Abstract
Aim
Up to 80% of patients after low anterior resection, experience (low) anterior resection syndrome (ARS/LARS). However, there is no standard treatment option currently available. This systemic review aims to summarize treatment possibilities for LARS after surgical treatment of rectal cancer in the medical literature.
Methods
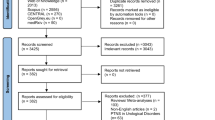
Embase, PubMed, and the Cochrane Library were searched using the terms anterior resection syndrome, low anterior resection, colorectal/rectal/rectum, surgery/operation, pelvic floor rehabilitation, biofeedback, transanal irrigation, sacral nerve stimulation, and tibial nerve stimulation. All English language articles presenting original patient data regarding treatment and outcome of LARS were included. We focused on the effects of different treatment modalities for LARS. The Jadad score was used to assess the methodological quality of trials. The quality scale ranges from 0 to 5 points, with a score ≤ 2 indicating a low quality report, and a score of ≥ 3 indicating a high quality report.
Results
Twenty-one of 160 studies met the inclusion criteria, of which 8 were reporting sacral nerve stimulation, 6 were designed to determine pelvic floor rehabilitation, 3 studies evaluated the effect of transanal irrigation, 2—percutaneous tibial nerve stimulation, and the rest of the studies assessed probiotics and 5-HT3 receptor antagonists for LARS in patients who had undergone rectal resection. All except one study were poor quality reports according to the Jadad score.
Conclusions
LARS treatment still carries difficulties because of a lack of well-conducted, randomized multicenter trials. Well-performed randomized controlled trials are needed.


Similar content being viewed by others
References
Ziv Y, Zbar A, Bar-Shavit Y, Igov I (2013) Low anterior resection syndrome (LARS): cause and effect and reconstructive considerations. Tech Coloproctol 17(2):151–162. https://doi.org/10.1007/s10151-012-0909-3
Camilleri-Brennan J, Steele RJ (1998) Quality of life after treatment for rectal cancer. Br J Surg 85(8):1036–1043. https://doi.org/10.1046/j.1365-2168.1998.00808.x
Bryant CL, Lunniss PJ, Knowles CH, Thaha MA, Chan CL (2012) Anterior resection syndrome. Lancet Oncol 13:403–408
Keane C, Wells C, O'Grady G, Bissett IP (2017) Defining low anterior resection syndrome: a systematic review of the literature. Colorectal Dis doi: https://doi.org/10.1111/codi.13767. [Epub ahead of print], 19, 8, 713, 722
Liu CH, Chen CH, Lee JC (2011) Rehabilitation exercise on the quality of life in anal sphincter-preserving surgery. Hepato-Gastroenterology 58(110-111):1461–1465. https://doi.org/10.5754/hge11160
Emmertsen KJ, Laurberg S (2012) Low anterior resection syndrome score: development and validation of a symptom-based scoring system for bowel dysfunction after low anterior resection for rectal cancer. Ann Surg 255(5):922–928. https://doi.org/10.1097/SLA.0b013e31824f1c21
Chen TY, Emmertsen KJ, Laurberg S (2015) What are the best questionnaires to capture anorectal function after surgery in rectal cancer? Curr Colorectal Cancer Rep 11(1):37–43. https://doi.org/10.1007/s11888-014-0217-6
Pucciani F (2013) A review on functional results of sphincter-saving surgery for rectal cancer: the anterior resection syndrome. Updat Surg 65(4):257–263. https://doi.org/10.1007/s13304-013-0220-5
Liu F, Guo P, Shen Z, Gao Z, Wang S, Ye Y (2017) Risk factor analysis of low anterior resection syndrome after anal sphincter preserving surgery for rectal carcinoma. Zhonghua Wei Chang Wai Ke Za Zhi 20(3):289–294
Lee WY, Takahashi T, Pappas T, Mantyh CR, Ludwig KA (2008) Surgical autonomic denervation results in altered colonic motility: an explanation for low anterior resection syndrome? Surgery 143(6):778–783. https://doi.org/10.1016/j.surg.2008.03.014
Farouk R, Duthie GS, Lee PW, Monson JR (1998) Endosonographic evidence of injury to the internal anal sphincter after low anterior resection: long-term follow-up. Dis Colon rectum 41(7):888–891. https://doi.org/10.1007/BF02235373
Bakx R, Doeksen A, Slors JF, Bemelman WA, van Lanschot JJ, Boeckxstaens GE (2009) Neorectal irritability after short-term preoperative radiotherapy and surgical resection for rectal cancer. Am J Gastroenterol 104(1):133–141. https://doi.org/10.1038/ajg.2008.2
Dulskas A, Miliauskas P, Tikuisis R, Escalante R, Samalavicius NE (2016) The functional results of radical rectal cancer surgery: review of the literature. Acta Chir Belg 116(1):1–10. https://doi.org/10.1080/00015458.2015.1136482
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 62(10):1006–1012. https://doi.org/10.1016/j.jclinepi.2009.06.005
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17(1):1–12. https://doi.org/10.1016/0197-2456(95)00134-4
Bols E, Berghmans B, de Bie R, Govaert B, van Wunnik B, Heymans M, Hendriks E, Baeten C (2012) Rectal balloon training as add-on therapy to pelvic floor muscle training in adults with fecal incontinence: a randomized controlled trial. Neurourol Urodyn 31(1):132–138. https://doi.org/10.1002/nau.21218
Visser WS, te Riele WW, Boerma D, van Ramshorst B, van Westreenen HL (2014) Pelvic floor rehabilitation to improve functional outcome after a low anterior resection: a systematic review. Ann Coloproctol 30(3):109–114. https://doi.org/10.3393/ac.2014.30.3.109
Allgayer H, Dietrich CF, Rohde W, Koch GF, Tuschhoff T (2005) Prospective comparison of short- and long-term effects of pelvic floor exercise/biofeedback training in patients with fecal incontinence after surgery plus irradiation versus surgery alone for colorectal cancer: clinical, functional and endoscopic/endosonographic findings. Scand J Gastroenterol 40(10):1168–1175. https://doi.org/10.1080/00365520510023477
Kim KH, CS Y, Yoon YS, Yoon SN, Lim SB, Kim JC (2011) Effectiveness of biofeedback therapy in the treatment of anterior resection syndrome after rectal cancer surgery. Dis Colon rectum 54(9):1107–1113. https://doi.org/10.1097/DCR.0b013e318221a934
Pucciani F, Ringressi MN, Redditi S, Masi A, Giani I (2008) Rehabilitation of fecal incontinence after sphincter-saving surgery for rectal cancer: encouraging results. Dis Colon rectum 51(10):1552–1558. https://doi.org/10.1007/s10350-008-9312-6
Laforest A, Bretagnol F, Mouazan AS, Maggiori L, Ferron M, Panis Y (2012) Functional disorders after rectal cancer resection: does a rehabilitation programme improve anal continence and quality of life? Color Dis 14(10):1231–1237. https://doi.org/10.1111/j.1463-1318.2012.02956.x
Liang Z, Ding W, Chen W, Wang Z, Du P, Cui L (2016) Therapeutic evaluation of biofeedback therapy in the treatment of anterior resection syndrome after sphincter-saving surgery for rectal cancer. Clin Colorectal Cancer 15:101–107
Ridolfi TJ, Berger N, Ludwig KA (2016) Low anterior resection syndrome: current management and future directions. Clin Colon Rectal Surg 29(3):239–245. https://doi.org/10.1055/s-0036-1584500
Tan E, Ngo NT, Darzi A, Shenouda M, Tekkis PP (2011) Metaanalysis: sacral nerve stimulation versus conservative therapy in the treatment of faecal incontinence. Int J Color Dis 26(3):275–294. https://doi.org/10.1007/s00384-010-1119-y
Nakamura A, Osonoi T, Terauchi Y (2010) Relationship between urinary sodium excretion and pioglitazone-induced edema. J Diabetes Investig 1(5):208–211. https://doi.org/10.1111/j.2040-1124.2010.00046.x
Matzel KE, Stadelmaier U, Bittorf B, Hohenfellner M, Hohenberger W (2002) Bilateral sacral spinal nerve stimulation for fecal incontinence after low anterior rectum resection. Int J Color Dis 17(6):430–434. https://doi.org/10.1007/s00384-002-0412-9
Jarrett ME, Matzel KE, Stosser M, Christiansen J, Rose H, Kamm MA (2005) Sacral nerve stimulation for faecal incontinence following a rectosigmoid resection for colorectal cancer. Int J Color Dis 20(5):446–451. https://doi.org/10.1007/s00384-004-0729-7
Ratto C, Grillo E, Parello A, Petrolino M, Costamagna G, Doglietto GB (2005) Sacral neuromodulation in treatment of fecal incontinence following anterior resection and chemoradiation for rectal cancer. Dis Colon rectum 48(5):1027–1036. https://doi.org/10.1007/s10350-004-0884-5
de Miguel M, Oteiza F, Ciga MA, Armendariz P, Marzo J, Ortiz H (2011) Sacral nerve stimulation for the treatment of faecal incontinence following low anterior resection for rectal cancer. Color Dis 13(1):72–77. https://doi.org/10.1111/j.1463-1318.2009.02066.x
Moya P, Arroyo A, Soriano-Irigaray L, Frangi A, Candela Polo F, Calpena Rico R (2012) Sacral nerve stimulation in patients with severe fecal incontinence after rectal resection. Tech Coloproctol 16(3):263–264. https://doi.org/10.1007/s10151-012-0823-8
Schwandner O (2013) Sacral neuromodulation for fecal incontinence and ‘low anterior resection syndrome’ following neoadjuvant therapy for rectal cancer. Int J Color Dis 28(5):665–669. https://doi.org/10.1007/s00384-013-1687-8
Thin NN, Horrocks EJ, Hotouras A, Palit S, Thaha MA, Chan CL, Matzel KE, Knowles CH (2013) Systematic review of the clinical effectiveness of neuromodulation in the treatment of faecal incontinence. Br J Surg 100(11):1430–1447. https://doi.org/10.1002/bjs.9226
Holzer B, Rosen HR, Zaglmaier W, Klug R, Beer B, Novi G, Schiessel R (2008) Sacral nerve stimulation in patients after rectal resection - preliminary report. J Gastrointest Surg 12(5):921–925. https://doi.org/10.1007/s11605-008-0485-z
D'Hondt M, Nuytens F, Kinget L, Decaestecker M, Borgers B, Parmentier I (2017) Sacral neurostimulation for low anterior resection syndrome after radical resection for rectal cancer: evaluation of treatment with the LARS score. Tech Coloproctol 21(4):301–307. https://doi.org/10.1007/s10151-017-1612-1
Spiller RC (2011) Targeting the 5-HT(3) receptor in the treatment of irritable bowel syndrome. Curr Opin Pharmacol 11(1):68–74. https://doi.org/10.1016/j.coph.2011.02.005
Itagaki R, Koda K, Yamazaki M, Shuto K, Hirano A, Arimitsu H, Shiragami R, Yoshimura Y, Suzuki M (2014) Serotonin (5-HT3) receptor antagonists for the reduction of symptoms of low anterior resection syndrome. Clin Exp Gastroenterol 7:47–52. https://doi.org/10.2147/CEG.S55410
Iwama T, Imajo M, Yaegashi K, Mishima Y (1989) Self washout method for defecational complaints following low anterior resection. Jpn J Surg 19(2):251–253. https://doi.org/10.1007/BF02471596
Blair GK, Djonlic K, Fraser GC, Arnold WD, Murphy JJ, Irwin B (1992) The bowel management tube: an effective means for controlling fecal incontinence. J Pediatr Surg 27(10):1269–1272. https://doi.org/10.1016/0022-3468(92)90271-8
Del Popolo G, Mosiello G, Pilati C, Lamartina M, Battaglino F, Buffa P, Redaelli T, Lamberti G, Menarini M, Benedetto P di, Gennaro M de (2008) Treatment of neurogenic bowel dysfunction in patients with spinal cord injury. Spinal Cord 46(7):517–522. https://doi.org/10.1038/sj.sc.3102167
Christensen P, Krogh K (2010) Transanal irrigation for disordered defecation: a systematic review. Scand J Gastroenterol 45(5):517–527. https://doi.org/10.3109/00365520903583855
Christensen P, Krogh K, Buntzen S, Payandeh F, Laurberg S (2009) Long-term outcome and safety of transanal irrigation for constipation and fecal incontinence. Dis Colon rectum 52(2):286–292. https://doi.org/10.1007/DCR.0b013e3181979341
Rosen H, Robert-Yap J, Tentschert G, Lechner M, Roche B (2011) Transanal irrigation improves quality of life in patients with low anterior resection syndrome. Color Dis 13:335–338
Koch SM, Rietveld MP, Govaert B, van Gemert WG, Baeten CG (2009) Retrograde colonic irrigation for faecal incontinence after low anterior resection. Int J Color Dis 24(9):1019–1022. https://doi.org/10.1007/s00384-009-0719-x
Cazemier M, Felt-Bersma RJ, Mulder CJ (2007) Anal plugs and retrograde colonic irrigation are helpful in fecal incontinence or constipation. World J Gastroenterol 13(22):3101–3105. https://doi.org/10.3748/wjg.v13.i22.3101
Stephens JH, Hewett PJ (2012) Clinical trial assessing VSL#3 for the treatment of anterior resection syndrome. ANZ J Surg 82(6):420–427. https://doi.org/10.1111/j.1445-2197.2012.06082.x
Altomare DF, Picciariello A, Ferrara C, Digennaro R, Ribas Y, de Fazio M (2017) Short-term outcome of percutaneous tibial nerve stimulation for low anterior resection syndrome: results of a pilot study. Colorectal Dis doi 19(9):851–856. https://doi.org/10.1111/codi.13669. [Epub ahead of print]
Vigorita V, Rausei S, Troncoso Pereira P, Trostchansky I, Ruano Poblador A, Moncada Iribarren E, Facal Alvarez C, de San Ildefonso Pereira A, Casal Núñez E (2017) A pilot study assessing the efficacy of posterior tibial nerve stimulation in the treatment of low anterior resection syndrome. Tech Coloproctol 21(4):287–293. https://doi.org/10.1007/s10151-017-1608-x
Chen TY, Emmertsen KJ, Laurberg S (2014) Bowel dysfunction after rectal cancer treatment: a study comparing the specialist's versus patient's perspective. BMJ Open 4(1):e003374. https://doi.org/10.1136/bmjopen-2013-003374
Martellucci J (2016) Low anterior resection syndrome: a treatment algorithm. Dis Colon rectum 59(1):79–82. https://doi.org/10.1097/DCR.0000000000000495
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Dulskas, A., Smolskas, E., Kildusiene, I. et al. Treatment possibilities for low anterior resection syndrome: a review of the literature. Int J Colorectal Dis 33, 251–260 (2018). https://doi.org/10.1007/s00384-017-2954-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-017-2954-x