TG, Karkos PD, Belafsky PC (2011) Review article: reflux and its consequences–the laryngeal, pulmonary and oesophageal manifestations. Conference held in conjunction with the 9th International Symposium on Human Pepsin (ISHP) Kingston-upon-Hull, UK, 21–23 April 2010. Aliment Pharmacol Ther 33(Suppl 1):1–71. https://doi.org/10.1111/j.1365-2036.2011.04581.x
Ludemann JP, Manoukian J, Shaw K, Bernard C, Davis M, al-Jubab A (1998) Effects of simulated gastroesophageal reflux on the untraumatized rabbit larynx. J Otolaryngol 27(3):127–131
Giuliano C, Wilhelm SM, Kale-Pradhan PB (2012) Are proton pump inhibitors associated with the development of community-acquired pneumonia? A meta-analysis. Expert Rev Clin Pharmacol 5(3):337–344. https://doi.org/10.1586/ecp.12.20
Xie Y, Bowe B, Li T, Xian H, Yan Y, Al-Aly Z (2017) Risk of death among users of proton pump inhibitors: a longitudinal observational cohort study of United States veterans. BMJ Open. https://doi.org/10.1136/bmjopen-2016-015735
Jobe BA, Richter JE, Hoppo T, Peters JH, Bell R, Dengler WC, DeVault K, Fass R, Gyawali CP, Kahrilas PJ, Lacy BE, Pandolfino JE, Patti MG, Swanstrom LL, Kurian AA, Vela MF, Vaezi M, DeMeester TR (2013) Preoperative diagnostic workup before antireflux surgery: an evidence and experience-based consensus of the Esophageal Diagnostic Advisory Panel. J Am Coll Surg 217(4):586–597. https://doi.org/10.1016/j.jamcollsurg.2013.05.023
Ravi K, Katzka DA (2016) Esophageal Impedance Monitoring: Clinical Pearls and Pitfalls. Am J Gastroenterol 111(9):1245–1256. https://doi.org/10.1038/ajg.2016.256
Cowgill SM, Gillman R, Kraemer E, Al-Saadi S, Villadolid D, Rosemurgy A (2007) Ten-year follow up after laparoscopic Nissen fundoplication for gastroesophageal reflux disease. Am Surg 73(8):748–752 (discussion 752–743)
Fumagalli U, Bona S, Battafarano F, Zago M, Barbera R, Rosati R (2008) Persistent dysphagia after laparoscopic fundoplication for gastro-esophageal reflux disease. Dis Esophagus 21(3):257–261. https://doi.org/10.1111/j.1442-2050.2007.00773.x
Birring SS, Prudon B, Carr AJ, Singh SJ, Morgan MD, Pavord ID (2003) Development of a symptom specific health status measure for patients with chronic cough: Leicester Cough Questionnaire (LCQ). Thorax 58(4):339–343
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Khoma, O., Falk, S.E., Burton, L. et al. Gastro-Oesophageal Reflux and Aspiration: Does Laparoscopic Fundoplication Significantly Decrease Pulmonary Aspiration?. Lung 196, 491–496 (2018). https://doi.org/10.1007/s00408-018-0128-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-018-0128-4