Abstract
Essential hypertension, insulin resistance, heart failure, congestion, diuretic resistance, and functional renal disease are all characterized by excessive central sympathetic drive. The contribution of the kidney’s somatic afferent nerves, as an underlying cause of elevated central sympathetic drive, and the consequences of excessive efferent sympathetic signals to the kidney itself, as well as other organs, identify the renal sympathetic nerves as a uniquely logical therapeutic target for diseases linked by excessive central sympathetic drive. Clinical studies of renal denervation in patients with resistant hypertension using an endovascular radiofrequency ablation methodology have exposed the sympathetic link between these conditions. Renal denervation could be expected to simultaneously affect blood pressure, insulin resistance, sleep disorders, congestion in heart failure, cardiorenal syndrome and diuretic resistance. The striking epidemiologic evidence for coexistence of these disorders suggests common causal pathways. Chronic activation of the sympathetic nervous system has been associated with components of the metabolic syndrome, such as blood pressure elevation, obesity, dyslipidemia, and impaired fasting glucose with hyperinsulinemia. Over 50% of patients with essential hypertension are hyperinsulinemic, regardless of whether they are untreated or in a stable program of treatment. Insulin resistance is related to sympathetic drive via a bidirectional mechanism. In this manuscript, we review the data that suggests that selective impairment of renal somatic afferent and sympathetic efferent nerves in patients with resistant hypertension both reduces markers of central sympathetic drive and favorably impacts diseases linked through central sympathetics—insulin resistance, heart failure, congestion, diuretic resistance, and cardiorenal disorders.
Similar content being viewed by others
Introduction
The contribution of renal somatic afferent nerves to central sympathetic drive and the impact of excessive efferent sympathetic signaling to the kidney are intimately linked to the development of several chronic diseases associated with such sympathetic excess [1, 2]. These chronic ailments, essential hypertension, insulin resistance, congestion, diuretic resistance and cardiorenal disorders, have a multiplicity of underlying etiologies, yet their shared link with elevated central sympathetic drive identifies a common therapeutic target [3–5]. Therefore, treatment of the elevated sympathetic activity would be anticipated to provide significant clinical benefit. Recently, a new approach to selectively denervate the kidneys by ablation of efferent sympathetic and afferent somatic fibers has been established in clinical practice [6]. This article summarizes the chronic diseases linked by increased central sympathetic drive by describing the organ specific consequences of increased efferent signaling, and further suggests a common role of renal somatic afferents in elevation of central drive.
Renal somatic afferent nerve activity as a source of central sympathetic drive
The sophisticated network of afferent and efferent sensory, chemo- and baroreceptor nerve fibers, lie netlike in the adventitia of the renal artery (Fig. 1) and throughout the kidney [7]. Their signaling pathway to the hypothalamus provides the basis for targeting these nerves’ as modulators of central integration in the brain stem [2] (Fig. 2). Altering the signals from the kidney to the hypothalamus is expected to impact peripherally, including on arterial resistance, the venous capacitance vasculature, peripheral and central chemoreceptors, sympathetic activity of the kidney, the liver and of course the heart itself [8]. Reduction of central sympathetic tone is therefore expected to simultaneously impact the plethora of systemic disorders linked through inappropriately high central sympathetic activity. Activation of renal sensory afferent signaling is likely caused by various stimuli such as renal ischemia, hypoxia, and oxidative stress as well as intrinsic renal diseases [2]. In the 5/6 nephrectomy rat model of chronic renal failure and hypertension dorsal rhizotomy prevented blood pressure elevation indicating that afferent signaling from the diseased kidney to central integrative structures contributes to the rise in blood pressure in kidney disease [9]. Renal injury caused by unilateral phenol injection reliably causes hypertension in rats and is associated with both an increase in norepinephrine secretion from the posterior hypothalamus and increased renal sympathetic efferent and afferent nerve activity of both kidneys [10]. Surgical renal denervation of the phenol-treated kidney prevents hypothalamic-mediated rises in noradrenaline and increases in blood pressure, while restoring vascular resistance to normal. These findings have been confirmed in several other models of renal disease as well as interventions targeting the sympathetic nervous system, thereby demonstrating the crucial role of both efferent and afferent renal nerve signaling in hypertension associated with chronic kidney disease [11]. Experiments based on the same principles conducted in humans using nephrectomy in end stage renal disease patients with and without transplant have demonstrated similar findings [12]. Nephrectomy of the native non-functioning kidney has resulted in reduction of muscle sympathetic nerve activity, reduction of total body noradrenaline spillover, reducing blood pressure and calf vascular resistance, confirming the role of the diseased kidney in mediating central sympathetic tone.
The invasive nature of nephrectomy or spinal rhizotomy has recently been superseded by endovascular renal specific denervation of native kidney using low power radiofrequency in end stage renal disease patients either on dialysis or post transplant as well as patients with hypertension resistant to pharmacologic therapy [13]. Following endovascular denervation, blood pressure fell significantly, and, when measured, muscle sympathetic nerve activity had returned to normal post denervation [14–16]. Similar findings of reduced total body noradrenaline spillover and reduced muscle sympathetic nerve frequency in resistant hypertension patients without evident renal disease suggest the renal chemo- or baroreceptors are responding to stimuli other than overt renal damage, possibly local metabolites of ischemia or hypoxia [14]. While renal generated NO, adenosine, and angiotensin II may be responsive to changes in central nervous system status, these animal and human experiments strongly identify a direct neurologic link. These numerous observations, confirm the native kidney as a neurologic progenitor of signals to the central sympathetic nervous system.
Consequences of increased central sympathetic tone
Increased renal sensory afferent signaling, following its integration in the posterior hypothalamus, directly influences central sympathetic outflow, not only restricted to the kidneys but evident throughout the entirety of the sympathetic system [1] (Fig. 3). Outbound sympathetic nerve fibers innervate all organs that are involved in the direct control of peripheral vascular resistance, management of central and peripheral chemo receptors, directly influence cardiovascular contractility, heart rate and rhythm, management of total body salt and water through both renal mechanisms and control of intravascular circulating blood volume through alterations in tone of the splanchnic storage vessels and of course the kidney itself [2]. Thus, reduction of excessive central sympathetic activity, following the selective removal of renal signals to the hypothalamus, is therapeutically attractive in the treatment of disorders commonly linked by sympathetic over-activity [17]. The consequences of elevated central sympathetic drive underlie the many diseases that are found to cluster with hypertension and systolic heart failure, such as insulin resistance, sleep disorders, diuretic resistance and congestion [18].
Specific consequences of increased sympathetic efferent signaling to the kidney
The sympathetic nerves to the kidneys terminate in the blood vessels, the juxtaglomerular apparatus, and the renal tubules [19]. Stimulation of the renal sympathetic nerves cause increased renin release, increased sodium reabsorption, and a reduction of renal blood flow [2]. These nerves, exclusively noradrenergic, have a graded response to nerve stimulation including increased renin secretion rate; increased proximal tubular sodium reabsorption; and direct adrenergic-mediated increases in renal vascular resistance. It has been discussed that essential hypertension is largely neurogenic, both initiated and sustained by sympathetic nervous system over-activity proved with studies using radiotracer dilution methodology measuring spillover of noradrenaline from the kidney to plasma [3, 20–22]. Beyond essential hypertension, efferent sympathetic traffic is logically linked with the three major physiologic features identified as the renal component of the “cardiorenal syndrome” [23, 24]: excess renin release, rightward shift of the pressure-natriuresis relation and reduced renal blood flow and glomerular filtration rates. These three consequences of heightened sympathetic tone to the kidney portend heightened morbidity and mortality rates.
Efferent sympathetic nerve activity is increased in systolic heart failure, as demonstrated by an excessive increase of noradrenaline synaptic spillover to plasma from both the heart and kidney [23]. Intravenous infusion of the centrally acting alpha adrenoceptor agonist clonidine, at modest doses, significantly attenuates cardiac and renal sympathetic tone in heart failure patients [25]. Beyond the noted beneficial cardiac effects of antiadrenergic therapy in heart failure, the renal sympatholytic effects counteract direct neuro-mediated tubular salt retention. Consistent with this notion is the predictive value of renal sympathetic activation on all-cause mortality or need for heart transplant in patients with congestive heart failure [26]. The contribution of increased renal noradrenaline spillover in heart failure as a predictor of mortality is independent of overall sympathetic activity, glomerular filtration rate, and left ventricular ejection fraction [23]. Evidence-based treatment with beta-blockers in patients with chronic heart failure reduces morbidity and mortality, due to blockade of the effects of excessive sympathetic activation on the heart [27, 28]. These findings suggest treatment strategies that further reduce renal sympathetic activation, and in particular renal sympathetic efferent signals, have the potential to improve survival in patients with heart failure.
Both advanced chronic kidney disease and end stage renal disease are characterized by heightened efferent sympathetic nervous system activation [29]. Centrally acting sympatholytic agents, such as moxonidine delay the progression of renal failure, and reduces MSNA in normotensive patients with type I diabetes mellitus, in the absence of blood pressure changes [7, 30, 31].
Consequences of chronic elevated central sympathetic tone
Essential hypertension
Bilateral renal denervation prevents or attenuates the development of hypertension in a large number of diverse animal models of experimental hypertension including genetic, salt sensitive, obesity related, renovascular, and other hypertension models [2, 32–34]. Only models of volume expansion with hormonal activation, such as the one-kidney, one-clip model of hypertension, are associated with elevated blood pressure in the absence of involvement of the renal sympathetic axis [35]. In other models, the renal sympathetic axis causes, promotes or sustains blood pressure across species and hypertension models. These findings corroborate the notion that renal sympathetic nerves represent a critical link between the sympathetic nervous system and the kidney in essential hypertension.
Approximately 70% of incident hypertension is associated with overweight and obesity [36]. The potential for renal denervation to treat obesity-related hypertension has been investigated in a chronically instrumented, high-fat fed dog model, which is characterized by sodium retention and increased sympathetic nervous system activation [34]. Whilst the high fat diet resulted in a 50% increase in body mass in both control and denervated dogs, blood pressure increased significantly only in the control but not in the denervated dogs. Furthermore, sodium retention was reduced by 50% in the denervated dogs. Extension of this principle to man has been demonstrated in the Symplicity HTN-2 trial of therapeutic renal denervation in resistant hypertension. Patients failing to attain blood pressure control, despite an average of more than five medications, experienced a 6 months reduction of office blood pressure by −32/−12 mmHg compared to well-matched controls [16]. With a mean body mass index of 31 kg/m [2] most of the included patients were overweight or obese. The reduction of blood pressure alone is anticipated to have significant impact on the risk of developing cardiovascular diseases in these patients.
Obstructive sleep apnea in resistant hypertension
Obstructive sleep apnea, often considered a cause of resistance in patients with essential hypertension, may also be a consequence of increased central sympathetic tone [37, 38]. A recent observational series of patients with sleep study pre and post renal denervation for resistant hypertension suggests that denervation and/or blood pressure reduction alone reduces the frequency of apneic–hypopneic episodes [39]. Reduction of renal mediated salt and water expansion, a consequence of reducing renal sympathetic efferent signaling and neurologic mediated volume expansion [38], could be expected to reduce the occurrence or severity of obstructive sleep apnea in patients with overt or those with subtle volume expansion. Patients with obstructive sleep apnea have elevated muscle sympathetic nerve activity [40], which is reduced following adequate treatment of the obstruction. The suggestion that it is the over-activity of the sympathetic system that underlies some of the obstruction needs further testing.
Insulin resistance
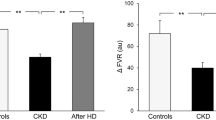
That insulin resistance has been found in lean as well as in weight matched hypertensives suggests that insulin resistance is related to the basic determinates of blood pressure [41]. Julius et al. [42] proposed in 1991 that pressure induced restriction of the microcirculation limits nutritional flow, and thereby impairs glucose uptake in the skeletal muscle. While other factors are likely operative, two recent studies have observed profound changes in insulin resistance following renal denervation for the treatment of resistant hypertension [43, 44]. Euglycemic hyperinsulinemic clamp studies in conjunction with assessment of total body noradrenaline spillover and muscle sympathetic nerve activity before and after renal denervation in patients with polycystic ovary syndrome demonstrated an association between reduction of total body spillover, sympathetic nerve activity and improved insulin sensitivity measured with clamp [44]. A second and larger series, in resistant hypertensive patients undergoing renal denervation has documented a dramatic change in fasting insulin, C-peptide and calculated HOMA-IR with 20% of patients were documented to improve diabetic status (from glucose intolerance to normal or from diabetes to glucose intolerance) 3 months after renal denervation [43]. Beyond questions of insulin level and diabetic risk, the application of renal denervation to prevent development of structural renal changes due to early diabetic nephropathy has previously been explored [45]. Functional and anatomic studies performed 2 weeks after the onset of streptozotocin-induced diabetes in denervated rats revealed attenuation of physiologic and anatomic findings of early diabetic nephropathy. Studies in humans demonstrated that sympathoinhibition with the centrally acting drug moxonidine reduced microalbuminuria in normotensive patients with type 1 diabetes, in the absence of any significant blood pressure changes [30]. Both the change in diabetic state and the profound reduction of insulin levels in these initial reports may have profound implications on cardiovascular risk. The calculated 10-year change in cardiovascular risk associated with blood pressure reduction and improvement in diabetic state appears to be more than additive. Preclinical observations on renal protection against diabetic glomerular sclerosis coupled with the human data on renal denervation resulting in reduced blood pressure with improved insulin sensitivity justify additional study in this area.
Congestion
Heart failure associated with reduced systolic function or congestion (or both) is characterized by substantial neuro-hormonal activation in heart, kidney and skeletal muscle [23, 46]. These neurohumoral responses include activation of the sympathetic nervous system and the renin–angiotensin–aldosterone system, further aggravating heart failure by increasing ventricular afterload and preload. Initial measures of serum noradrenaline verified an inverse relation between serum levels and mortality, which was initially hypothesized to be a hormonal marker of hemodynamic stress, and later with the appreciation of the value of beta blockers to improve morbidity and mortality in heart failure, felt to itself be a mediator of the increased mortality rates [47, 48]. Moreover, renal noradrenaline spillover is an independent predictor of heart transplant free survival; patients with elevated serum norepinephrine experience rates of mortality three times higher in untreated than treated heart failure patients [2, 23, 49]. Renal sympathetic efferent traffic can underlie congestion due to frequency dependent release of renin, sodium retention in the proximal tubules and elevation of renal vascular resistance [2]. Renin release, and subsequent generation of local angiotensin II directly stimulates proximal tubular sodium reabsorption by activating sodium bicarbonate co-transporters and sodium hydrogen exchange [50] and also by causing vasoconstriction of the efferent renal arteriole, lowering peritubular hydrostatic pressure [51]. Aldosterone, acting within the distal tubule and collecting duct, up-regulates and activates the basolateral Na/K pumps retaining remaining intraluminal Na. The clinical importance of the sympathetically mediated impact on fluid retention is evident even after standing, which increases renal sympathetic efferent signaling in heart failure and hepato renal syndrome [2]. Upright posture alone decreases eGFR and raises plasma concentrations of noradrenaline, renin and aldosterone in both hepato renal and heart failure patients [52]. The effects of chronic activation of efferent renal signaling on total body Na and water balance are likely critical in edema and congestion formation. The natriuretic peptides are considered markers of volume expansion, however, they may also serve as indicators of excess renal efferent signaling [53]. The natriuretic actions of natriuretic peptides are reduced in heart failure. Thematically, the family of natriuretic peptides may represent compensation to the anti natriuretic consequences of renal sympathetic activity and other activated vasoconstrictor systems. Experimental ligation of renal nerves protects against development of postprandial natriuretic resistance and the development of congestion or rises in ventricular filling pressures [54]. The therapeutic value of renal denervation in heart failure was evaluated in a similar experimental model of coronary ligation induced myocardial infarction in rats [55]. This study, in which renal denervation was performed pre-onset of myocardial infarction, demonstrated reduced ventricular filling pressure and improved ventricular function compared to non-denervated controls [55]. More recently, evidence from a rabbit model with pacing induced heart failure demonstrated that the reduction in renal blood flow and the increase in renal vascular resistance can be prevented by surgical renal denervation, indicating that renal sympathetic nerve activity elicits a detrimental effect on renal blood flow [56]. Equally important in this later study, expression of angiotensin receptors was found to be dependent on sympathetic innervation [57]. Beyond renal management of volume, the appreciation that circulating blood volume can abruptly be altered by neurologically recruiting splanchnic venous storage blood pools suggests that increased central sympathetic drive has potential to both increase total body salt and water through renal mechanisms as well as abruptly change circulating volume by recruiting splanchnic venous stores of blood [2]. This neurogenic mechanism may explain the often clinically frustrating finding in patients who experience dramatic increases in dyspnea and pulmonary congestion in the absence of either weight changes or abnormalities of ventricular function, i.e. sympathetically mediated changes in circulating volume.
Central sympathetic control of sensory afferent receptors—sympathetic underpinnings of central sleep apnea and dyspnea
Like the peripheral pO2 receptor, the central pCO2 receptor set point and gain are sympathetically modifiable [58]; suggesting that the clinical appreciation of dyspnea may reflect sympathetic hyperactivity quite independent of the mechanism by which alveolar and interstitial lung water stimulate interstitial pulmonary juxtacapillary receptors. A leftward shifted set point of the central pCO2 receptor in heart failure is well recognized, as the chronic metabolic alkalosis is ubiquitous, and on occasion the development of central sleep apnea, a manifestation of the shift being so leftward that the trigger point for inspiration is not reached [59]. Certainly, restoring a normal set point and gain of the central pCO2 receptor from the pathological altered set point could obliterate central sleep apnea. Dyspnea is most often considered a consequence of increased alveolar and interstitial lung water, however, it is not significantly improved following diuretic therapy except in the patient with alveolar water [60]. On the other hand, dyspnea is principally a consequence of hypersensitivity to pCO2. If renal denervation can restore normal minute ventilation response to pCO2, then this direct consequence of diastolic and systolic heart failure, i.e. exercise intolerance, may be amenable by renal denervation.
Diuretic resistance and the cardiorenal syndrome
Escalating doses of diuretics are associated with worsening prognosis in heart failure [61, 62]. Although generally interpreted as a sign of worsening intrinsic heart function, the resistance to diuretics, in particular furosemide, may indeed reflect renal sympathetic mediated Na reabsorption proximal to the more distal sites of furosemide action [63]. Thus, congestion and natriuretic resistance may reflect underlying increased renal sympathetic activity. This principle has been previously observed following the increase of renal sympathetic signaling associated with standing in patients with either heart failure or hepatorenal syndrome [52]. The consequences of increased renin release associated with renal sympathetic activity, increased angiotensin II and aldosterone, both act to increase salt and water retention and interfere with pharmacologic intervention [1]. Worsening renal function observed in heart failure patients is associated with increased morbidity and mortality. In a pacing rabbit heart failure model, the elevations of renal resistance and reduction of blood flow observed with the development of heart failure were entirely restored to normal following renal denervation [57]. Additionally, renal AT1R expression was increased by approximately 67% and AT2R expression was decreased by approximately 87% in rabbits with heart failure. In contrast, kidneys from denervated rabbits with heart failure showed a near normalization in the expression of these receptors [57]; suggesting that the renal hormonal milieu is in large part consequent upon underlying renal sympathetic efferent state. The best-described consequence of cardiorenal disease is the staggering prevalence of cardiovascular mortality seen in patients with either chronic or end stage renal disease or both [24]. The possible clinical value of therapeutic native kidney denervation or nephrectomy for the attenuation of cardiovascular disorders remains entirely unexplored, yet the ease and reported safety of the endovascular therapeutic renal denervation may allow this experiment to be conducted with relatively little risk to the end stage renal disease patient.
Tachycardiac arrhythmias
Both atrial and ventricular arrhythmias are associated with sympathetic hyperactivity [64, 65]. The sinus tachycardia of heart failure may represent primary elevations of cardiac efferent signaling. Recent studies of drugs that reduce heart rate without additional systemic effects have demonstrated improvements of cardiovascular mortality in heart failure similar to the findings of beta-blockers, which also reduce heart rate [66, 67]. The ventricular response rate in atrial fibrillation is often an expression of sympathetic state. The underlying ventricular rate in atrial fibrillation has been observed to fall following renal denervation in resistant hypertension (Felix Mahfoud, personal communication). While this may represent changes in myocardial work and stress associated with blood pressure declines, there may also be reductions in direct cardiac sympathetic signaling. Similarly, left stellate cardiac ganglionectomy has been reported to both reduce heart rate and shorten the QT interval [68].
From theory to practice
Reduction of central sympathetic activity following baro-receptor stimulation has been reported with the Rheos baroreceptor stimulator, and this carotid strategy may indeed exhibit similar systemic properties. Further, the reduction of central sympathetic stimulation associated with nerve stimulation from the carotid sinus may result in substantially reduced renal sympathetic efferent signaling [69]. Therapeutic renal denervation has been applied in a controlled randomized trial for the treatment of resistant hypertension with a significant reduction of systolic blood pressure, diastolic pressure and pulse pressure at 6 months [16]. Reduction of insulin resistance has been anticipated in preclinical work, and confirmed in man using gold standard euglycemic hyperinsulinemic clamp and the calculated HOMA-IR in two different models of excess sympathetic state [43, 44]. While this confirms the hypothesis, prospective randomized clinical trials remain to be conducted and are currently underway. Sleep disorders, similarly may be a reflection of the underlying sympathetic state, and a logical diagnostic and treatment strategy may target treatment of the sympathetic state, and later consideration of supplemental ventilator support. Certainly, the congestion that accompanies systolic and diastolic heart failure may be mediated in part by neurologic mechanisms. Removal of both the renal somatic afferent and sympathetic efferent conduction may address both the total body excess volume and the maldistribution of stored blood. Lastly, the functional renal component of cardiorenal syndrome, including diuretic resistance, may indeed be an immediate reflection of the functional efferent renal sympathetic activity, and a clinical trial to discern this physiology in humans is shortly to begin.
Conclusions
Afferent somatic signals arising from the kidney and efferent sympathetic activity to the kidney can mediate effects on wide range of chronic conditions. Interventional renal denervation has been shown to successfully reduce blood pressure and improve insulin resistance in patients with resistant hypertension. Further investigations are needed to study the effects of selective renal denervation in other entities linked by elevated sympathetic activity.
References
Esler M (2010) The 2009 Carl Ludwig Lecture: pathophysiology of the human sympathetic nervous system in cardiovascular diseases: the transition from mechanisms to medical management. J Appl Physiol 108:227–237
DiBona GF (2005) Physiology in perspective: the wisdom of the body. Neural control of the kidney. Am J Physiol Regul Integr Comp Physiol 289:R633–R641
Esler M, Lambert G, Jennings G (1989) Regional norepinephrine turnover in human hypertension. Clin Exp Hypertens A 11(Suppl 1):75–89
Huggett RJ, Scott EM, Gilbey SG, Stoker JB, Mackintosh AF, Mary DA (2003) Impact of type 2 diabetes mellitus on sympathetic neural mechanisms in hypertension. Circulation 108:3097–3101
DiBona GF, Sawin LL (1991) Role of renal nerves in sodium retention of cirrhosis and congestive heart failure. Am J Physiol 260:R298–R305
Mahfoud F, Böhm M (2010) Interventional renal sympathetic denervation—a new approach for patients with resistant hypertension. Dtsch Med Wochenschr 135:2422–2425
Vonend O, Marsalek P, Russ H, Wulkow R, Oberhauser V, Rump LC (2003) Moxonidine treatment of hypertensive patients with advanced renal failure. J Hypertension 21:1709–1717
Schlaich MP, Lambert E, Kaye DM, Krozowski Z, Campbell DJ, Lambert G, Hastings J, Aggarwal A, Esler MD (2004) Sympathetic augmentation in hypertension: role of nerve firing, norepinephrine reuptake, and angiotensin neuromodulation. Hypertension 43:169–175
Campese VM (1997) Neurogenic factors and hypertension in chronic renal failure. J Nephrol 10:184–187
Ye S, Zhong H, Yanamadala V, Campese VM (2002) Renal injury caused by intrarenal injection of phenol increases afferent and efferent renal sympathetic nerve activity. Am J Hypertens 15:717–724
Joles JA, Koomans HA (2004) Causes and consequences of increased sympathetic activity in renal disease. Hypertension 43:699–706
Hausberg M, Kosch M, Harmelink P, Barenbrock M, Hohage H, Kisters K, Dietl KH, Rahn KH (2002) Sympathetic nerve activity in end-stage renal disease. Circulation 106:1974–1979
Krum H, Sobotka P, Mahfoud F, Böhm M, Esler M, Schlaich M (2011) Device-based antihypertensive therapy: therapeutic modulation of the autonomic nervous system. Circulation 123:209–215
Schlaich MP, Sobotka PA, Krum H, Lambert E, Esler MD (2009) Renal sympathetic-nerve ablation for uncontrolled hypertension. N Engl J Med 361:932–934
Krum H, Schlaich M, Whitbourn R, Sobotka PA, Sadowski J, Bartus K, Kapelak B, Walton A, Sievert H, Thambar S, Abraham WT, Esler M (2009) Catheter-based renal sympathetic denervation for resistant hypertension: a multicentre safety and proof-of-principle cohort study. Lancet 373:1275–1281
Esler MD, Krum H, Sobotka PA, Schlaich MP, Schmieder RE, Böhm M (2010) Renal sympathetic denervation in patients with treatment-resistant hypertension (the symplicity htn-2 trial): a randomised controlled trial. Lancet 376:1903–1909
Doumas M, Douma S (2010) Renal sympathetic denervation: the jury is still out. Lancet 376:1878–1880
Fitzgerald PJ (2009) Is elevated noradrenaline an aetiological factor in a number of diseases? Auton Autacoid Pharmacol 29:143–156
Barajas L (1978) Innervation of the renal cortex. Fed Proc 37:1192–1201
Esler M (2000) The sympathetic system and hypertension. Am J Hypertens 13:99S–105S
Esler M, Jennings G, Biviano B, Lambert G, Hasking G (1986) Mechanism of elevated plasma noradrenaline in the course of essential hypertension. J Cardiovasc Pharmacol 8(Suppl 5):S39–S43
Esler M, Jennings G, Lambert G (1989) Noradrenaline release and the pathophysiology of primary human hypertension. Am J Hypertens 2:140S–146S
Hasking GJ, Esler MD, Jennings GL, Burton D, Johns JA, Korner PI (1986) Norepinephrine spillover to plasma in patients with congestive heart failure: evidence of increased overall and cardiorenal sympathetic nervous activity. Circulation 73:615–621
Ronco C, Haapio M, House AA, Anavekar N, Bellomo R (2008) Cardiorenal syndrome. J Am Coll Cardiol 52:1527–1539
Aggarwal A, Esler MD, Morris MJ, Lambert G, Kaye DM (2003) Regional sympathetic effects of low-dose clonidine in heart failure. Hypertension 41:553–557
Petersson M, Friberg P, Eisenhofer G, Lambert G, Rundqvist B (2005) Long-term outcome in relation to renal sympathetic activity in patients with chronic heart failure. Eur Heart J 26:906–913
Dickstein K (2008) Esc guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: application of natriuretic peptides. Reply. Eur Heart J 29:2388–2442
Gheorghiade M, Colucci WS, Swedberg K (2003) Beta-blockers in chronic heart failure. Circulation 107:1570–1575
Zoccali C, Mallamaci F, Parlongo S, Cutrupi S, Benedetto FA, Tripepi G, Bonanno G, Rapisarda F, Fatuzzo P, Seminara G, Cataliotti A, Stancanelli B, Malatino LS (2002) Plasma norepinephrine predicts survival and incident cardiovascular events in patients with end-stage renal disease. Circulation 105:1354–1359
Strojek K, Grzeszczak W, Gorska J, Leschinger MI, Ritz E (2001) Lowering of microalbuminuria in diabetic patients by a sympathicoplegic agent: novel approach to prevent progression of diabetic nephropathy? JASN 12:602–605
Hausberg M, Tokmak F, Pavenstadt H, Kramer BK, Rump LC (2010) Effects of moxonidine on sympathetic nerve activity in patients with end-stage renal disease. J Hypertension 28:1920–1927
Katholi RE (1985) Renal nerves and hypertension: an update. Fed Proc 44:2846–2850
O’Hagan KP, Thomas GD, Zambraski EJ (1990) Renal denervation decreases blood pressure in doca-treated miniature swine with established hypertension. Am J Hypertens 3:62–64
Kassab S, Kato T, Wilkins FC, Chen R, Hall JE, Granger JP (1995) Renal denervation attenuates the sodium retention and hypertension associated with obesity. Hypertension 25:893–897
Norman RA Jr, Murphy WR, Dzielak DJ, Khraibi AA, Carroll RG (1984) Role of the renal nerves in one-kidney, one clip hypertension in rats. Hypertension 6:622–626
Mancia G, Bousquet P, Elghozi JL, Esler M, Grassi G, Julius S, Reid J, Van Zwieten PA (2007) The sympathetic nervous system and the metabolic syndrome. J Hypertension 25:909–920
Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, White A, Cushman WC, White W, Sica D, Ferdinand K, Giles TD, Falkner B, Carey RM (2008) Resistant hypertension: diagnosis, evaluation, and treatment: a scientific statement from the American Heart Association professional education committee of the council for high blood pressure research. Circulation 117:e510–e526
Yumino D, Redolfi S, Ruttanaumpawan P, Su MC, Smith S, Newton GE, Mak S, Bradley TD (2010) Nocturnal rostral fluid shift: a unifying concept for the pathogenesis of obstructive and central sleep apnea in men with heart failure. Circulation 121:1598–1605
Witkowski A, Prejbisz A, Florczak E, Kadziela J, Sliwinski P, Bielen P, Michalowska I, Kabat M, Warchol E, Januszewicz M, Narkiewicz K, Somers V, Sobotka P, Januszewicz A (2011) Effects of renal sympathetic denervation on blood pressure in patients with resistant hypertension and sleep apnea—a preliminary report. TRenD Meeting 2011, Frankfurt, Germany
Grassi G, Facchini A, Trevano FQ, Dell’Oro R, Arenare F, Tana F, Bolla G, Monzani A, Robuschi M, Mancia G (2005) Obstructive sleep apnea-dependent and -independent adrenergic activation in obesity. Hypertension 46:321–325
Lima NK, Abbasi F, Lamendola C, Reaven GM (2009) Prevalence of insulin resistance and related risk factors for cardiovascular disease in patients with essential hypertension. Am J Hypertens 22:106–111
Julius S, Gudbrandsson T, Jamerson K, Tariq Shahab S, Andersson O (1991) The hemodynamic link between insulin resistance and hypertension. J Hypertension 9:983–986
Mahfoud F, Schlaich M, Kindermann I, Ukena C, Cremers B, Brandt MC, Hoppe UC, Vonend O, Rump LC, Sobotka PA, Krum H, Esler M, Bohm M (2011) Effect of renal sympathetic denervation on glucose metabolism in patients with resistant hypertension: a pilot study. Circulation 123:1940–1946
Schlaich MP, Straznicky N, Grima M, Ika-Sari C, Dawood T, Mahfoud F, Lambert E, Chopra R, Socratous F, Hennebry S, Eikelis N, Bohm M, Krum H, Lambert G, Esler MD, Sobotka PA (2011) Renal denervation: a potential new treatment modality for polycystic ovary syndrome? J Hypertension 29:991–996
Luippold G, Beilharz M, Muhlbauer B (2004) Chronic renal denervation prevents glomerular hyperfiltration in diabetic rats. Nephrol Dial Transplant 19:342–347
Cohn JN, Levine TB, Olivari MT, Garberg V, Lura D, Francis GS, Simon AB, Rector T (1984) Plasma norepinephrine as a guide to prognosis in patients with chronic congestive heart failure. N Engl J Med 311:819–823
Floras JS (2009) Sympathetic nervous system activation in human heart failure: clinical implications of an updated model. J Am Coll Cardiol 54:375–385
Packer M, Bristow MR, Cohn JN, Colucci WS, Fowler MB, Gilbert EM, Shusterman NH (1996) The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. U.S. Carvedilol heart failure study group. N Engl J Med 334:1349–1355
Francis GS, Benedict C, Johnstone DE, Kirlin PC, Nicklas J, Liang CS, Kubo SH, Rudin-Toretsky E, Yusuf S (1990) Comparison of neuroendocrine activation in patients with left ventricular dysfunction with and without congestive heart failure. A substudy of the studies of left ventricular dysfunction (solvd). Circulation 82:1724–1729
Jessup M, Costanzo MR (2009) The cardiorenal syndrome: do we need a change of strategy or a change of tactics? J Am Coll Cardiol 53:597–599
Schrier RW (1990) Body fluid volume regulation in health and disease: a unifying hypothesis. Ann Internal Med 113:155–159
Ring-Larsen H, Henriksen JH, Wilken C, Clausen J, Pals H, Christensen NJ (1986) Diuretic treatment in decompensated cirrhosis and congestive heart failure: effect of posture. Br Med J (Clin Res Ed) 292:1351–1353
Di Angelantonio E, Chowdhury R, Sarwar N, Ray KK, Gobin R, Saleheen D, Thompson A, Gudnason V, Sattar N, Danesh J (2009) B-type natriuretic peptides and cardiovascular risk: systematic review and meta-analysis of 40 prospective studies. Circulation 120:2177–2187
Villarreal D, Freeman RH, Johnson RA, Simmons JC (1994) Effects of renal denervation on postprandial sodium excretion in experimental heart failure. Am J Physiol 266:R1599–R1604
Nozawa T, Igawa A, Fujii N, Kato B, Yoshida N, Asanoi H, Inoue H (2002) Effects of long-term renal sympathetic denervation on heart failure after myocardial infarction in rats. Heart Vessels 16:51–56
Masaki H, Imaizumi T, Harasawa Y, Takeshita A (1994) Dynamic arterial baroreflex in rabbits with heart failure induced by rapid pacing. Am J Physiol 267:H92–H99
Clayton SC, Haack KK, Zucker IH (2011) Renal denervation modulates angiotensin receptor expression in the renal cortex of rabbits with chronic heart failure. Am J Physiol Renal Physiol 300:F31–F39
Steinback CD, Salzer D, Medeiros PJ, Kowalchuk J, Shoemaker JK (2009) Hypercapnic vs. Hypoxic control of cardiovascular, cardiovagal, and sympathetic function. Am J Physiol Regul Integr Comp Physiol 296:R402–R410
Chowdhury M, Adams S, Whellan DJ (2010) Sleep-disordered breathing and heart failure: focus on obstructive sleep apnea and treatment with continuous positive airway pressure. J Card Fail 16:164–174
Holzer-Richling N, Holzer M, Herkner H, Riedmuller E, Havel C, Kaff A, Malzer R, Schreiber W (2011) Randomized placebo controlled trial of furosemide on subjective perception of dyspnoea in patients with pulmonary oedema because of hypertensive crisis. Eur J Clin Invest 41:627–634
Hasselblad V, Gattis Stough W, Shah MR, Lokhnygina Y, O’Connor CM, Califf RM, Adams KF Jr (2007) Relation between dose of loop diuretics and outcomes in a heart failure population: results of the escape trial. Eur J Heart Fail 9:1064–1069
Smilde TD, Damman K, van der Harst P, Navis G, Westenbrink BD, Voors AA, Boomsma F, van Veldhuisen DJ, Hillege HL (2009) Differential associations between renal function and “modifiable” risk factors in patients with chronic heart failure. Clin Res Card 98:121–129
Ellison DH (2001) Diuretic therapy and resistance in congestive heart failure. Cardiology 96:132–143
Tomaselli GF, Zipes DP (2004) What causes sudden death in heart failure? Circ Res 95:754–763
Del Pace S, Parodi G, Bellandi B, Zampini L, Venditti F, Ardito M, Antoniucci D, Gensini GF (2011) Anxiety trait in patients with stress-induced cardiomyopathy: a case-control study. Clin Res Card 100:523–529
Swedberg K, Komajda M, Böhm M, Borer JS, Ford I, Dubost-Brama A, Lerebours G, Tavazzi L (2010) Ivabradine and outcomes in chronic heart failure (shift): a randomised placebo-controlled study. Lancet 376:875–885
Böhm M, Swedberg K, Komajda M, Borer JS, Ford I, Dubost-Brama A, Lerebours G, Tavazzi L (2010) Heart rate as a risk factor in chronic heart failure (shift): the association between heart rate and outcomes in a randomised placebo-controlled trial. Lancet 376:886–894
Moss AJ, Schwartz PJ, Crampton RS, Locati E, Carleen E (1985) The long qt syndrome: a prospective international study. Circulation 71:17–21
Heusser K, Tank J, Engeli S, Diedrich A, Menne J, Eckert S, Peters T, Sweep FC, Haller H, Pichlmaier AM, Luft FC, Jordan J (2010) Carotid baroreceptor stimulation, sympathetic activity, baroreflex function, and blood pressure in hypertensive patients. Hypertension 55:619–626
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Sobotka, P.A., Mahfoud, F., Schlaich, M.P. et al. Sympatho-renal axis in chronic disease. Clin Res Cardiol 100, 1049–1057 (2011). https://doi.org/10.1007/s00392-011-0335-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-011-0335-y