Abstract
Background
The aging population is growing rapidly and this change results in an increase in the number of fragility fracture patients. Several reports describe their poor outcome. Integrated models of care have been published in order to improve quality of patient care. We established an orthogeriatric model of care at the Department of Trauma Surgery in Innsbruck in cooperation with the Department of Geriatric Medicine (Hochzirl) and the Department for Anesthesiology. This report describes our concept as well as initial experience.
Patients and methods
We included all geriatric patients according to the definition of the German Geriatric Society. In all patients, basic demographic data, Charlson Comorbidity Index, and type of fracture were recorded. Main principles of the newly implemented system are the integration of a geriatrician in our team of trauma surgeons and anesthesiologists, prioritization of patients, development of our own clinical treatment guidelines, regular interdisciplinary and interprofessional meetings, a special outpatient clinic for these patients, and the better cooperation with the nearby Department of Geriatric Medicine.
Results
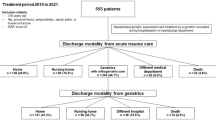
A total of 529 patients met our inclusion criteria during 2010; 77.4% were female and the mean age was 84.1 years. The overall medical complication rate was 20.4%. Of the patients, 36.1% had hip fractures and 70.5% could be operated mainly using spinal anesthesia within 24 h and their mean length of stay was significantly shorter than operations performed 5 years previously. At 3 months, 86.7% of the patients had returned home and, thus, had reached their prefracture residency.
Conclusion
A coordinated, multidisciplinary model for the treatment of fragility fractures has the potential to improve the quality of patient care. Several international studies report superior outcome and our own findings are promising as well. We could show that our major goals, e.g., reduction of complications, shortening the length of stay, and restoration of the prefracture residency, can be improved by implementing such a model.
Zusammenfassung
Hintergrund
Der demographische Wandel mit zunehmender Überalterung der Bevölkerung führt auch zu einer deutlichen Zunahme an Patienten mit Fragilitätsfrakturen. Einige Studien zeigten das schlechte Outcome nach solchen Frakturen. In den letzten Jahren haben daher Modelle zur interdisziplinären Primärbehandlung dieser Patienten zugenommen und auch bereits deutliche Verbesserungen im Outcome dieser Patienten erbracht. An der Universitätsklinik für Unfallchirurgie wurde im April 2009 ein „Tiroler Zentrum für Altersfrakturen“ in Zusammenarbeit mit der Akutgeriatrie des Krankenhauses in Hochzirl und der Universitätsklinik für Anästhesie gegründet. Diese Arbeit stellt unser Konzept und erste Ergebnisse vor.
Patienten und Methoden
Alle geriatrische Patienten mit einer Fraktur wurden eingeschlossen. Neben demographischen Daten wurden auch die Nebenerkrankungen und Daten zur Fraktur erhoben. Die Grundprinzipien sind die Integration eines Geriaters in unser unfallchirurgisches Team, die Priorisierung der geriatrischen Patienten, die Entwicklung eigener Guidelines, regelmässige Meetings, eine spezielle Altersfrakturambulanz und ein besseres Nahtstellenmanagement.
Ergebnisse
In die Studie wurden alle geriatrische Patienten mit einer Fraktur eingeschlossen. Neben demographischen Daten wurden auch die Nebenerkrankungen und Daten zur Fraktur erhoben. Die Grundprinzipien des Modells sind die Integration eines Geriaters in unser unfallchirurgisches Team, die Priorisierung der geriatrischen Patienten, die Entwicklung eigener Guidelines, regelmäßige Meetings, eine spezielle Altersfrakturambulanz und ein besseres Nahtstellenmanagement.
Schlussfolgerung
Ein koordiniertes, multidisziplinäres Modell zur Behandlung von Patienten mit Fragilitätsfrakturen verbessert deren Behandlungsqualität. Zahlreiche internationale Studien und eigene Daten belegen dies. Die Hauptvorteile sind eine signifikante Reduktion von internistischen Komplikationen und stationärer Aufenthaltsdauer sowie die bessere Wiederherstellung der Funktion, sodass ein großer Teil der Patienten wieder nach Hause entlassen werden kann.



Similar content being viewed by others
References
Statistik Austria (2011) http://www.statistik.at/web_de/statistiken/bevoelkerung/bevoelkerungsstruktur/bevoelkerung_nach_alter_geschlecht/index.html (accessed 09 October 2011)
Berger E (2008) The graying of America: the impact of aging baby boomers on emergency departments. Ann Emerg Med 51:288–290
BOA (2007) BOA-BGS Blue Book – The care of fragility fracture patients. p 74
Charlson M, Szatrowski TP, Peterson J et al (1994) Validation of a combined comorbidity index. J Clin Epidemiol 47:1245–1251
Clement ND, Aitken SA, Duckworth AD et al (2011) The outcome of fractures in very elderly patients. J Bone Joint Surg Br 93:806–810
Cogan L, Martin AJ, Kelly LA et al (2010) An audit of hip fracture services in the Mater Hospital Dublin 2001 compared with 2006. Ir J Med Sci 179:51–55
Friedman SM, Mendelson DA, Bingham KW et al (2009) Impact of a comanaged Geriatric Fracture Center on short-term hip fracture outcomes. Arch Intern Med 169:1712–1717
Friedman SM, Mendelson DA, Kates SL et al (2008) Geriatric co-management of proximal femur fractures: total quality management and protocol-driven care result in better outcomes for a frail patient population. J Am Geriatr Soc 56:1349–1356
Gosch M, Kammerlander C, Roth T et al (2011) Tiroler Zentrum für Altersfrakturen – Traumatologisch-geriatrisches Co-Management: Erste Erfahrungen und Ergebnisse. J Mineralstoffwechsel 18:7–12
Kammerlander C, Gosch M, Kammerlander-Knauer U et al (2011) Long-term functional outcome in geriatric hip fracture patients. Arch Orthop Trauma Surg 131:1435–1444
Kammerlander C, Roth T, Friedman SM et al (2010) Ortho-geriatric service – a literature review comparing different models. Osteoporos Int 21:637–646
Kanis JA, Johnell O (2005) Requirements for DXA for the management of osteoporosis in Europe. Osteoporosis international: a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA 16:229–238
Naglie G, Tansey C, Kirkland JL et al (2002) Interdisciplinary inpatient care for elderly people with hip fracture: a randomized controlled trial. Can Medl Assoc J 167:25–32
Pioli G, Giusti A, Barone A (2008) Orthogeriatric care for the elderly with hip fractures: where are we? Aging Clin Exp Res 20:113–122
Radcliff TA, Henderson WG, Stoner TJ et al (2008) Patient risk factors, operative care, and outcomes among older community-dwelling male veterans with hip fracture. J Bone Joint Surg Am 90:34–42
Rieder (2007) Austrian Report on Osteoporosis
Roche JJ, Wenn RT, Sahota O et al (2005) Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ 331:1374
Roth T, Kammerlander C, Gosch M et al (2010) Outcome in geriatric fracture patients and how it can be improved. Osteoporos Int 21:615–619
Todd CJ, Freeman CJ, Camilleri-Ferrante C et al (1995) Differences in mortality after fracture of hip: the east Anglian audit. BMJ 310:904–908
Vidán M, Serra JA, Moreno C et al (2005) Efficacy of a comprehensive geriatric intervention in older patients hospitalized for hip fracture: a randomized, controlled trial. J Am Geriatr Soc 53:1476–1482
Conflict of interest
The corresponding author states that there are no conflicts of interest.
Funding
The Tyrolean Geriatric Fracture Center receives funding from the Tyrolean Government through the “Tiroler Gesundheitsförderungsfonds.”
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kammerlander, C., Gosch, M., Blauth, M. et al. The Tyrolean Geriatric Fracture Center. Z Gerontol Geriat 44, 363–367 (2011). https://doi.org/10.1007/s00391-011-0253-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00391-011-0253-7
Keywords
- Hip fracture
- Interdisciplinary healthcare team
- Treatment outcome
- Independent living
- Inhospital mortality