Abstract
Background
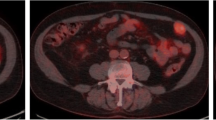
CT imaging is widely used for response evaluation of immunotherapy in patients with advanced stage renal cell carcinoma (RCC). However, this kind of treatment may not immediately be cytoreductive, although the treatment is successful. This poses new demands on imaging modalities. Positron emission tomography (PET) using 18F-fluorodeoxyglucose (FDG) proved to be useful in monitoring the effect of several antitumour treatments. We investigated the potential of FDG-PET for the evaluation of response to immunotherapy.
Methods
In seven patients with metastasized RCC, who were treated with either interferon-alpha (IFN-α) monotherapy or a combination of IFN-α, interleukin-2 and 5-fluorouracil, FDG-PET was performed prior and after 5 and 9 weeks of treatment. Quantitative changes of glucose metabolic rate (MRGlu) were compared with changes in tumour size on CT imaging using Response Evaluation Criteria in Solid Tumors (RECIST) and to survival and progression-free survival.
Results
No consistent changes in MRGlu were observed within different response groups. And no correlation with CT imaging, neither with survival or progression-free survival, was found.
Conclusion
In contrast to the positive results reported on (chemo) therapy response evaluation with FDG-PET in different malignancies, this imaging modality appears not useful in response monitoring of immunotherapeutic modalities in RCC.
Similar content being viewed by others
Introduction
Renal cell carcinoma (RCC) is a relative rare tumour type. It accounts for 2.1% of all malignancies and is responsible for 1.5% of all cancer deaths worldwide [1]. Almost 25% of patients have metastatic disease at presentation, and 30–40% of patients that initially present with localized disease, develop metastases during the course of their disease [2]. At that stage, patients cannot longer be cured, and 5-year survival rates do not reach 5% [3]. Since chemotherapeutic and hormonal agents appeared to be of limited benefit, different treatment strategies have been developed [4]. One frequently used strategy is immunotherapy with interferon-alpha (IFN-α) or combination therapy with IFN-α and interleukin-2 (IL-2) together with the biological agent 5-fluorouracil (5-FU).
Response assessment for these therapies has traditionally been made by anatomical imaging modalities, such as CT, using the Response Evaluation Criteria in Solid Tumors (RECIST) [5]. These treatments, however, are rather cytostatic than cytoreductive, in which case successful treatment may not lead to a decrease in tumour size. An unchanged residual mass does not necessarily imply poor therapeutic response. This makes anatomical imaging less suitable for monitoring the effect of treatment strategies. Furthermore, differentiation between vital tumour and fibrosis or necrosis is difficult using morphological imaging. Therefore, functional imaging techniques to monitor response to therapy may be an attractive alternative to morphological imaging. Positron emission tomography (PET) with 18fluorodeoxyglucose (FDG) is an imaging modality, which has already an established role for many indications in clinical oncology [6, 7]. With PET, using the fluoride-18-labelled glucose analogue FDG, tissue with a high-glucose metabolic rate is visualized, which is useful for initial diagnosis or staging. Furthermore, quantification and measurement of therapy-induced changes in glucose metabolism is possible with PET as well.
Earlier studies on FDG-PET for evaluation of malignant lymphoma after chemotherapy show that FDG-PET was superior to CT in predicting progression-free survival [8, 9]. Similar results were found in recent studies in patients with non-small cell lung cancer and colorectal cancer in which chemotherapeutic response was evaluated with FDG-PET [10, 11].
Furthermore, FDG-PET has also shown to be useful in monitoring the response to targeted therapy in various malignancies as for instance malignant gastrointestinal stromal tumours [12]. Concerning immunotherapy, promising results have been obtained from recent studies on response evaluation with FDG-PET in patients with non-Hodgkin lymphoma with suggestion of superiority to CT as well [13, 14].
In this study, we investigated whether FDG-PET is a useful modality for monitoring therapeutic response and for predicting outcome in terms of survival and progression-free survival in patients who were treated by either IFN-α monotherapy or triple therapy with IFN-α, IL-2 and 5-FU. Quantitative FDG-PET analysis using glucose metabolic rate (MRGlu) was compared with conventional CT imaging using RECIST. Survival and progression-free survival served as the standard of reference.
Materials and methods
Patients
The present study was carried out as part of a large multicenter protocol that studied the therapeutic effect of IFN-α, IL-2, 5-FU triple therapy compared with IFN-α-monotherapy on advanced stages of RCC. All patients considered eligible for this multicenter trial (Table 1) were asked to participate in this side study. An exclusion criterion for the side study was diabetes mellitus. Patients participating in the multicenter trial were randomized for treatment with IFN-α monotherapy or triple therapy including IFN-α, IL-2 and 5-FU.
FDG-PET
FDG-PET was performed prior to treatment and respectively after 5 and 9 weeks for response evaluation (Table 2). Patients were fasted for at least six hours prior to injection of 200 MBq 18F-FDG. FDG-PET was performed on an ECAT-EXACT47 PET scanner (Siemens/CTI, Knoxville, TN, USA). Patients were positioned supine. The dynamic data acquisition was started simultaneously with the injection of FDG.
Tumour time-activity curves
Tumour time-activity curves were obtained by placing volumes of interest (VOIs) semi-automatically over the tumour and metastases using a threshold of 50% of the maximum pixel value within the lesion. The locations of the lesions were evaluated visually on the transaxial, coronal and sagittal images. For this purpose, the late frames (frame 14–16) were summed, yielding a static image of 30 min and a scan mid-time of 35 min post-injection. The tumour VOIs were then copied to all dynamic time frames to obtain time–activity curves. A volume-weighted mean value of all lesions in each PET scan was derived to provide one MRGlu for each study.
Image-derived input function
The image-based input functions were determined by measuring FDG counts in VOIs over the ascending aorta or abdominal aorta, depending on the body location of the study. An early time frame (frame 3, i.e., 60–90 s post-injection) was used, in which the bolus of activity was best visualized, and time-activity curves were created using VOIs that consisted of several regions of interest drawn over the blood pool area in as many planes as possible. For VOI definition, a semi-automatic threshold-based region-growing programme was used. All VOIs were confirmed visually [15].
Patlak graphical analyses
For quantitative measurement of glucose metabolism, Patlak graphical analysis was used to calculate the MRGlu (expressed in μmol ml−1 min−1) in tumour tissue [16]. The Patlak approach takes into account differences in the whole-body distribution of FDG at the time of scanning, which may affect the accumulation of FDG in the tumour tissue. Therefore, the MRGlu is in principle a more reliable measure of tumour glucose use than the standardized uptake value (SUV). Patlak graphical analysis is based on the assumption that the ratio of the tracer concentration in tissue to that in plasma increases linearly when plotted as a function of normalized time. This linear relationship follows directly from the FDG model when the free tissue FDG concentration is constant and unidirectional transport, i.e., trapping of FDG can be assumed. This assumption in practice occurs about 5 min post-injection. The Patlak analysis was performed over the period from 5 to 50 min after injection. Furthermore, the MRGlu (expressed in μmol ml−1 min−1) in tumour was calculated by multiplication of the slope of the Patlak-plot (K1k3.(k2 + k3)−1) and the basic blood glucose level (expressed in μmol ml−1), measured before FDG injection (hexokinase method, Aeroset, Abbott diagnostics, Illinois, USA). In this study the lumped constant used was set to 1 and was assumed to be constant over time, because no studies on the actual value of the lumped constant in tumours outside the central nervous system have been reported yet.
Patient evaluation and follow-up
The first response evaluation PET was performed after five weeks when immunotherapy with IL-2 in the triple-therapy-group was completed and therapy with 5-FU was not yet started. Furthermore, patients treated with IFN-α monotherapy were maximally boosted at that time. The second evaluation at nine weeks was chosen because of the concurrent CT evaluation at that time-point, in order to obtain more comparable results. Data derived from the Patlak analysis were compared with those from CT-response evaluation based on RECIST guidelines [5].
Clinical follow-up took place at 9, 19 and 26 weeks, at 8, 10 and 12 months, subsequently every 4 months for 1 year and every 6 months thereafter. In this follow-up period, CT was used to determine response. The median follow-up period was 37.5 months (range 22–47 months).
Progression-free survival was defined as the duration of response/stable disease as determined by CT, starting from the day on which the baseline PET was performed. Overall survival was defined as the time from baseline PET until death.
Statistical considerations
When designing the study, a power analysis was performed to estimate the required size of the patient population. Data from the literature suggest that 15% of patients show response on immunotherapy and 30% of patients show stable disease according to RECIST [17]. Conventional imaging, however, often underestimates immunotherapy treatment response. Thus, to detect 20% more treatment responses using FDG-PET, a sample size of 15 patients is required (alpha 0.05, power 0.80, McNemar test, two-sided), assuming that PET does not underestimate therapy response.
An agreement was made to perform an interim analysis halfway the study and to discontinue if the interim analysis would not show an association between metabolic and morphologic response assessment or (progression-free) survival.
Results
FDG-PET was performed in 7 patients with metastatic RCC. All patients were nephrectomized (6 men, 1 woman; mean age 59 years; range, 49–66 years) and had histologically confirmed RCC, all of the clear cell type. Four patients already had metastatic disease at initial diagnosis. Metastases were located in the lung, lymph nodes and adrenal gland. The median follow-up period was 37.5 months (range, 22–47 months).
Two patients received triple therapy, and five were treated with IFN-α monotherapy. According to CT, performed 9 weeks after starting therapy, one patient had partial response, four had stable disease, and two had progressive disease. Complete remission was not observed. The median progression-free survival after starting immunotherapy was 9 months (range, 3–37 months). Four patients died, all within 40 months after initial diagnosis.
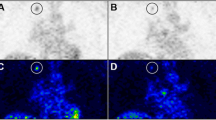
The average glucose metabolic rate measured at baseline was 0.0665 μmol/ml/min (range, 0.0365–0.1028). There was a large variation of glucose metabolic rate within the group of patients. No association between metabolic and morphologic response, progression-free survival and overall survival was found at interim analysis (Fig. 1), which resulted in a discontinuation of the study.
Metabolic rate of glucose of each response group, measured at baseline (MRGlu1) and after 5 and 9 weeks of treatment (MRGlu2 and MRGlu3 respectively). Therapy consisted of either IFN-α (straight line) or triple therapy (dashed line). Response groups were defined as partial response (a), stable disease (b) and progressive disease (c) according to RECIST on CT findings. No association between glucose metabolic rate and response to therapy, as established by CT, and progression-free survival (PFS) and overall survival (OS) was found
Discussion
At present, response monitoring of antitumour treatments with FDG-PET is still in its infancy. Not for all kinds of antitumour treatment it is elucidated whether FDG-PET is capable of predicting response and whether FDG-PET shows added value in response evaluation of a certain treatment. The present study, however, could not confirm the utility of FDG-PET-based response evaluation of immunotherapy in patients with metastatic RCC.
In the present study, the variable metabolic response pattern on immunotherapy without correlation to morphological response and overall survival or progression-free survival may be explained by some biological features of RCC tumour cells and by the effect of immunotherapy on these biological features. One could speculate, on the possible effects on glucose metabolism of the hypoxia inducible factor 1α (HIF-1α), activated T cells and the expression of c-myc in RCC.
The latter one is a proto-oncogene that regulates cell proliferation, cell growth and apoptosis. Evidence for over-expression in c-myc in most cases of RCC has been found and is correlated with T status, nuclear grade and venous invasion. However, the expression of c-myc, which variates within patients with RCC, is not correlated with clinical parameters such as nodal or distant metastasis, tumour type and neither is an independent predictor of survival [18]; consequently, IFN-α is not equally effective in each patient.
It is known that c-myc enhances glucose metabolism [19]. In case of such a straightforward relation, one would expect some correlation between (progression-free) survival, morphological response and the degree of MRGlu prior to therapy. However, this was not seen in the present study. This suggests more unknown mechanisms that interfere with glucose metabolism as for instance HIF-1α over-expression which is associated with loss of functional Von Hippel-Lindau (VHL) gene which occurs in approximately 70% of clear cell RCCs [20]. HIF-1α over-expression in RCC is also associated with high GLUT-1 expression [21].
Furthermore, in the two patients who were treated with triple therapy, activation of T cells by IL-2 could also have contributed to an enhancement of glucose metabolism after therapy as well. In this case, an increment in MRGlu due to inflammatory reaction could mask a true therapeutic effect.
On staging of RCC and in the preoperative diagnostic work-up, far more studies concerning the role of FDG-PET have been published. For instance, Kang and colleges investigated a group of 66 patients with renal cell carcinoma. Although the specificity of FDG-PET was 100%, which was superior to CT, sensitivity was low for both primary and metastatic lesions (60 and 77%, respectively) due to variation in FDG avidity of these tumours [22].
It remains unclear why FDG uptake (glucose metabolism) varies among patients with RCC. In some malignancies, FDG uptake is correlated with glucose transporter protein 1 (GLUT-1) expression [23, 24]. No evidence for such a correlation in RCC, however, has been found [25]. In our group of patients with metastasis who had resection of the primary tumour, glucose metabolic rate prior to immunotherapy varied widely as well.
Finally, there are more radiopharmaceuticals for PET beyond FDG. The goal of more targeted, individualized therapies probably needs more specific, biologically directed imaging, a role for which PET is ideally suited. Future applications of PET for therapy response assessment will likely involve other tracers in addition to FDG, to better characterize tumour biology and more effectively measure response to antitumour therapy, such as immunotherapy. New PET tracers for imaging RCC, like 18F-fluoromisonidazole (18F-FMISO), 11C-acetate and 89Zr-labelled cG250 monoclonal antibody already have been investigated with promising results [26–28]. However, these studies all focussed on staging and on imaging the primary RCC prior to therapy.
Conclusion
In contrast to the positive results reported on (chemo) therapy response evaluation in a wide variety of malignancies, FDG-PET seems not to be useful for response monitoring of immunotherapeutic modalities in RCC.
References
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM (2010) Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 127(12):2893–2917. doi:10.1002/ijc.25516
Rabinovitch RA, Zelefsky MJ, Gaynor JJ, Fuks Z (1994) Patterns of failure following surgical resection of renal cell carcinoma: implications for adjuvant local and systemic therapy. J Clin Oncol 12(1):206–212
Lawrentschuk N, Davis ID, Bolton DM, Scott AM (2006) Positron emission tomography (PET), immuno-PET and radioimmunotherapy in renal cell carcinoma: a developing diagnostic and therapeutic relationship. BJU Int 97(5):916–922. doi:10.111/j.1464-410x.2006.06125.x
Vugrin D (1987) Systemic therapy of metastatic renal cell carcinoma. Semin Nephrol 7(2):152–162
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, Gwyther SG (2000) New guidelines to evaluate the response to treatment in solid tumours. European organization for research and treatment of cancer, national cancer institute of the United States, national cancer institute of Canada. J Natl Cancer Inst 92(3):205–221
Delbeke D (1999) Oncological applications of FDG PET imaging: brain tumours, colorectal cancer, lymphoma and melanoma. J Nucl Med 40(4):591–603
Rigo P, Paulus P, Kaschten BJ, Hustinx R, Bury T, Jerusalem G, Benoit T, Foidart-Willems J (1996) Oncological applications of positron emission tomography with fluorine-18 fluorodeoxyglucose. Eur J Nucl Med 23(12):1641–1674
Guay C, Lepine M, Verreault J, Benard F (2003) Prognostic value of PET using 18F-FDG in Hodgkin’s disease for posttreatment evaluation. J Nucl Med 44(8):1223–1225
Filmont JE, Czernin J, Yap C, Silverman DH, Quon A, Phelps ME, Emmanouilides C (2003) Value of F-18 fluorodeoxyglucose positron emission tomography for predicting the clinical outcome of patients with aggressive lymphoma prior to and after autologous stem-cell transplantation. Chest 124(2):608–613
de Geus-Oei LF, van Laarhoven HW, Visser EP, Hermsen R, van Hoorn BA, Kamm YJ, Krabbe PF, Corstens FH, Punt CJ, Oyen WJ (2008) Chemotherapy response evaluation with FDG PET in patients with colorectal cancer. Ann Oncol 19(2):348–352. doi:10.1093/annonc/mdm470
Dimitrakopoulou-Strauss A, Hoffmann M, Bergner R, Uppenkamp M, Eisenhut M, Pan L, Haberkorn U, Strauss LG (2007) Prediction of short-term survival in patients with advanced nonsmall cell lung cancer following chemotherapy based on 2-deoxy-2-[F-18]fluoro-d-glucose-positron emission tomography: a feasibility study. Mol Imaging Biol 9(5):308–317. doi:10.1007/s11307-607-0103-6
Gayed I, Vu T, Iyer R, Johnson M, Macapinlac H, Swanston N, Podoloff D (2004) The role of 18F-FDG PET in staging and early prediction of response to therapy of recurrent gastrointestinal stromal tumours. J Nucl Med 45(1):17–21
Chaise C, Itti E, Petegnief Y, Wirquin E, Copie-Bergman C, Farcet JP, fau-Larue MH, Meignan M, Talbot JN, Molinier-Frenkel V (2007) [F-18]-Fluoro-2-deoxy-d-glucose positron emission tomography as a tool for early detection of immunotherapy response in a murine B cell lymphoma model. Cancer Immunol Immunother 56(8):1163–1171. doi:10.1007/s00262-006-0265-0
Torizuka T, Zasadny KR, Kison PV, Rommelfanger SG, Kaminski MS, Wahl RL (2000) Metabolic response of non-Hodgkin’s lymphoma to 131I-anti-B1 radioimmunotherapy: evaluation with FDG PET. J Nucl Med 41(6):999–1005
de Geus-Oei LF, Visser EP, Krabbe PF, van Hoorn BA, Koenders EB, Willemsen AT, Pruim J, Corstens FH, Oyen WJ (2006) Comparison of image-derived and arterial input functions for estimating the rate of glucose metabolism in therapy-monitoring 18F-FDG PET studies. J Nucl Med 47(6):945–949
Patlak CS, Blasberg RG, Fenstermacher JD (1983) Graphical evaluation of blood-to-brain transfer constants from multiple-time uptake data. J Cereb Blood Flow Metab 3(1):1–7
van Herpen CM, Jansen RL, Kruit WH, Hoekman K, Groenewegen G, Osanto S, De Mulder PH (2000) Immunochemotherapy with interleukin-2, interferon-alpha and 5-fluorouracil for progressive metastatic renal cell carcinoma: a multicenter phase II study. Dutch immunotherapy working party. Br J Cancer 82(4):772–776. doi:10.1054/bjoc.1999.0997
Lanigan D, McLean PA, Murphy DM, Donovan MG, Curran B, Leader M (1993) c-myc expression in renal carcinoma: correlation with clinical parameters. Br J Urol 72(2):143–147
Osthus RC, Shim H, Kim S, Li Q, Reddy R, Mukherjee M, Xu Y, Wonsey D, Lee LA, Dang CV (2000) Deregulation of glucose transporter 1 and glycolytic gene expression by c-Myc. J Biol Chem 275(29):21797–21800. doi:10.1074/bjc.c000023200
Kenck C, Wilhelm M, Bugert P, Staehler G, Kovacs G (1996) Mutation of the VHL gene is associated exclusively with the development of non-papillary renal cell carcinomas. J Pathol 179(2):157–161. doi:10.1002/(SICI)1096-9896(199606)179:2<157:AID-PATH557>3.0.CO;2-S
Lidgren A, Bergh A, Grankvist K, Rasmuson T, Ljungberg B (2008) Glucose transporter-1 expression in renal cell carcinoma and its correlation with hypoxia inducible factor-1 alpha. BJU Int 101(4):480–484. doi:10.1111/j.1464-410X.2007.07238.x
Kang DE, White RL Jr, Zuger JH, Sasser HC, Teigland CM (2004) Clinical use of fluorodeoxyglucose F 18 positron emission tomography for detection of renal cell carcinoma. J Urol 171(5):1806–1809. doi:10.1097/01.ju.0000120241.50061.e4
Tateishi U, Yamaguchi U, Seki K, Terauchi T, Arai Y, Hasegawa T (2006) Glut-1 expression and enhanced glucose metabolism are associated with tumour grade in bone and soft tissue sarcomas: a prospective evaluation by [18F]fluorodeoxyglucose positron emission tomography. Eur J Nucl Med Mol Imaging 33(6):683–691. doi:10.1007/s00259-005-0044-8
Chung JK, Lee YJ, Kim SK, Jeong JM, Lee DS, Lee MC (2004) Comparison of [18F]fluorodeoxyglucose uptake with glucose transporter-1 expression and proliferation rate in human glioma and non-small-cell lung cancer. Nucl Med Commun 25(1):11–17. doi:00006231-200401000-00003
Miyakita H, Tokunaga M, Onda H, Usui Y, Kinoshita H, Kawamura N, Yasuda S (2002) Significance of 18F-fluorodeoxyglucose positron emission tomography (FDG-PET) for detection of renal cell carcinoma and immunohistochemical glucose transporter 1 (GLUT-1) expression in the cancer. Int J Urol 9(1):15–18
Lawrentschuk N, Poon AM, Foo SS, Putra LG, Murone C, Davis ID, Bolton DM, Scott AM (2005) Assessing regional hypoxia in human renal tumours using 18F-fluoromisonidazole positron emission tomography. BJU Int 96(4):540–546. doi:10.1111/j.1464-410X.2005.05681.x
Shreve P, Chiao PC, Humes HD, Schwaiger M, Gross MD (1995) Carbon-11-acetate PET imaging in renal disease. J Nucl Med 36(9):1595–1601
Brouwers A, Verel I, van Eerd EJ, Visser G, Steffens M, Oosterwijk E, Corstens F, Oyen W, Van Wylen DG, Boerman O (2004) PET radioimmunoscintigraphy of renal cell cancer using 89Zr-labeled cG250 monoclonal antibody in nude rats. Cancer Biother Radiopharm 19(2):155–163. doi:10.1089/108497804323071922
Conflict of interest
The authors declare that they have no conflict of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Gilles, R., de Geus-Oei, LF., Mulders, P.F.A. et al. Immunotherapy response evaluation with 18F-FDG-PET in patients with advanced stage renal cell carcinoma. World J Urol 31, 841–846 (2013). https://doi.org/10.1007/s00345-011-0723-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-011-0723-y