Abstract
Purpose
To assess the effect of transcutaneous electrical nerve stimulation (TENS) for treating refractory overactive bladder syndrome (OAB).
Patients and methods
A consecutive series of 42 patients treated with TENS for refractory OAB was prospectively investigated at an academic tertiary referral centre. Effects were evaluated using bladder diary for at least 48 h and satisfaction assessment at baseline, after 12 weeks of TENS treatment, and at the last known follow-up. Adverse events related to TENS were also assessed.
Results
Mean age of the 42 patients (25 women, 17 men) was 48 years (range, 18–76). TENS was successful following 12 weeks of treatment in 21 (50 %) patients, and the positive effect was sustained during a mean follow-up of 21 months (range, 6–83 months) in 18 patients. Following 12 weeks of TENS treatment, mean number of voids per 24 h decreased significantly from 15 to 11 (p < 0.001) and mean voided volume increased significantly from 160 to 230 mL (p < 0.001). In addition, TENS completely restored continence in 7 (39 %) of the 18 incontinent patients. Before TENS, all 42 patients were dissatisfied or very dissatisfied; following 12 weeks of TENS treatment, 21 (50 %) patients felt satisfied or very satisfied (p < 0.001). No adverse events related to TENS were noted.
Conclusions
TENS seems to be an effective and safe treatment for refractory OAB warranting randomized, placebo-controlled trials.
Similar content being viewed by others
Introduction
Overactive bladder syndrome (OAB), also known as urgency syndrome or urgency-frequency syndrome, is characterized by urgency, with or without urgency incontinence, usually with frequency and nocturia, and there is no proven infection or obvious pathology [1]. OAB is highly prevalent and affects the lives of millions of people worldwide, i.e. approximately 15 % of women and 10 % of men, increasing with advancing age [2]. OAB has a major impact on quality of life and sexuality [2], and besides the debilitating manifestations for patients, OAB also imposes substantial economic burden on every healthcare system, as direct annual costs are comparable to those of other chronic diseases such as dementia and diabetes mellitus [3].
Although antimuscarinics are the pharmacological treatment of choice for OAB, the effectiveness is limited. In a recent systematic review and meta-analysis of randomized controlled trials [4], antimuscarinics led to a mean decrease in incontinence episodes of less than one episode per 24 h compared to placebo. In addition, many patients discontinue antimuscarinic treatment due to adverse events [5]. Thus, there is an urgent need for effective, well-tolerated therapeutic alternatives. Transcutaneous electrical nerve stimulation (TENS) is an established treatment for OAB in children [6, 7] and may also be a valuable option in adults. We therefore investigated, in a prospective study, the effect of TENS for treating adult patients with refractory OAB.
Patients and methods
Patients
A consecutive series of 42 patients who underwent TENS for refractory non-neurogenic OAB was prospectively evaluated. All patients had a complete urological evaluation before considering study enrolment including medical history, satisfaction assessment, physical examination, bladder diary for at least 48 h, urinalysis, urine culture, urethrocystoscopy, bladder washing cytology, and urodynamic investigation. Study inclusion criteria were non-neurogenic OAB with urodynamically proven detrusor overactivity, failed behavioural treatment and pharmacotherapy with at least 2 antimuscarinics, each for a minimum of 1 month and titrated to the maximum dose, no previous surgery for OAB, and no urodynamic signs of bladder outlet obstruction.
The study was performed in accordance with the ethical standards expressed in the Declaration of Helsinki. Before study inclusion, all patients were thoroughly informed, and informed consent was obtained. Urodynamic studies were performed according to Good Urodynamic Practices [8]. All methods, definitions and units conform to the standards recommended by the International Continence Society [1].
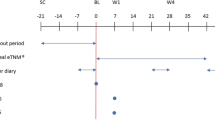
TENS treatment and follow-up assessment
Transcutaneous electrical nerve stimulation was performed at home with an Alpha 4 Conti (Danmeter A/S, 5000 Odense C, Danmark) stimulation device applying Periform® + vaginal electrodes (Mobilis Healthcare Group, Lancashire, UK) in women and PEN2 penile electrodes (Sugar International, Chevillon-sur-Huillard, France) in men (Fig. 1). Bipolar stimulation with 8 Hz and 400 μs at sensory threshold level was used for 20 min twice a day.
Effects of TENS treatment were evaluated by bladder diary for at least 48 h and by satisfaction assessment (i.e. very satisfied, satisfied/undecided/dissatisfied, very dissatisfied). In analogy to the sacral neuromodulation (SNM) literature [9, 10], success of TENS was defined as an improvement of more than 50 % in bladder diary variables (i.e. number of voids, voided volume, and number of leakages: at least 2 of these 3 variables had to have improved for considering a treatment success). After 12 weeks of treatment, TENS was discontinued in all patients and restarted (20 min twice a day) on patient’s request in the case that OAB symptoms recurred.
Outcome measures
Primary outcome measures were changes in the bladder diary and in the satisfaction assessment at baseline and after 12 weeks of treatment.
Secondary outcome measures were changes in the bladder diary and in the satisfaction assessment in patients with successful TENS at the last known follow-up.
Tertiary outcome measures were adverse events during TENS.
Statistical analysis
Data distribution was tested by Q–Q plots. Data were approximately normally distributed and are shown as the mean ± standard deviation (SD). For a calculated sample size of 41 patients, the study was designed to have 80 % power (β = 0.2) for the paired t-test to detect a difference of 2 voiding episodes and a difference of 50 mL in voided volume (these differences were estimated to be clinically relevant) before TENS versus during TENS at a 2-sided significance level of 2.5 % (α = 0.025), assuming a standard deviation (SD) of about two times the detectable difference. The paired t-test and the McNemar’s test were used to compare related samples, respectively. Comparing unrelated samples, the unpaired t-test was applied. Statistical analyses were performed using IBM® SPSS® Statistics version 19.
Results
Baseline characteristics of the 42 patients (25 women, 17 men) treated with TENS for refractory non-neurogenic OAB are shown in Table 1.
Transcutaneous electrical nerve stimulation was successful following 12 weeks of treatment in 21 (50 %) of the 42 patients. The positive TENS effect was sustained during a mean follow-up of 21 months (SD ± 22; range, 6–83 months) in 18 (86 %) of the 21 patients. At the last known follow-up, 4 of the successfully treated patients were still under TENS; the 14 remaining had a sustained effect without treatment.
Following 12 weeks of TENS treatment, mean number of voids per 24 h decreased significantly (p < 0.001) from 15 (SD ± 3.6; range, 9–26) to 11 (SD ± 4.8; range, 5–26) and mean voided volume increased significantly (p < 0.001) from 160 mL (SD ± 50; range, 90–300) to 230 mL (SD ± 85; range, 90–370). In addition, 18 (43 %) of the 42 patients were incontinent before TENS. Following 12 weeks of TENS treatment, continence was completely restored in 7 (39 %) of the 18 incontinent patients, and the mean number of pads used per 24 h decreased significantly (p = 0.001) from 3 (SD ± 1.4; range, 1–6) to 1 (SD ± 1.7; range, 0–7).
Patients’ satisfaction with the lower urinary tract function changed significantly, following TENS treatment (p < 0.001). Before TENS, all 42 patients were dissatisfied or very dissatisfied. Following 12 weeks of TENS treatment, 21 (50 %) patients felt satisfied or very satisfied.
In a subgroup analysis assessing potential gender impact, no significant differences (p > 0.1) between female and male patients were found.
No adverse events related to TENS occurred during the study period.
Discussion
Main findings
In patients with refractory non-neurogenic OAB, TENS was successful following a 12-week treatment period in 50 % of the patients, and of these, the positive effect was sustained in more than 80 %. Importantly, no adverse events related to TENS occurred during the study period. Thus, our findings indicate that TENS may be effective and safe for treating patients with refractory OAB. However, randomized controlled trials are lacking and are highly warranted.
Findings in the context of existing evidence
Neuromodulation, both non-invasive and invasive, has become a well-established and widely accepted treatment in recent years for patients with OAB. Although the exact mechanism of action remains to be elucidated, it seems to involve modulation of spinal cord reflexes and brain networks by peripheral afferents [11]. Dorsal clitoral nerve stimulation during bladder filling reduced the activation of certain cortical areas suggesting a neuromodulatory effect on supraspinal centres involved in lower urinary tract control [12]. In addition, plastic reorganization of cortical networks triggered by peripheral neuromodulation has been hypothesized [13]. In a PET study of patients treated by SNM for urgency incontinence [14], the authors proposed that acute neuromodulation predominantly involves areas associated with sensorimotor learning, which might become progressively less active during the course of chronic neuromodulation. Moreover, the sympathetic nervous system might play a role as indicated by studies of low-frequency pudendal nerve stimulation in cats with chronic spinal cord injury [15].
Percutaneous tibial nerve stimulation (PTNS) has been shown to be an effective treatment for non-neurogenic OAB in randomized, double-blind, placebo-controlled trials [16, 17]. In patients with refractory OAB, SNM was found to have clear benefits for carefully selected patients, but many adverse events were reported and redo surgery was often necessary [18–20]. Pudendal neuromodulation has emerged as an alternative to SNM, considering a randomized crossover study reporting that stimulation of the pudendal nerve may be more effective than SNM for modulating bladder activity [21]. Since the pudendal nerves innervate many areas in the pelvic region including vagina, penis, anal and urethral sphincters, and the perineal skin, it is possible to stimulate these pudendal nerve branches non-invasively [22]. Previous animal studies have shown that vaginal [23] and penile stimulation [24] can inhibit bladder activity and prevent incontinence what is in line with the findings of the present study in humans. Thus, regarding the non-invasiveness, easy application, and excellent safety profile, TENS may become a valuable treatment option for refractory OAB before more invasive methods such as PTNS, intradetrusor botulinum-A-toxin injections or SNM are considered.
Implications for research
Considering the promising findings of the present study, further investigations are warranted. Randomized controlled trials are necessary to demonstrate the efficacy of TENS in treating OAB. In such prospective trials, both non-neurogenic and neurogenic OAB, validated disease- and condition-specific quality of life data, short-, medium- and long-term results as well as cost-effectiveness issues should be assessed, and outcomes should be reported with the Consolidated Standards of Reporting Trials statement [25]. Moreover, it would be interesting to directly compare TENS and PTNS. At a glance, PTNS seems to be more effective than TENS, considering the reported PTNS success rates of 55–71 % [16, 17]. However, taking into account the different inclusion criteria, the results are not comparable. The feasibility of TENS, which can be easily used at home by the patient, represents a real advantage compared to PTNS, which requires the insertion of a needle close to the tibial nerve. Furthermore, the genital nerves are in more proximity to the sacral plexus than the tibial nerve, and this may, at least from a theoretical viewpoint, have an effect on treatment efficacy. In addition, stimulation parameters need further investigation. Although the TENS device that applied in the present study allows a wide range of different stimulation settings, we preset the parameters and did them not adjust to each patient for homogeneity reasons. However, individual adjustment of the stimulation parameters in analogy to SNM may improve the response rate and warrants additional studies. There is also unclear whether a maintenance-therapy is needed or not. Indeed, treatment standardization is lacking, and there are no guidelines for therapeutic and maintenance regimens.
Implications for practice
Overactive bladder syndrome is a widespread chronic illness that has a major impact on quality of life, affecting emotional, social, sexual, occupational, and physical aspects of daily life [26]. Besides the debilitating manifestations for patients, it also imposes substantial economic burden for every healthcare system [3]. First-line treatment for OAB includes antimuscarinics, but the treatment effect is often unsatisfactory, so that other options have to be considered, including the yet unlicensed intradetrusor botulinum-A-toxin injections, SNM, or even more invasive procedures such as bladder augmentation or urinary diversion. Thus, easy, non-invasive, widely available, effective, and well-tolerated therapeutic alternatives are highly desirable. Considering the findings of the present study, TENS may become such a treatment option, especially taking into account that we only included patients with refractory OAB, i.e. all our patients had undergone multiple failed previous treatments (negative patient selection). In the case that our findings are confirmed in randomized trials, this would have major implications for daily practice since TENS would have to be propagated widely and implemented quickly as a standard OAB treatment.
Limitations
The present study has several limitations. First, the results are based on a non-randomized study without a control group. Thus, we are not able to differentiate between the real TENS effect and the placebo effect. From a patient’s viewpoint, however, it is most important that a treatment helps, independent of a potential placebo effect. Second, we did not assess patients’ quality of life using a validated OAB-specific questionnaire. Third, including only patients with refractory non-neurogenic OAB may induce a negative selection bias. Indeed, the TENS effect may be underestimated in the present study and is probably more pronounced in patients with treatment-naive OAB. Moreover, it is unclear whether our results in non-neurological patients could be extrapolated to patients with neurogenic OAB, although promising results of transcutaneous posterior tibial nerve stimulation for treating OAB in multiple sclerosis patients have been found [27]. Fourth, the duration of the bladder diary may have influenced our results, i.e. a bladder diary of more than at least 2 days may result in more reliable data regarding patients’ symptoms. However, it should be considered that patient compliance decreases with longer diary duration and that, despite recent attempts [28], there is no validated generally accepted bladder diary currently available [29].
Despite the addressed limitations, the present study was prospective with predefined outcome criteria, and it was adequately powered and sized to detect differences before versus during TENS treatment. In addition, the 42 evaluated patients with refractory non-neurogenic OAB with a mean follow-up of 21 months in the case of successful TENS treatment seem not insignificant, considering the lack of data published to date and taking into account the debilitating manifestations of OAB.
Conclusions
In patients with refractory non-neurogenic OAB, TENS was successful following a 12-week treatment period in 50 % of the patients, and of these, the positive effect was sustained in more than 80 % during a mean follow-up of 21 months. Importantly, no adverse events related to TENS occurred during the study period. Thus, TENS seems to be an effective and safe treatment for refractory OAB warranting randomized, placebo-controlled trials.
References
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, van Kerrebroeck P, Victor A, Wein A (2002) The standardisation of terminology of lower urinary tract function: report from the standardisation sub-committee of the international continence society. Neurourol Urodyn 21:167–178
Temml C, Heidler S, Ponholzer A, Madersbacher S (2005) Prevalence of the overactive bladder syndrome by applying the international continence society definition. Eur Urol 48:622–627
Klotz T, Bruggenjurgen B, Burkart M, Resch A (2007) The economic costs of overactive bladder in Germany. Eur Urol 51:1654–1662; discussion 1662–1663
Chapple CR, Khullar V, Gabriel Z, Muston D, Bitoun CE, Weinstein D (2008) The effects of antimuscarinic treatments in overactive bladder: an update of a systematic review and meta-analysis. Eur Urol 54:543–562
Kelleher CJ, Cardozo LD, Khullar V, Salvatore S (1997) A medium-term analysis of the subjective efficacy of treatment for women with detrusor instability and low bladder compliance. Br J Obstet Gynaecol 104:988–993
Hagstroem S, Mahler B, Madsen B, Djurhuus JC, Rittig S (2009) Transcutaneous electrical nerve stimulation for refractory daytime urinary urge incontinence. J Urol 182:2072–2078
Lordelo P, Teles A, Veiga ML, Correia LC, Barroso U Jr (2010) Transcutaneous electrical nerve stimulation in children with overactive bladder: a randomized clinical trial. J Urol 184:683–689
Schafer W, Abrams P, Liao L, Mattiasson A, Pesce F, Spangberg A, Sterling AM, Zinner NR, van Kerrebroeck P (2002) Good urodynamic practices: uroflowmetry, filling cystometry, and pressure-flow studies. Neurourol Urodyn 21:261–274
Kessler TM, Buchser E, Meyer S, Engeler DS, Al-Khodairy AW, Bersch U, Iselin CE, Roche B, Schmid DM, Schurch B, Zrehen S, Burkhard FC (2007) Sacral neuromodulation for refractory lower urinary tract dysfunction: results of a nationwide registry in Switzerland. Eur Urol 51:1357–1363
van Kerrebroeck PE, van Voskuilen AC, Heesakkers JP, Lycklama a Nijholt AA, Siegel S, Jonas U, Fowler CJ, Fall M, Gajewski JB, Hassouna MM, Cappellano F, Elhilali MM, Milam DF, Das AK, Dijkema HE, van den Hombergh U (2007) Results of sacral neuromodulation therapy for urinary voiding dysfunction: outcomes of a prospective, worldwide clinical study. J Urol 178:2029–2034
Kessler TM, Fowler CJ (2008) Sacral neuromodulation for urinary retention. Nat Clin Pract Urol 5:657–666
Mehnert U, Boy S, Svensson J, Michels L, Reitz A, Candia V, Kleiser R, Kollias S, Schurch B (2008) Brain activation in response to bladder filling and simultaneous stimulation of the dorsal clitoral nerve–an fMRI study in healthy women. Neuroimage 41:682–689
Finazzi-Agro E, Rocchi C, Pachatz C, Petta F, Spera E, Mori F, Sciobica F, Marfia GA (2009) Percutaneous tibial nerve stimulation produces effects on brain activity: study on the modifications of the long latency somatosensory evoked potentials. Neurourol Urodyn 28:320–324
Blok BF, Groen J, Bosch JL, Veltman DJ, Lammertsma AA (2006) Different brain effects during chronic and acute sacral neuromodulation in urge incontinent patients with implanted neurostimulators. BJU Int 98:1238–1243
Tai C, Smerin SE, de Groat WC, Roppolo JR (2006) Pudendal-to-bladder reflex in chronic spinal-cord-injured cats. Exp Neurol 197:225–234
Peters KM, Carrico DJ, Perez-Marrero RA, Khan AU, Wooldridge LS, Davis GL, Macdiarmid SA (2010) Randomized trial of percutaneous tibial nerve stimulation versus sham efficacy in the treatment of overactive bladder syndrome: results from the SUmiT trial. J Urol 183:1438–1443
Finazzi-Agro E, Petta F, Sciobica F, Pasqualetti P, Musco S, Bove P (2010) Percutaneous tibial nerve stimulation effects on detrusor overactivity incontinence are not due to a placebo effect: a randomized, double-blind, placebo controlled trial. J Urol 184:2001–2006
Brazzelli M, Murray A, Fraser C (2006) Efficacy and safety of sacral nerve stimulation for urinary urge incontinence: a systematic review. J Urol 175:835–841
Herbison GP, Arnold EP (2009) Sacral neuromodulation with implanted devices for urinary storage and voiding dysfunction in adults. Cochrane Database Syst Rev CD004202
Siddiqui NY, Wu JM, Amundsen CL (2010) Efficacy and adverse events of sacral nerve stimulation for overactive bladder: a systematic review. Neurourol Urodyn 29(suppl 1):S18–S23
Peters KM, Feber KM, Bennett RC (2005) Sacral versus pudendal nerve stimulation for voiding dysfunction: a prospective, single-blinded, randomized, crossover trial. Neurourol Urodyn 24:643–647
Shen B, Roppolo JR, Subbaroyan J, Diubaldi A, Wahlgren S, de Groat WC, Tai C (2011) Neuromodulation of bladder activity by stimulation of feline pudendal nerve using a transdermal amplitude modulated signal (TAMS). Neurourol Urodyn 30:1686–1694
Lindstrom S, Fall M, Carlsson CA, Erlandson BE (1983) The neurophysiological basis of bladder inhibition in response to intravaginal electrical stimulation. J Urol 129:405–410
Woock JP, Yoo PB, Grill WM (2008) Activation and inhibition of the micturition reflex by penile afferents in the cat. Am J Physiol Regul Integr Comp Physiol 294:R1880–R1889
Moher D, Schulz KF, Altman DG (2001) The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomised trials. Lancet 357:1191–1194
Abrams P, Kelleher CJ, Kerr LA, Rogers RG (2000) Overactive bladder significantly affects quality of life. Am J Manag Care 6:S580–S590
de Seze M, Raibaut P, Gallien P, Even-Schneider A, Denys P, Bonniaud V, Game X, Amarenco G (2011) Transcutaneous posterior tibial nerve stimulation for treatment of the overactive bladder syndrome in multiple sclerosis: results of a multicenter prospective study. Neurourol Urodyn 30:306–311
Bright E, Cotterill N, Drake M, Abrams P (2012) Developing a validated urinary diary: phase 1. Neurourol Urodyn. doi:10.1002/nau.21254
Bright E, Drake MJ, Abrams P (2011) Urinary diaries: evidence for the development and validation of diary content, format, and duration. Neurourol Urodyn 30:348–352
Conflict of interest
None of the contributing authors has a conflict of interest in relation to this article.
Author information
Authors and Affiliations
Corresponding author
Additional information
Marc Tellenbach and Marc Schneider have equal study contribution, i.e. shared first authorship.
Clinical trial registration: ACTRN12611000445976.
Rights and permissions
About this article
Cite this article
Tellenbach, M., Schneider, M., Mordasini, L. et al. Transcutaneous electrical nerve stimulation: an effective treatment for refractory non-neurogenic overactive bladder syndrome?. World J Urol 31, 1205–1210 (2013). https://doi.org/10.1007/s00345-012-0888-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-012-0888-z