Abstract
Purpose
The aims were (1) to assess the pediatric lower urinary tract symptom score (SS) prior to treatment as a means of determining severity of overactive bladder (OAB) and (2) to investigate relationships between SS results and those of standard diagnostic modalities.
Materials and methods
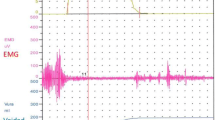
Symptom scores were recorded pre- and 6 months SS for 294 children with OAB unrelated to neurological disorder. Uroflowmetry–electromyography data, total bladder capacity, and a 2-day bladder diary were also recorded, and upper urinary tract deterioration was investigated as indicated. Overactive bladder was treated with standard approaches. No response to treatment was defined as 0–49 % reduction in OAB-related symptoms based on SS results. Non-responders underwent additional evaluations as indicated.
Results
Two hundred forty-one patients (97 %; mean age 9.8 ± 2.8 years; mean follow-up 11 months; range 6–18 months) completed the study. One hundred thirteen (47 %) required ultrasonography (USG), and those with abnormal USG had a significantly higher pre- and 6 months SS (p = 0.016). All non-responders (n = 38; 16 %) underwent urodynamics evaluation, 34 underwent spinal magnetic resonance imaging (MRI), 34 underwent voiding cystourethrography (VCUG), and 34 underwent dimercaptosuccinic acid scanning (DMSA). Non-responders with terminal detrusor hyperactivity had significantly lower SS after therapy (p = 0.09). Non-responders with abnormal MRI had higher pre- and 6 months SS than those with normal MRI. Thirteen (38 %) of the non-responders who required VCUG had vesicoureteral reflux (VUR), and this subgroup had higher pre-treatment SS (p = 0.030). Seven (21 %) of the non-responders who required DMSA had scarring, and all 7 had VUR. The subgroup with scarring had higher pre-treatment SS (p = 0.030).
Conclusion
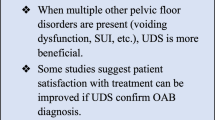
Pediatric OAB patients with high 6 months SS have a higher incidence of additional upper urinary tract pathology. Those with low pre-treatment SS require fewer laboratory tests and other assessments. The SS tool can reduce the number of urodynamics evaluations, and other tests required to diagnose renal damage in children with OAB.


Similar content being viewed by others
References
Sillén U, Brandström P, Jodal U et al (2010) The Swedish reflux trial in children: v. bladder dysfunction. J Urol 184(1):298–304
Nijman RJM, Bower W, Butler U et al (2005) Diagnosis and management of urinary incontinence and encopresis in children. In: Abrams P, Cardozo L, Khoury S et al (eds) Incontinence. Health Publication, Plymouth, p 965
Neveus T, vonGontard A, Hoebeke P et al (2006) The standardization of terminology of lower urinary tract functions in children and adolescents: report from the standardization committee of the International children’s continence society (ICCS). J Urol 176(1):314–324
Chung JM, Lee SD, Kang DI et al (2009) Korean enuresis association. Prevalence and associated factors of overactive bladder in Korean children 5–13 years old: a nationwide multicenter study. Urology 73(1):63–67
Kajiwara M, Inoue K, Kato M et al (2006) Nocturnal enuresis and overactive bladder in children: an epidemiological study. Int J Urol 13:36–41
Wallis MC, Khoury AE (2006) Symptom score for lower urinary tract dysfunction in pediatric urology. Curr Urol Rep 7(2):136–142
Akbal C, Genc Y, Burgu B et al (2005) Dysfunctional voiding and incontinence scoring system: quantitative evaluation of incontinence symptoms in pediatric population. J Urol 173:969–973
Yildirim A, Uluocak N, Atilgan D et al (2011) Evaluation of lower urinary tract symptoms in children exposed to sexual abuse. Urol J 8(1):38–42
Schneider D, Yamamoto A, Barone JG (2011) Evaluation of consistency between physician clinical impression and 3 validated survey instruments for measuring lower urinary tract symptoms in children. J Urol 186(1):261–265
Farhat W, Bagli DJ (2000) The dysfunctional voiding scoring system: quantitative standardization of dysfunctional voiding symptoms in children. J Urol 164:1011–1015
Nelson CP, Park JM, Bloom DA et al (2007) Incontinence symptom index and initial validation of a urinary incontinence instrument for the older pediatric population. J Urol 178:1763–1767
Fernbach SK, Maizels M, Conway JJ (1993) Ultrasound grading of hydronephrosis: introduction to the system used by the society for fetal urology. Pediatr Radiol 23:478–480
Lebowitz RL, Olbing H, Parkkulainen KV et al (1985) International system of radiographic grading of vesicoureteric reflux. International reflux study in children. Pediatr Radiol 15:105–109
Dik P, Klijn AJ, van Gool JD et al (2006) Early start to therapy preserves kidney function in spina bifida patients. Eur Urol 49:908–913
Vande Walle J, Rittig S, Bauer S et al (2012) American academy of pediatrics; European society for paediatric urology, European society for paediatric nephrology; International children’s continence society, practical consensus guidelines for the management of enuresis. Eur J Pediatr 171(6):971–983
Abrams P (2003) Describing bladder storage function: overactive bladder syndrome and detrusor overactivity. Urology 62(5 Suppl 2):28–37
Glassberg KI, Combs AJ, Horowitz M (2010) Nonneurogenic voiding disorders in children and adolescents: clinical and videourodynamic findings in 4 specific conditions. J Urol 184(5):2123–2127
Pippi Salle JL, Capolicchio G, Houle AM et al (1998) Magnetic resonance imaging in children with voiding dysfunction: is it indicated? J Urol 160(3 Pt 2):1080–1083
Arikan N, Soygür T, Selçuki M et al (1999) Role of magnetic resonance imaging in children with voiding dysfunction: retrospective analysis of 81 patients. Urology 54(1):157–160
Neveus T, Lackgren G, Tuvemo T et al (2000) Enuresis-background and treatment. Scand J Urol Nephrol Suppl 206:1–44
Milsom I, Abrams P, Cardozo L et al (2001) How widespread are the symptoms of an overactive bladder and how are they managed? A population-based prevalence study. BJU Int 87:760–766
Snodgrass W (1998) The impact of treated dysfunctional voiding on the nonsurgical management of vesicoureteral reflux. J Urol 160:1823–1825
van Gool JD, Hjalmas K, Tamminen-Mobius T et al (1992) Historical clues to the complex of dysfunctional voiding, urinary tract infection and vesicoureteral reflux. The International reflux study in children. J Urol 148:1699–1702
Homayoon K, Chen JJ, Cummings JM et al (2005) Voiding dysfunction: outcome in infants with congenital vesicoureteral reflux. Urology 66:1091–1094
Koff SA (1992) Relationship between dysfunctional voiding and reflux. J Urol 148:1703–1705
Yeung CK, Sreedhar B, Sihoe JD et al (2006) Renal and bladder functional status at diagnosis as predictive factors for the outcome of primary vesicoureteral reflux in children. J Urol 176:1152–1156
Godley ML, Desai D, Yeung CK et al (2001) The relationship between early renal status and the resolution of vesico-ureteric reflux and bladder function at 16 months. BJU Int 87:457–462
Soygur T, Arikan N, Tokatli Z et al (2004) The role of video-urodynamics studies in managing non-neurogenic voiding dysfunction in children. BJU Int 93:841–843
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Akbal, C., Şahan, A., Şener, T.E. et al. Diagnostic value of the pediatric lower urinary tract symptom score in children with overactive bladder. World J Urol 32, 201–208 (2014). https://doi.org/10.1007/s00345-013-1224-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-013-1224-y