Abstract
Purpose
To report the extended long-term results of the use of tension-free vaginal tape(TVT) and trans-obturator tape (TOT) for the treatment of female stress urinary incontinence (SUI).
Methods
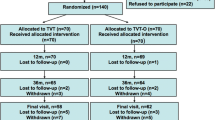
A prospective, multicentre randomized clinical trial comparing the use of TVT and TOT was used to evaluate 87 patients. The inclusion criteria were stress or mixed UI associated with urethral hyper mobility (the stress component was clinically predominant), while the exclusion criteria were previous anti-incontinence surgery and/or pelvic organ prolapse. The objective cure criteria were a negative provocative stress test and a negative 1-h pad test, with no further treatment for SUI. The subjective cure criteria were a 3-day voiding diary, quality-of-life questionnaires (UDI6–IIQ7), and patient satisfaction on a scale from 0 to 10.
Results
Eighty-seven patients were evaluated (47 TOT and 40 TVT) at a median follow-up of 100 months. Subjective and objective cure rates were 59.6 and 70.2 % in the TOT group and 75 and 87.5 % in the TVT group. The mid-to-long-term trend was a decreasing continence rate in patients who underwent TOT, compared with a stable rate for TVT. The Kaplan–Meier survival curve showed that continence rate decreased for up to 25 months after surgery, with stabilization thereafter for the TVT group while continuing to drop in the TOT group, with no inter-group difference.
Conclusion
The patients in both groups were highly satisfied at long-term follow-up. The overall continence rate worsened for both groups within 25 months. While the results tend to stabilize in the TVT group, a further decline in the TOT was observed.
Similar content being viewed by others
Introduction
Tension-free mid-urethral slings, retropubic and trans-obturator (TVT and TOT, respectively), have been increasingly used for the treatment of stress urinary incontinence (SUI). TVT and TOT are currently considered the gold standard of SUI surgery [1, 2]. A Cochrane review and different meta-analyses evaluating the outcomes of retropubic and trans-obturator sling procedures showed no significant difference between objective and subjective outcomes of the two sling approaches [3–6].
One of the most significant drawbacks of randomised controlled studies is the absence of long-term follow-up, which provide crucial information necessary for proper patient counselling with regard to significantly lengthening female life expectancy in developed countries. Previously, we reported the short- and mid-term results of a large, multicentre randomized controlled trial that compared the efficacy and safety of the trans-obturator and retropubic mid-urethral slings [7, 8]. The purpose of the present paper is to report the extended long-term follow-up data of women who had been recruited in the previous study.
Materials and methods
The study design was previously reported [7]. For the current analysis, we collected the long-term data of women enroled in the previous study. The study was granted by an independent medical association (TETI), whose mission is to fund objective and patient-reported long-term outcome assessments for genitourinary disease [www.tetiassociation.com]. IRB approval was obtained to conduct a follow-up to the previous RCT study.
The inclusion criteria were stress or mixed urinary incontinence associated with urethral hypermobility, according to ICS classification (the stress component was clinically predominant). Exclusion criteria were previous anti-incontinence surgery and pelvic organ prolapse (POP) greater than stage I in any vaginal compartment, according to the POP-Q system [9] classification. The pre-operative workup included a detailed case history; clinical, neurological, and urogynaecological examination; and the compiled results of the Urogenital Distress Inventory (UDI-6) and Impact Incontinence Quality of Life (IIQ7) Questionnaires. Voiding and storage symptoms were evaluated on the basis of ICS classification. All patients underwent cough and Valsalva stress tests at physiological maximum bladder capacity. The same tests were performed again at 3, 6, and 12 months, and then annually. All patients underwent pre-operative urodynamic testing, including Valsalva leak point pressure (VLPP) evaluations. Standard operative techniques were, respectively, the TVT according to Ulmsten (TVT; Gynecare; Ethicon, Somerville, NJ, USA) and TOT according to Delorme techniques (Obtape; Mentor–Porges, Le Plessis-Robinson, France) [10].
All the recruited patients were invited for a clinical assessment between October 2012 and June 2013. The primary outcome was determined by the objective and subjective cure rates assessment. The objective cure rate assessment was based on repeated negative provocative stress tests with the bladder filled to capacity and a negative 1-h pad test, with no further treatment for any urinary incontinence (behavioural, pharmacologic, or surgical). The subjective criteria were assessed with a 3-day voiding diary, quality-of-life questionnaires (UDI6–IIQ7), patient satisfaction on a scale of 0–10 (with 10 indicating the highest satisfaction and 0 the lowest), and the single question of whether they would repeat the same procedure. Finally, a comparison between mid- and long-term follow-up results and the original RCT study was made in the same group of women.
Statistical analysis
Chi-square and Mann–Whitney U tests were used to analyse categorical and continuous data; Wilcoxon signed rank tests were used to compare discrete paired data; and the Kaplan–Meier estimator was used to estimate relapse-free survival rates. Survival times were measured in months and were censored either at the date a patient was lost to follow-up, or at the date of the last follow-up. A log-rank test was conducted to compare event-free survivals. Statistical analysis was performed by using IBM SPSS, version 21.0, 2012. A power analysis calculation was performed using PS Power and Sample Size software, rel. 3.0, 2009.
The power analysis indicated that a sample size of 87 patients (47 for the TOT group and 40 for the TVT group) provided a statistical power (1-β) of at least 80 % at α = 0.05 for the detection of 30 %, in differences in proportion of any postoperative condition between the two groups, when the lower frequency of the condition was equal to 50 %.
Results
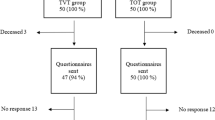
The entire cohort of patients enroled (95 patients) was contacted (51 TOT and 44 TVT). Two of the 95 patients died, and six did not participate in the follow-up (three TOT and three TVT). A total of 87 patients were evaluated (47 TOT and 40 TVT), with a median follow-up of 100 months (range 75–131). At the last follow-up, the TVT and TOT groups were still comparable with regard to their age distribution, body mass index, menopausal status, and parity (Table 1). There were no statistically significant differences between the TOT and TVT groups in pre-operative voiding (p = 0.601) or in storage symptoms (p = 0.912)
Subjective and objective results for incontinence in the TOT group (median follow-up 99 months; range 75–124 months) and TVT group (median follow-up 111 months; range 75–131 months) are reported in Table 2. Twenty-eight out of 47 patients (59.6 %) in the TOT group were subjectively dry versus 30 out of 40 (75 %) in the TVT group. On the basis of objective criteria, 33 (70.2 %) were found to be dry in the TOT group. In this group, four patients underwent reintervention for recurrent SUI (one Burch colposuspension and three TVT), two for POP repair, and seven for mesh revision. In two of seven cases, mesh extrusion occurred in the first 3 months; in one case, after 6 months; in two cases, after 1 year; and in two cases, after 2 years: all of these patients presented with vaginal discharge. The four treated patients remained dry for at least 1 year after surgery; for the other three patients in which the early exposure appeared, SUI recurred after mesh removal. Three patients in the TVT group underwent reintervention: one for POP, one for para-incisional hernia, and one for suprapubic granuloma.
At final evaluation, 39 patients (83 %) in the TOT group said they would repeat incontinence surgery, with a post-operative mean VAS score of 7.8 ± 2.2 (median 8; range 0–10) versus 35 patients (87.5 %) in the TVT group, with a post-operative mean VAS score of 8.2 ± 2.1 (median 9; range 0–10). In both groups, the post-operative questionnaire scores showed a significant improvement (p < 0.0001), with no difference between the TOT and TVT groups (Table 1). At final evaluation, 82.9 % of the patients in the TOT group and 87.5 % in the TVT group would repeat surgery.
Overall subjective incontinence outcomes at mid- and long-term follow-up were not associated with either pre-operative detrusor overactivity or with pre-operative storage symptoms for both groups (Table 3). When comparing the incontinence outcomes with the pre-operative VLPP, no association was demonstrated for VLPP values <60 cm H2O at 3 and 6 years follow-up (Table 4). Figure 1 shows the success rates and their differences in incontinence, voiding symptoms and storage symptoms at 3 and 6 years, respectively, for both TOT and TVT. Storage symptoms, which have the most significant impact on patients’ quality of life, were treated in nine patients in the TOT group and ten in the TVT group with anti-cholinergic therapy. Comparing the long-term follow-up results to the mid-term, the continence rate after mid-urethral slings tended to decrease in patients who underwent TOT, while it remained stable for patients who underwent TVT. Voiding and storage symptoms seemed to be better for TOT patients, although no definitive statistical consideration could be done due to the low number of patients. The Kaplan–Meier survival curve (Fig. 2) shows that the continence rate decreased up until 25 months, following which the results remained stable for the TVT group, while they decreased in the TOT group. Figure 3 shows how free survival times from storage symptoms are not significantly different between the two groups. Again, the disturbance appeared in the majority of patients within 25 months, following which the decline over time became evident.
Figure 4 shows that the free survival times from voiding symptoms were also not significantly different after surgery between the two groups. The symptoms worsened within the initial months and stabilized afterwards until 75 months, after which the symptoms tended to worsen over time. In the TOT group, four patients eventually underwent reintervention for recurrent/persistent SUI.
In the TOT group, voiding symptoms appeared de novo in the long-term follow-up in seven patients. However, none of these patients were suffering from bladder outlet obstruction, as confirmed by flowmetry data (Fig. 5), and no patients needed surgery to release the sling. In three cases, the urodynamic data showed a decrease in pdet Qmax (10 cm H2O) suggestive for detrusor hypocontractility (Qmax of 15 ml/sec); one patient showed a reduction in Qmax with normal pressure parameters and no post-void residue, and three patients showed a detrusor overactivity with normal pressure values during voiding phase (two of these patients showed similar parameters in the pre-operative urodynamic, and one patient developed fibromyalgia). None of these patients had a urodynamic obstruction, and all the patients developed the symptoms after at least 2 years.
In the TVT group, de novo voiding symptoms developed in five patients. Urodynamic data showed normal parameters in one patient and hypocontractility in one patient 4 years after TVT surgery; one patient developed a cystocele after 3 years with a urodynamic diagnosis of mild obstruction, and two patients presented a persistence of DO with normal detrusor pressures.
None of the patients reported groin pain or presented recurrent urinary tract infections (UTIs) related to chronic obstructions. During the follow-up, eight patients in the TOT group and eight in the TVT group presented sporadic uncomplicated UTIs. Recurrent UTIs were reported in two cases in the TOT group and three in the TVT group; however, all the patients referred the same problems in the pre-operative evaluation. No difference between the groups emerged.
Discussion
Over the course of the long follow-up period in our randomized study, we confirmed that mid-urethral slings are an effective option for the treatment of SUI. The overall continence rate worsened for both the TVT and TOT groups within the first 25 months after the procedure. While the results tended to stabilize in the TVT group, a further decline occurred in the TOT group. Although the use of a problematic mesh, such as the Obtape, could potentially undermine the value of this study, the results, excluding the patients who received mesh revisions, showed a 60 % dry rate in TOT versus 75 % dry rate in TVT.
Retropubic and trans-obturator mid-urethral slings represent the most effective current procedures for the surgical treatment of SUI, and they are considered to be the gold standard [1]. However, few studies have reported the long-term outcomes of these procedures. Determining these long-term outcomes is of paramount importance, due to the increasing life expectancy of women seeking SUI treatment in the Western world. In our study, we observed that the continence rate after trans-obturator mid-urethral slings dropped from 77.3 to 59.6 %, while the results after TVT remained stable over time (75 %), as has been confirmed by other authors [2, 11]
In our previous publication, we concluded that TOT appeared to be as safe and effective as TVT in surgery for female SUI, with minimal complications at mean follow-up of 31 months [7]. The Cochrane review [4], comparing retropubic and trans-obturator mid-urethral slings, demonstrated subjective cure rates of 83 %, with no statistically significant difference between the two approaches at 12 months. However, longer follow-up results were not available. Similar to our findings, an updated review on SUI surgery by Novara et al. [6] found similar subjective cure rates and a trend towards higher objective efficacy in the retropubic group.
All of the reported results on the mid- and long-term follow-up for the retropubic approach confirm a continence rate that is stable over time. Serati et al. [11] evaluated the outcomes of women who received TVT for urodynamic stress incontinence (USI) after their 10-years follow-up and reported subjective, objective, and urodynamics cure rates of 89.7, 93.1, and 91.4 %, respectively, which were stable across the entire study period (p > 0.99). However, they reported 18.9 % of the patients with de novo overactive bladder (OAB), with 43.8 % of the patients non-responsive to anti-muscarinic drugs. Taking into account the different definitions of outcome in our study, in which dry patients without urgency or SUI were considered, the results of this study could be considered to overlap with our 75 % of patients found to be dry.
Two other studies comparing retropubic and trans-obturator tape confirmed our results. Albo et al. [12] reported 24-month continence rates, complications, and symptom outcomes from a randomized equivalence trial. The objective success rates for retropubic and trans-obturator mid-urethral slings were 77.3 and 72.3 %, respectively, and the subjective success rates were 55.7 and 48.3 %, respectively. The objective success criteria for equivalence at 12 months were no longer met at 24 months, although patient satisfaction remained high, and symptom severity improved. The use of composite outcomes to define treatment success (in our study, the continence rate was the combination of subjective and objective evaluation) resulted in lower success rates.
Our results are also comparable to those reported by Schierlitz et al. [13]. In this study, 164 women were randomly assigned to either a TVT or TOT group, and the primary outcome studied, assessed at the 3-year follow-up, was symptomatic stress incontinence requiring surgical reintervention. Secondary outcomes were quality-of-life parameters assessed by validated questionnaires and numerical success scores. The results showed that it was necessary for 20 % of the TOT group patients to repeat surgery, compared with 1.4 % in the TVT group. These data are confirmed in our study, where only in the TOT group (8.5 %) was a reintervention for recurrent SUI needed. The Schierlitz et al. [13] study showed no difference between the two slings with regard to quality-of-life outcomes and concluded that the long-term cure rates for USI and intrinsic sphincter deficiency were significantly greater for women who received a retropubic TVT than the long-term cure rates for women who received a TOT. Possible explanations for the higher success rate of TVT compared with TOT may be the difference in sling axis and the more distal location of the trans-obturator tape, resulting in more urethral kinking during straining in the TVT group, which can be seen on ultrasonography [16, 17]. On the basis of our Kaplan–Meier curve (Fig. 3), our results confirm the findings of previous studies on the long-term results after MUSs. Our results also add a further consideration, which is the stability of the incontinence results (in particular for TVT), over time [4, 11, 18]. Within 25 months of the initial surgery, the failure rate was relatively high for both the slings, following which it stabilized. Additionally, major complications, such as mesh extrusion, appeared in the first 2 years.
The tendency of an effectiveness decline of synthetic sling during the time has been also shown by the TOMUS trial [15]. In this paper, the authors suggested that patients with poor urethral function have better success rates with retropubic than trans-obturator MUS because the vector forces provided by a retropubic sling may be more compressive than that provided by a trans-obturator sling. Basing on this consideration, therefore, the knowledge of poor urethral function pre-operatively might be important when selecting the surgical technique. Even if in our experience we did not make this observation, it can be one of the aspects that should be taken into consideration [14, 15].
The results of this study could represent an important milestone in the proper counselling of patients regarding the long-term outcomes of sling procedures. A thorough follow-up should be mandatory in the first 2 years after surgery, as adverse events, such as mesh exposure and recurrence of SUI, typically occur within the first 24 months.
The presence of post-operative storage symptoms and the onset of de novo OAB symptoms, together with their progression and their possible treatment, is one of the most clinically relevant and largely debated post-operative complications of mid-urethral slings. Previous studies have reported de novo urgency rates ranging from 4 to 33 % after TVT [6, 19–21]. It is almost impossible to address this large discrepancy, as it could be related to different definitions and questionnaires adopted to collect OAB symptoms, to the different demographic characteristics of women included, or to the different concomitant surgical procedures associated with TVT. In their long-term results after TVT-O, Serati et al. [18] reported 24.3 % of patients with de novo OAB symptoms after 5-year follow-up. Our long-term findings (presence of storage symptoms in 20 % of the TOT group and 36.8 % of the TVT group) and the Kaplan–Meier curve, describing the onset of post-operative storage symptoms, confirmed the relevance of this problem and how it tends to worsen over time. This does not seem to be related to the anti-incontinence procedure, because we cannot exclude the possibility that a certain percentage of women may naturally develop OAB symptoms due to their ageing and other comorbidities with their confounding roles.
The same considerations should be made at the onset of post-operative voiding symptoms. They worsened within the first few months after the procedure, stabilized up until 75 months, and then tended to worsen over time, clearly related to other factors. Voiding and storage symptoms seemed to be better, although not statistically significant, for TOT patients (Fig. 1). This may help to explain why the overall TOT patient satisfaction was maintained while SUI cure rates fell. However, independent of incontinence status, other factors may change the outcome’s perception. For example, the patient’s age, general health, or comorbidities may worsen QoL and affect the outcome of incontinence surgery even if not directly related to it. Extended follow-up periods could be subject to an increased measurement error [22]. Patients’ recollections of the experience during the reference period are what matters most, and any response process—even for current status—relies on cognitive processing and memory. Furthermore, other elements could affect the outcome measures. In the evaluation of voiding symptoms in the long term, we had seven patients in the TOT group and five in the TVT group. In these patients, the symptoms could be related to factors not dependent on anti-incontinence surgery such as normal ageing detrusor process or new pathologies that occurred during the follow-up (vaginal prolapse, stroke, Parkinson’s disease, myeloma, kidney tumour). This represents one of the reasons that do not allow us to reach a definitive conclusion.
Strength of this study is the comprehensive clinical evaluation performed in the majority of the patients after a long follow-up, which was based not only on a telephone interview but on strict follow-up with the patients to obtain data over a long period. We acknowledge that a limitation of this study is the limited sample size, as patients were recruited in just one urogynaecological centre, even though a low percentage of patients were lost in follow-up and though there was no bias due to different surgical techniques and evaluations. Another limitation of the study is that two different meshes were used, and their composition could potentially be responsible for some of the differences in our study. Finally, we should also consider that patients may not have been able to give accurate responses when the long-term follow-ups were conducted due to possible cognitive decline.
Conclusion
The long-term results of this study demonstrated that mid-urethral slings are an effective option for treatment of SUI with high level of patient satisfaction. After being initially effective, effectiveness for the TOT group declined over time.
References
Serati M, Salvatore S, Uccella S et al (2009) Surgical treatment for female stress urinary incontinence: what is the gold-standard procedure? Int Urogynecol J Pelvic Floor Dysfunct 20:619–621
Oliphant SS, Wang L, Bunker CH, Lowder JL (2009) Trends in stress urinary incontinence inpatient procedures in the United States, 1979–2004. Am J Obstet Gynecol 200(5):521.e1–521.e6
Novara G, Ficarra V, Boscolo-Berto R, Secco S, Cavalleri S, Artibani W (2007) Tension free mid-urethral slings in the treatment of female stress urinary incontinence: a systematic review and meta-analysis of randomized controlled trials of effectiveness. Eur Urol 52:663–678
Ogah J, Cody JD, Rogerson L (2009) Minimally invasive synthetic suburethral sling operations for stress urinary incontinence in women. Cochrane Database Syst Rev (4):CD006375. doi:10.1002/14651858.CD006375.pub2
Latthe PM, Foon R, Toozs-Hobson P (2007) Transobturator and retropubic tape procedures in stress urinary incontinence: a systematic review and meta-analysis of effectiveness and complications. BJOG 114:522–531
Novara G, Galfano A, Boscolo-Berto R et al (2008) Complication rates of tension-free mid-urethral slings in the treatment of female stress urinary incontinence: a systematic review and meta-analysis of randomized controlled trials comparing tension-free midurethral tapes to other surgical procedures and different devices. Eur Urol 53:288–308
Porena M, Costantini E, Frea B, Giannantoni A, Ranzoni S, Mearini L, Bini V, Kocjancic E (2007) Tension-free vaginal tape versus Transobturator tape as surgery for stress urinary incontinence: results of a multicentre randomised trial. Eur Urol 52:1481–1491
Costantini E, Lazzeri M, Zucchi A, Di Biase M, Porena M (2014). Long-term efficacy of the transobturator and retropubic mid-urethral slings for stress urinary incontinence: single-center update from a randomized controlled trial. Eur Urol 66(3):599–601
Bump RC, Mattiasson A, Bo K et al (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–17
De Lorme E (2001) Transobturator urethral suspension: mini-invasive procedure in the treatment of stress urinary incontinence in women. Prog Urol 11:1306–1313
Serati M, Ghezzi F, Cattoni E, Braga A et al (2012) Tension-free vaginal tape for the treatment of urodynamic stress incontinence: efficacy and adverse effects at 10-year follow-up. Eur Urol 61:939–946
Albo ME, Litman HJ, Richter HE et al (2012) Urinary incontinence reatment network. Treatment network treatment success of retropubic and transobturator mid urethral slings at 24 months. J Urol 188:2281–2287
Schierlitz L, Dwyer PL, Rosamilia A et al (2012) Three-year follow-up of tension-free vaginal tape compared with transobturator tape in women with stress urinary incontinence and intrinsic sphincter deficiency. Obstet Gynecol 119(2, Part 1):321–327
Costantini E, Lazzeri M, Giannantoni A et al (2008) Preoperative Valsalva leak point pressure may not predict outcome of mid-urethral slings. Analysis from a randomized controlled trial of retropubic versus transobturator mid-urethral slings. Int Braz J Urol 34(1):73–83
Nager CW, Sirls L, Litman HJ et al (2011) Urinary incontinence treatment network. baseline urodynamic predictors of treatment failure 1 year after mid urethral sling surgery. J Urol 186:597–603
De Lancey JO (1994) Structural support of the urethra as it relates to stress urinary incontinence: the hammock hypothesis. Am J Obstet Gynecol 170:1713–1720
Whiteside JL, Walters MD (2004) Anatomy of the obturator region: relations to a trans-obturator sling. Int Urogynecol J Pelvic Floor Dysfunct 15:223–226
Serati M, Bauer R, Cornu JN, Cattoni E et al (2013) TVT-O for the treatment of pure urodynamic stress incontinence: efficacy, adverse effects, and prognostic factors at 5-year follow-up. Eur Urol 63:872–878
Debodinance P, Delporte P, Engrand JB, Boulogne M (2002) Tension-free vaginal tape (TVT) in the treatment of urinary stress incontinence: 3 years experience involving 256 operations. Eur J Obstet Gynecol Reprod Biol 105:49–58
Ustun Y, Engin-Ustun Y, Gungor M, Tezcan S (2003) Tension-free vaginal tape compared with laparoscopic Burch urethropexy. J Am Assoc Gynecol Laparosc 10:386–389
Ward KL, Hilton P, UK and Ireland TVT Trial Group (2004) A prospective multicenter randomized trial of tension-free vaginal tape and colposuspension for primary urodynamic stress incontinence two-year follow-up. Am J Obstet Gynecol 190:324–331
Costantini E, Lazzeri M (2010) Elephants can remember. Eur Urol 58(5):678–679
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that all conflicts of interest, including specific financial interests and relationships and affiliations relevant to the subject matter or materials discussed in the manuscript (e.g. employment/affiliation, grants or funding, consultancies, honoraria, stock ownership or options, expert testimony, royalties, or patents filed, received, or pending), are the following: None.
Authors contributions
Protocol/project development: Costantini, Zucchi, Lazzeri, Giannantoni, and Porena; data collection or management: Costantini, Kocjancic, and Zucchi’ data analysis: pastore, Giannantoni, Carbone, Bini, and Palleschi; manuscript writing/editing: Costantini, Kocjancic, Lazzeri, Giannantoni, Zucchi, Carbone, Bini, Palleschi, Pastore, and Porena.
Rights and permissions
About this article
Cite this article
Costantini, E., Kocjancic, E., Lazzeri, M. et al. Long-term efficacy of the trans-obturator and retropubic mid-urethral slings for stress urinary incontinence: update from a randomized clinical trial. World J Urol 34, 585–593 (2016). https://doi.org/10.1007/s00345-015-1651-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-015-1651-z