Abstract
Purpose
The study aims to systematically evaluate the clinical efficacy after 8 weeks (long interval, LI) between neoadjuvant chemoradiotherapy and surgery for locally advanced rectal cancer.
Methods
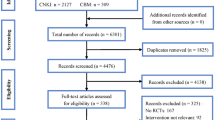
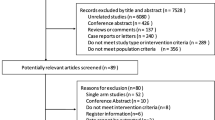
The PubMed database, EMBASE database, and the Cochrane Library (deadline: September 25, 2021) were searched to select clinical studies that compared two intervals between neoadjuvant chemoradiotherapy and surgery for locally advanced rectal cancer: after 8 weeks (long interval, LI) and within 8 weeks (short interval, SI). The included studies were screened and evaluated according to the inclusion and exclusion criteria, and meta-analysis was performed by RevMan 5.3 software.
Results
Eighteen studies were included, with 9070 cases in the LI group and 14,207 cases in the SI group. The analysis results showed that the pathologic complete response (PCR) rate in the LI group was higher than that in the SI group (P < 0.00001). There was no significant difference in the R0 resection rate (P = 0.85), anal preservation rate (P = 0.89), morbidity rate (P = 0.60), anastomotic leakage rate (P = 0.06), operation time (P = 0.58), local recurrence rate (P = 0.56), distant metastasis rate (P = 0.32), or overall survival (OS) rate (P = 0.17) between the two groups.
Conclusion
A longer interval between neoadjuvant chemoradiotherapy and surgery can improve the PCR rate; however, it has no significant impact on the clinical efficacy or long-term prognosis. Due to some limitations in the number and quality of the studies, these findings still need to be further verified by multicenter, large-sample high-quality RCTs in the future.














Similar content being viewed by others
References
Martling AL, Holm T, Rutqvist LE, Moran BJ, Heald RJ, Cedemark B (2000) Effect of a surgical training programme on outcome of rectal cancer in the County of Stockholm. Stockholm colorectal cancer study group, basingstoke bowel cancer research project. Lancet 356:93–96. https://doi.org/10.1016/s0140-6736(00)02469-7
Marr R, Birbeck K, Garvican J et al (2005) The modern abdominoperineal excision: the next challenge after total mesorectal excision. Ann Surg 242:74–82. https://doi.org/10.1097/01.sla.0000167926.60908.15
Benson AB, Venook AP, Al-Hawary MM et al (2018) Rectal cancer, version 2.2018, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw 16:874–901. https://doi.org/10.6004/jnccn.2018.0061
Glynne-Jones R, Wyrwicz L, Tiret E, Brown G, Rödel C, Cervantes A, Arnold D (2017) Rectal cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 28:iv22–iv40. https://doi.org/10.1093/annonc/mdx224
Turner MC, Keenan JE, Rushing CN, Gulack BC, Nussbaum DP, Benrashid E, Hyslop T, Strickler JH, Mantyh CR, Migaly J (2019) Adjuvant chemotherapy improves survival following resection of locally advanced rectal cancer with pathologic complete response. J Gastrointest Surg 23:1614–1622. https://doi.org/10.1007/s11605-018-04079-8
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17:1–12. https://doi.org/10.1016/0197-2456(95)00134-4
Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savović J, Schulz KF, Weeks L, Sterne JAC (2011) The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:D5928. https://doi.org/10.1136/bmj.d5928
Stang A (2010) Critical evaluation of the Newcastle-Ottawa Scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25:603–605. https://doi.org/10.1007/s10654-010-9491-z
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I et al (2016) ROBINS-I: a tool for assessing risk of bias in nonrandomised studies of interventions. BMJ (Clin Res Ed) 355:i4. https://doi.org/10.1136/bmj.i4919
Akbar A, Bhatti AB, Niazi SK, Syed AA, Khattak S, Raza SH, Kazmi AS (2016) Impact of time interval between chemoradiation and surgery on pathological complete response and survival in rectal cancer. Asian Pac J Cancer Prev 17:89–93. https://doi.org/10.7314/apjcp.2016.17.1.89
Akgun E, Caliskan C, Bozbiyik O, Yoldas T, Sezak M, Ozkok S, Kose T, Karabulut B, Harman M, Ozutemiz O (2018) Randomized clinical trial of short or long interval between neoadjuvant chemoradiotherapy and surgery for rectal cancer. Br J Surg 105:1417–1425. https://doi.org/10.1002/bjs.10984
Evans J, Tait D, Swift I, Pennert K, Tekkis P, Wotherspoon A, Chau I, Cunningham D, Brown G (2011) Timing of surgery following preoperative therapy in rectal cancer: the need for a prospective randomized trial?. Dis Colon Rectum 54:1251–1259. https://doi.org/10.1097/DCR.0b013e3182281f4b
Foster JD, Ewings P, Falk S, Cooper EJ, Roach H, West NP, Williams-Yesson BA, Hanna GB, Francis NK (2016) Surgical timing after chemoradiotherapy for rectal cancer, analysis of technique (STARRCAT): results of a feasibility multi-centre randomized controlled trial. Tech Coloproctol 20:683–693. https://doi.org/10.1007/s10151-016-1514-7
Garcia-Aguilar J, Smith DD, Avila K, Bergsland EK, Chu P, Krieg RM (2011) Optimal timing of surgery after chemoradiation for advanced rectal cancer: preliminary results of a multicenter, nonrandomized phase II prospective trial. Ann Surg 254:97–102. https://doi.org/10.1097/SLA.0b013e3182196e1f
Garrer WY, El Hossieny HA, Gad ZS, Namour AE, Abo Amer SM (2016) Appropriate timing of surgery after neoadjuvant chemoradiation therapy for locally advanced rectal cancer. Asian Pac J Cancer Prev 17:4381–4389
Kim MJ, Cho JS, Kim EM, Ko WA, Oh JH (2018) Optimal time interval for surgery after neoadjuvant chemoradiotherapy in patients with locally advanced rectal cancer: analysis of health insurance review and assessment service data. Ann Coloproctol 34:241–247. https://doi.org/10.3393/ac.2018.01.01
Kuan FC, Lai CH, Ku HY, Wu CF, Hsieh MC, Liu TW, Yeh CY, Lee KD (2017) The survival impact of delayed surgery and adjuvant chemotherapy on stage II/III rectal cancer with pathological complete response after neoadjuvant chemoradiation. Int J Cancer 140:1662–1669. https://doi.org/10.1002/ijc.30562
Lee SW, Lee JH, Lee IK et al (2018) The impact of surgical timing on pathologic tumor response after short course and long course preoperative chemoradiation for locally advanced rectal adenocarcinoma. Cancer Res Treat 50:1039–1050. https://doi.org/10.4143/crt.2017.252
Lefevre JH, Mineur L, Kotti S et al (2016) Effect of Interval (7 or 11 weeks) between neoadjuvant radiochemotherapy and surgery on complete pathologic response in rectal cancer: a multicenter, randomized, controlled trial (GRECCAR-6). J Clin Oncol 34:3773–3780. https://doi.org/10.1200/jco.2016.67.6049
Lichthardt S, Wagner J, Löb S et al (2020) Pathological complete response due to a prolonged time interval between preoperative chemoradiation and surgery in locally advanced rectal cancer: analysis from the German StuDoQ| Rectalcarcinoma registry. BMC Cancer 20(1):1–8
Nguyen P, Wuthrick E, Chablani P et al (2018) Does delaying surgical resection after neoadjuvant chemoradiation impact clinical outcomes in locally advanced rectal adenocarcinoma?. A single-institution experience. Am J Clin Oncol 41:140–146. https://doi.org/10.1097/coc.0000000000000248
Probst CP, Becerra AZ, Aquina CT, Tejani MA, Wexner SD, Garcia-Aguilar J, Remzi FH, Dietz DW, Monson JR, Fleming FJ (2015) Extended Intervals after neoadjuvant therapy in locally advanced rectal cancer: the key to improved tumor response and potential organ preservation. J Am Coll Surg 221:430–440. https://doi.org/10.1016/j.jamcollsurg.2015.04.010
Rombouts AJM, Hugen N, Elferink MAG, Nagtegaal ID, de Wilt JHW (2016) Treatment interval between neoadjuvant chemoradiotherapy and surgery in rectal cancer patients: a population-based study. Ann Surg Oncol 23:3593–3601. https://doi.org/10.1245/s10434-016-5294-0
Stein DE, Mahmoud NN, Anné PR, Rose DG, Isenberg GA, Goldstein SD, Mitchell E, Fry RD (2003) Longer time interval between completion of neoadjuvant chemoradiation and surgical resection does not improve downstaging of rectal carcinoma. Dis Colon Rectum 46:448–453. https://doi.org/10.1007/s10350-004-6579-0
Terzi C, Bingul M, Arslan NC et al (2020) Randomized controlled trial of 8 weeks’ vs 12 weeks’ interval between neoadjuvant chemoradiotherapy and surgery for locally advanced rectal cancer. Colorectal Dis 22:279–288. https://doi.org/10.1111/codi.14867
Timudom K, Phothong N, Akaraviputh T, Chinswangwatanakul V, Pongpaibul A, Petsuksiri J, Ithimakin S, Trakarnsanga A (2016) Does extending the waiting time of low-rectal cancer surgery after neoadjuvant chemoradiation increase the perioperative complications? Gastroenterol Res Pract 2016:7870815. https://doi.org/10.1155/2016/7870815
Tran CL, Udani S, Holt A, Arnell T, Kumar R, Stamos MJ (2006) Evaluation of safety of increased time interval between chemoradiation and resection for rectal cancer. Am J Surg 192:873–877. https://doi.org/10.1016/j.amjsurg.2006.08.061
Habr-Gama A, Perez RO, Proscurshim I, Nunes Dos Santos RM, Kiss D, Gama-Rodrigues J, Cecconello I (2008) Interval between surgery and neoadjuvant chemoradiation therapy for distal rectal cancer: does delayed surgery have an impact on outcome?. Int J Radiat Oncol Biol Phys 71:1181–1188. https://doi.org/10.1016/j.ijrobp.2007.11.035
Huntington CR, Boselli D, Symanowski J, Hill JS, Crimaldi A, Salo JC (2016) Optimal timing of surgical resection after radiation in locally advanced rectal adenocarcinoma: an analysis of the national cancer database. Ann Surg Oncol 23:877–887. https://doi.org/10.1245/s10434-015-4927-z
Garcia-Aguilar J, Chow OS, Smith DD et al (2015) Effect of adding mFOLFOX6 after neoadjuvant chemoradiation in locally advanced rectal cancer: a multicentre, phase 2 trial. Lancet Oncol 16(8):957–966
Du D, Su Z, Wang D et al (2018) Optimal interval to surgery after neoadjuvant chemoradiotherapy in rectal cancer: a systematic review and meta-analysis. Clin Colorectal Cancer 17(1):13–24
Foster JD, Jones EL, Falk S et al (2013) Timing of surgery after long-course neoadjuvant chemoradiotherapy for rectal cancer: a systematic review of the literature. Dis Colon Rectum 56(7):921–930
Petrelli F, Sgroi G, Sarti E et al (2016) Increasing the interval between neoadjuvant chemoradiotherapy and surgery in rectal cancer [J]. Ann Surg 263(3):458–464
Ryan ÉJ, O’Sullivan DP, Kelly ME et al (2019) Meta-analysis of the effect of extending the interval after long-course chemoradiotherapy before surgery in locally advanced rectal cancer. Journal of British Surgery 106(10):1298–1310
Polanco PM, Mokdad AA, Zhu H et al (2018) Association of adjuvant chemotherapy with overall survival in patients with rectal cancer and pathologic complete response following neoadjuvant chemotherapy and resection. JAMA Oncol 4(7):938–943
Dossa F, Acuna SA, Rickles AS et al (2018) Association between adjuvant chemotherapy and overall survival in patients with rectal cancer and pathological complete response after neoadjuvant chemotherapy and resection. JAMA Oncol 4(7):930–937
Mills CC, Kolb EA, Sampson VB (2018) Development of chemotherapy with cell-cycle inhibitors for adult and pediatric cancer therapy. Can Res 78(2):320–325
Habr-Gama A, São Julião GP, Fernandez LM et al (2019) Achieving a complete clinical response after neoadjuvant chemoradiation that does not require surgical resection: it may take longer than you think!. Dis Colon Rectum 62(7):802–808
Figueiredo N, Panteleimonitis S, Popeskou S et al (2018) Delaying surgery after neoadjuvant chemoradiotherapy in rectal cancer has no influence in surgical approach or short-term clinical outcomes. Eur J Surg Oncol 44(4):484–489
Wang X, Zheng Z, Zhu H et al (2021) Timing to achieve the best recurrence-free survival after neoadjuvant chemoradiotherapy in locally advanced rectal cancer: experience in a large-volume center in China. Int J Colorectal Dis 36(5):1007–1016
Hu MH, Huang RK, Zhao RS, Yang KL, Wang H (2017) Does neoadjuvant therapy increase the incidence of anastomotic leakage after anterior resection for mid and low rectal cancer?. A systematic review and meta-analysis. Colorectal Dis 19(1):16–26
Fan WH, Xiao J, An X et al (2017) Patterns of recurrence in patients achieving pathologic complete response after neoadjuvant chemoradiotherapy for rectal cancer. J Cancer Res Clin Oncol 143(8):1461–1467
Liu Q, Zhang H, Jiang X et al (2017) Factors involved in cancer metastasis: a better understanding to “seed and soil” hypothesis. Mol Cancer 16(1):1–19
Petrelli F, Trevisan F, Cabiddu M et al (2020) Total neoadjuvant therapy in rectal cancer: a systematic review and meta-analysis of treatment outcomes. Ann Surg 271(3):440–448
Funding
This work was supported by the scientific research project of Sichuan Vocational College of Health and Rehabilitation (CWKY-2020Y-04).
Author information
Authors and Affiliations
Contributions
Miao Yu and Deng-Chao Wang designed the study. Sheng Li ran the search strategy. Li-Yan Huang collected the data. Deng-Chao Wang and Miao Yu re-checked the data. Sheng Li and Li-Yan Huang performed the analyses, and Deng-Chao Wang checked the analyses. Jian Wei and Sheng Li assessed the quality of the studies, and Deng-Chao Wang confirmed the quality. Miao Yu wrote the manuscript, and Deng-Chao Wang edited the manuscript. All listed authors reviewed and revised the manuscript.
Corresponding author
Ethics declarations
Ethics approval
For this type of study, formal consent was not required.
Consent to participate
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yu, M., Wang, DC., Li, S. et al. Does a long interval between neoadjuvant chemoradiotherapy and surgery benefit the clinical outcomes of locally advanced rectal cancer? A systematic review and meta analyses. Int J Colorectal Dis 37, 855–868 (2022). https://doi.org/10.1007/s00384-022-04122-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-022-04122-w