Abstract
Introduction
We aimed to evaluate adherence to the EAU guidelines (GL) on penile cancer (PC) with regard to primary surgical treatment and management of lymph nodes and to estimate the influence of adherence to GL on clinical outcome.
Materials and methods
This is a retrospective multicenter study (PEnile Cancer ADherence study, PECAD Study) on PC patients treated at 12 European and American centers between 2010 and 2016. Adherence to the EAU GL on the surgical management of the primary penile tumor and lymphadenectomy was evaluated. Descriptive analyses were performed, and survival curves were estimated.
Results
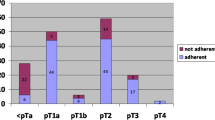
Data on 425 patients were considered for the analysis. The EAU GL on surgical treatment of the primary tumor and lymphadenectomy were respected in 74.8% and 73.7% of cases, respectively. Survival analysis showed that adherence to the GL on primary penile surgery was significantly associated with a good overall survival [adjusted HR 0.40 (95% CI 0.20–0.83, p value = 0.014)]. Also, the adherence to the GL on lymphadenectomy was statistically significantly associated with overall survival [adjusted HR 0.48 (95% CI 0.24–0.96, p value = 0.038)]. Limited follow-up and retrospective design represent limitations of this study.
Conclusions
Our findings suggest that there is a good adherence to the EAU GL on PC. However, this should be further reinforced, endorsed and encouraged as it might translate into better clinical outcomes for PC patients.



Similar content being viewed by others
References
Barnholtz-Sloan JS, Maldonado JL, Pow-sang J, Giuliano AR (2007) Incidence trends in primary malignant penile cancer. Urol Oncol 25:361–367
Christodoulidou M, Sahdev V, Houssein S, Muneer A (2005) Epidemiology of penile cancer. Curr Probl Cancer 39:126–136
Siegel RL, Miller KD, Jemal A et al (2016) Cancer statistics 2016. CA Cancer J Clin 66:7–30
Djajadiningrat RS, Graafland NM, van Werkhoven E et al (2014) Contemporary management of regional nodes in penile cancer-improvement of survival? J Urol 191:68–73
Pandey D, Mahajan V, Kannan RR (2006) Prognostic factors in node-positive carcinoma of the penis. J Surg Oncol 93:133–138
Hakenberg OW, Compérat EM, Minhas S et al (2015) EAU guidelines on penile cancer: 2014 update. Eur Urol 67:142–150
Lont AP, Gallee MP, Meinhardt W, van Tinteren H, Horenblas S (2006) Penis conserving treatment for T1 and T2 penile carcinoma: clinical implications of a local recurrence. J Urol 176:575–580
Clark PE, Spiess PE, Agarwal N et al (2013) Penile cancer: clinical practice guidelines in oncology. J Natl Compr Canc Netw 11:594–615
Baumgarten A, Chipollini J, Yan S et al (2017) Penile sparing surgery for penile cancer: a multicenter international retrospective cohort. J Urol 199(5):1233–1237
Kamel MH, Tao J, Su J et al (2018) Survival outcomes of organ sparing surgery, partial penectomy, and total penectomy in pathological T1/T2 penile cancer: report from the National Cancer Data Base. Urol Oncol. 36(2):82.e7–82.e15
Kirrander P, Sherif A, Friedrich B, Lambe M, Hakansson U (2016) Swedish national penile cancer register: incidence, tumour characteristics, management and survival. BJU Int 117:287–292
Hughes BE, Leijte JA, Kroon BK et al (2010) Lymph node metastasis in intermediate-risk penile squamous cell cancer: a two-centre experience. Eur Urol 57(4):688–692
Graafland NM, Lam W, Leijte JA et al (2010) Prognostic factors for occult inguinal lymph node involvement in penile carcinoma and assessment of the high-risk EAU subgroup: a two-institution analysis of 342 clinically node-negative patients. Eur Urol 58(5):742–747
da Costa WH, Rosa de Oliveira RA et al (2016) Prognostic factors in patients with penile carcinoma and inguinal lymph node metastasis. Int J Urol 22:669–673
Zargar-Shoshtari K, Sharma P, Djajadiningrat R et al (2016) Extent of pelvic lymph node dissection in penile cancer may impact survival. World J Urol 34:353–359
Zhu Y, Gu CY, Ye DW (2014) Population-based assessment of the number of lymph nodes removed in the treatment of penile squamous cell carcinoma. Urol Int 92:186–193
Joshi SS, Handorf E, Strauss D, et al. (2018) Treatment trends and outcomes for patients with lymph node-positive cancer of the penis. JAMA Oncol https://doi.org/10.1001/jamaoncol.2017.5608. [Epub ahead of print]
Johnson TV, Hsiao W, Delman KA et al (2010) Extensive inguinal lymphadenectomy improves overall 5-year survival in penile cancer patients: results from the surveillance, epidemiology, and end results program. Cancer 116:2960–2966
Heins MJ, de Jong JD, Spronk I, Ho VK, Brink M, Korevaar JC (2017) Adherence to cancer treatment guidelines: influence of general and cancer-specific guideline characteristics. Eur J Public Health 27(4):616–620
Cabana MD, Rand CS, Powe NR et al (1999) Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA 282:1458–1465
Rieken M, Djajadiningrat RS, Kluth LA et al (2014) Predictors of cancer-specific mortality after disease recurrence in patients with squamous cell carcinoma of the penis. Eur Urol 66:811–814
Campbell RA, Slopnick EA, Ferry EK, Zhu H, Kim SP, Abouassaly R (2017) Disparity between pre-existing management of penile cancer and NCC guidelines. Urol Oncol 35(8):531.e9–531.e14
Tang DH, Yan S, Ottenhof SR, Draeger D et al (2018) Laser ablation as monotherapy for penile squamous cell carcinoma: a multi-center cohort analysis. Urol Oncol. 36(4):147–152
Albersen M, Parnham A, Joniau S et al (2017) Predictive factors for local recurrence after glansectomy and neoglans reconstruction for penile squamous cell carcinoma. Urol Oncol pii S1078–1439(17):30387–30388
Thuret R, Sun M, Lughezzani G, Budaus L et al (2011) A contemporary population-based assessment of the rate of lymphnode dissection for penile carcinoma. Ann Surg Oncol 18:439–446
Breen KJ, O’Connor KM, Power DG, Mayer NJ, Rogers E, Sweeney P (2005) Penile cancer-guidelines adherence produces optimum results. Surgeon 13(4):200–206
Sharma P, Zargar H, Spiess PE (2016) Surgical advances in inguinal lymph node dissection: optimizing treatment outcomes. Urol Clin North Am 43:457–468
Spiess PE, Hernandez MS, Pettaway CA (2009) Contemporary inguinal lymph node dissection: minimizing complications. World J Urol 27:205–212
Leijte JAP, Kirrander P, Antonini N, Windahl T, Horenblas S (2008) Recurrence patterns of squamous cell carcinoma of the penis: recommendations for follow-up based on a two-centre analysis of 700 patients. Eur Urol 54:161–168
Briganti A, MacLennan S, Marconi L, Plass K, N’Dow J (2016) European Association of Urology (EAU) guidelines: do we care? Reflections from the EAU impact assessment of guidelines implementation and education group. BJU Int 117(6):850–851
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cindolo, L., Spiess, P.E., Bada, M. et al. Adherence to EAU guidelines on penile cancer translates into better outcomes: a multicenter international study. World J Urol 37, 1649–1657 (2019). https://doi.org/10.1007/s00345-018-2549-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-018-2549-3