Abstract
Background
Osteoporotic hip fractures are a major cause of morbidity and mortality in postmenopausal women, and their impacts on society are substantial. Although adequate osteoporotic treatment reduces the risk of subsequent fractures and also mortality, only a minor proportion of the patients receives sufficient therapy.
Objectives
The goal of the present study was to evaluate osteoporosis treatment in two different cohorts and to describe the changes after the implementation of a Geriatric Facture Center (GFC) in cooperation with a level 1 trauma center.
Study design
A retrospective, single-center cross sectional study design was used.
Methods
A total of 455 patients (70 years and older) were included at our department of geriatric medicine. The patients were split into two groups. The usual care (UC) group consisted of 327 patients admitted to our department from 2001–2004. The GFC group included 128 patients admitted from 2009–2010. In addition to recording osteoporosis therapy, we collected demographic data, comorbidities, and different functional parameters of the patients. The data were collected retrospectively using medical records. SPSS 18.0 was used for statistical analysis.
Results
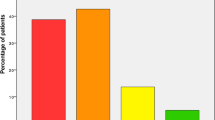
Of the patients, 43% in the GFC group received a specific antiresorptive or anabolic treatment (SAAT). Basic treatment with calcium and vitamin D3 was prescribed in 88% of the patients. The diagnosis “osteoporosis” was found in 73.4% of the discharge letters. In the UC group, the percentage of patients with a SAAT was 14.7%, calcium and vitamin D3 was prescribed in 30%, and the diagnosis was documented in 24.5%. All these differences are statistically significant (p < 0.0001). In the GFC group, better functional status and cognition were significantly associated with a higher rate of a prescribed SAAT, whereas age and comorbidities showed a negative association.
Conclusion
Our results show that the management of osteoporosis in postmenopausal hip fracture patients has significantly improved over the last decade. From our point of view, the main impact on this development is due to the implementation of a GFC with corresponding guidelines and treatment steps. In addition to structural changes, the improved evidence for osteoporosis treatment, especially of geriatric patients, has a positive influence on osteoporosis therapy.
Zusammenfassung
Hintergrund
Osteoporotische Frakturen stellen sowohl für die Betroffenen als auch für das Gesundheits- und Sozialsystem eine große Belastung dar. Bei älteren Frauen treten typischerweise hüftnahe Frakturen auf. Obwohl durch eine adäquate osteoporotische Therapie die Frakturrate und auch die Mortalität signifikant reduziert werden können, erhält nur eine Minderheit der Patientinnen die erforderliche Medikation.
Zielsetzung
Ziel der vorliegenden Studie war es, die Versorgung der Osteoporosetherapie in zwei Kohorten zu untersuchen sowie die Veränderungen nach Implementierung eines Geriatric Fracture Centers (GFC) an einem Traumazentrum darzustellen.
Studiendesign
Als Design wurde eine retrospektive Single-Center-Querschnittsuntersuchung benutzt.
Methode
Insgesamt konnten 455 Patientinnen (70 Jahre und älter) der Abteilung für Innere Medizin und Akutgeriatrie in die Studie eingeschlossen werden, die in zwei Gruppen aufgeteilt wurden. Patientinnen aus den Jahren 2001 bis 2004 wurden wie üblich behandelt und bildeten die Vergleichsgruppe (n=327). Die anderen 128 Patientinnen wurden 2009 bis 2011 interdisziplinär im Rahmen des GFC betreut. Neben der Osteoporosetherapie wurden Komorbiditäten sowie funktionelle Parameter als mögliche Einflussfaktoren miterfasst. Die Datenerhebung erfolgte retrospektiv anhand der Krankenakten. Die Auswertung erfolgte mittels SPSS 18.0.
Ergebnisse
In der Gruppe der GFC-Patienten erhielten 43% eine spezifische anitresorptive oder anabole Therapie. Die Basistherapie mit Kalzium und Vitamin D3 wurde in 88% der Fälle verordnet, die Diagnose „Osteoporose“ fand sich in 73,4% der Entlassungsbriefe. In der Vergleichsgruppe lag der Prozentsatz der Patienten mit einer spezifischen Therapie bei 14,7%, mit Kalzium und Vitamin D3 bei 30%, die Diagnose wurde in 24,5% angeführt. Alle Veränderungen sind hochsignifikant (p<0,0001). In der Gruppe der GFC-Patienten war ein besserer Funktionsstatus signifikant mit der Verordnung einer Basistherapie assoziiert; Alter, Komorbiditäten, kognitives Defizit waren signifikant negativ assoziiert; keinen Einfluss hatte die Polypharmazie.
Schlussfolgerung
Unsere Ergebnisse zeigen, dass es in den letzten 10 Jahren zu einer hochsignifikanten Verbesserung in der Versorgung der Patientinnen nach hüftnahen Frakturen gekommen ist. Einen wesentlichen Anteil an dieser Entwicklung dürfte die Etablierung eines GFC mit entsprechenden Leitlinien und Behandlungsschritten sein. Neben den strukturellen Änderungen hat sicher die verbesserte Evidenz für die Behandlung, insbesondere der geriatrischen Patienten, einen positiven Einfluss auf die Osteoporosetherapie.
Similar content being viewed by others
Reference
Parker M, Johannson A (2006) Hip fracture. BMJ 333:27–30
Zuckermann JD (1996) Hip fractures. N Engl J Med 334:1519–1525
Magaziner J, Simonsick EM, Kashner TM et al (1990) Predictors of functional recovery one year following hospital discharge for hip frature: a prospective study. J Gerontol 45:M101–M107
Center JR, Bliuc D, Nguyen TV et al (2007) Risk of subsequent fracture after low-trauma fracture in men and women. JAMA 297:387–394
Bliuc D, Nguyen ND, Milch VE et al (2009) Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and woman. JAMA 301(5):513–521
Clinician’s Guide to Prevention and Treatment of Osteoporosis (2009) National Osteoporosis Foundation [on-line]. Available at http://www.nof.org/professionals/NOF_Clinicians_Guide.pdf. Accessed 01 November 2011
NIH Consensus Development Panel on Osteoporosis Prevention, Diagnosis and Therapy (2001) Osteoporosis prevention, diagnosis and therapy. JAMA 285:785–795
Lyles KW, Colon-Emeric CS, Magaziner JS et al (2007) Zoledronic acid in reducing clinical fracture and mortality after hip fracture. N Engl J Med 357:1799–1809
MacLean C, Newberry S, Maglione M et al (2008) Systematic review: comparative effectiveness of treatments to prevent fractures in men and women with low bone density or osteoporosis. Ann Intern Med 148:197–213
Morin S, Rahme E, Behlouli H et al (2007) Effectiveness of antiresorptive agents in the prevention of recurrent hip fractures. Osteoporos Int 18:1625–1632
Kammerlander C, Gosch M, Kammerlander-Knauer U et al (2011) Long-term functional outcome in geriatric patients hip fracture patients. Arch Orthop Trauma Surg. doi 10.1007/s00402-011-1313-6
Jennings LA, Auerbach AD, Maselli J et al (2010) Missed opportunities for osteoporosis treatment in patients hospitalized for hip fracture. J Am Geriatr Soc 58:650–657
Leyles KW, Colon-Emerie CS, Magaziner JS et al (2007) Zoledronic acid in reducing clinical fracture and mortality after hip fracture. N Engl J Med 357:1799–1809
Black DM, Delmas PD, Eastell R et al (2007) Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med 356:1809–1833
Bolland MJ, Grey AB, Gamble GD et al (2010) Effect of osteoporosis treatment on mortality: a meta analysis. J Clin Endocrinol Metab 95:1174–1181
Bogoch ER, Elliot-Gibson V, Beaton DE et al (2006) Effective initiation of osteoporosis diagnosis and treatment for patients with a fragility fracture in an orthopedic environment. J Bone Joint Surg Am 88(1):25–34
Friedman SM, Mendelson DA, Bingham KW et al (2009) Impact of a comanaged geriatric fracture center on short-term hip fracture outcomes. Arch Intern Med 169(18):1712–1717
Shyu YI, Liang J, Wu CC et al (2010) Two-year effects of interdisciplinary intervention for hip fracture in older Taiwanese. J Am Geriatr Soc 58:1081–1089
Henry MJ, Pasco JA, Nicholson GC et al (2000) Prevalence of osteoporosis in Australian women: Geelong osteoporosis study. J Clin Densitom 3:261–268
Chiang A, Jones J, Humphreys J et al (2006) Osteoporosis, diagnosis and treatment in a general practice population. Aust Fam Physician 35(3):166–168
Häussler B, Gothe H, Göl D et al (2007) Epidemiology, treatment and costs of osteoporosis in Germany – the BoneEVA Study. Osteoporos Int 18(1):77–84
McLellan AR, Wolowacz SE, Zimovetz EA et al (2011) Fracture liaison services for the evaluation and management of patients with osteoporotic fracture: a cost effectiveness evaluation based on data collected over 8 years of service provision. Osteoporos Int 22:2083–2098
Handoll HH, Cammeron ID, Mak JC et al (2009) Multidisciplinary rehabilitation for older patients with hip fractures. Cochrane Database Syst Rev 7(4):CD007125
Inderjeeth CA, Foo ACH, Lai MMY et al (2009) Efficacy and safety of pharmacological agents in managing osteoporosis in the old old: review of the literature. Bone 44:744–751
Boonen ST, Black DM, Clon-Emeric CS et al (2010) Efficacy and safety of a once-yearly intravenous zoledronic acid 5 mg for fracture prevention in elderly postmenopausal women with osteoporosis aged over 75 and older. J Am Geriatr Soc 58:292–299
Boonen ST, Black DM, Clon-Emeric CS et al (2006) Safety and efficacy of teriparatide in elderly women with established osteoporosis: bone anabolic therapy from a geriatric perspective. J Am Geriatr Soc 54:782–789
Meunier PJ, Roux C, Seeman E et al (2004) The effects of strontium ranelate on the risk of vertebral fracture in women with postmenopausal osteoporosis. SOTI study. N Engl J Med 350(5):459–468
Cummings SR, San Martin J, McClung MR et al (2009) Denosumab for prevention of fractures in postmenopaual women with osteoporosis. N Engl J Med 361(8):756–765
Gates BJ, Sonnett TE, Duvall CA et al (2009) Review of osteoporosis pharmacotherapy for geriatric patients. Am J Geriatr Pharmacother 7:293–323
Schousboe JT, Ensrud KE, Nyman JA et al (2005) Universal bone densitometry screening combined with alendronate therapy for those diagnosed with osteoporosis is highly cost-effective for eldery women. J Am Geriatr Soc 53(10):1697–1704
Conflict of interest
The corresponding author states that there are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gosch, M., Roth, T., Kammerlander, C. et al. Treatment of osteoporosis in postmenopausal hip fracture patients after geriatric rehabilitation. Z Gerontol Geriat 44, 381–386 (2011). https://doi.org/10.1007/s00391-011-0254-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00391-011-0254-6