Abstract
Background
We evaluated 18F-FDG PET/CT in small cell lung cancer (SCLC) staging and assessed metabolic (SUVmax, MTV and TLG) and morphologic (CTvol) variables as predictors for overall survival (OS) and progression-free survival (PFS).
Methods
Patients with newly diagnosed, histopathology-confirmed SCLC, who underwent 18F-FDG PET/CT were evaluated. A Cox proportional hazard model was used to determine the association between the primary tumour SUVmax, MTV, TLG and CTvol with OS and PFS. Similar evaluations were performed when hilar/mediastinal lymphadenopathy was included [total SUVmax (TSUVmax), total MTV (TMTV) and total TLG (TTLG)].
Results
55 patients were included. 18F-FDG PET/CT changed staging in 6/55 (10.9%) patients who were upstaged to extensive disease. TTLG (>443.8) was a significant variable for OS with HR=2.1 (CI 1.14–3.871, p=0.017). Patients with TTLG>443.8 had a median OS of 13.4 months compared to 25.7 months in patients with TTLG<443.8 (p=0.018). TMTV (>72.4) was significant for PFS with HR=2.3 (CI 1.11-4.8, p=0.025). A median PFS of 12.1 and 26.2 months was found with TMTV greater and less than 72.4, respectively (p=0.005).
Conclusions
18F-FDG PET/CT improved staging of patients with SCLC, and TTLG and TMTV can be used as prognostic variables for OS and PFS, respectively.
Key Points
• Identifying variables that predict the prognosis of patients with SCLC is important.
• 18F-FDG PET/CT influences staging of patients with SCLC.
• Metabolic parameters could be used as predictors for PFS and OS.
Similar content being viewed by others
Introduction
Small cell lung cancer (SCLC) represents approximately 14 % of newly diagnosed lung cancer [1] and is usually characterized by a rapid onset of symptoms, a tendency to metastasize early, an initial good response to chemotherapy and radiation and a high association with paraneoplastic syndromes [2]. Staging is based on conventional imaging, including: computed tomography (CT) of the chest and abdomen, bone scintigraphy and magnetic resonance imaging (MRI) of the brain, using the Veterans Administration Lung Study Group (VALSG) classification in which disease is divided into limited disease (LD) whenever tumour volume is confined to one hemithorax and regional lymph nodes that can be included in a single tolerable radiation port or extensive disease (ED). Response to treatment relies on RECIST 1.1 (response evaluation criteria in solid tumours).
The added value of positron emission tomography (PET) regarding the diagnostic accuracy for staging patients with SCLC is uncertain mainly due to research method inconsistencies between different studies; still, most studies have found that PET improved staging accuracy with an impact on patient management. For example, Brink et al. [3] compared the diagnostic accuracy of PET and CT in 120 patients with regard to the primary tumour, lymph node, distant (not brain) metastases and brain and found values of 100 % for both, 99 vs. 83 %, 96 vs. 81 % and 90 vs. 100 %, respectively. PET up-staged and down-staged 10 and 3 patients, respectively, and incorrectly staged 1 patient with brain metastases not clearly seen on PET.
Treatment is based mainly on the extension of disease at presentation but also takes several prognostic markers into consideration, such as the performance status of the patient. In general, patients with limited disease are treated with definitive chemoradiation as the addition of radiation in limited disease improved local control and increased the overall survival (OS) in 5 %. Patients with extensive disease are treated with palliative chemotherapy, sparing the toxicity of definitive chemoradiation and reducing health-care costs associated with radiation planning and delivering. However, this paradigm has been challenged with several studies that have shown that several patients with ED might benefit from curative radiation [4]. It is, therefore, important to find more prognostic variables that might better stratify patients into different treatment regimens. The principal prognostic variables that are based on conventional imaging include: the extent of disease (i.e., LD vs ED), tumour size, lymph node location, presence of pleural and pericardial effusion, involvement of the contralateral lung and metastases to another organ. The usefulness of PET-based indexes that represent the glucose metabolic activity of the tumour in non-SCLC (NSCLC) such as maximum standardized uptake value (SUVmax), metabolic tumour volume (MTV) and total lesion glycolysis (TLG), as prognostic variables has been shown in several studies [6, 7]. However, to the best of our knowledge metabolic parameters have been largely unexplored to predict survival in SCLC [8]. The purpose of the current study is to evaluate the role of 18F-Fluorodeoxyglucose PET/CT (18F-FDG PET/CT) in staging of patients with SCLC and to assess metabolic (SUVmax, MTV and TLG) and morphologic [computed tomography volume (CTvol)] parameters as predictors of progression-free survival (PFS) and OS.
Materials and methods
Subjects
This retrospective study was approved by the institutional review board with a waiver of informed consent. Inclusion criteria included: consecutive patients with biopsy-proven SCLC (i.e., bronchoscopic or trans-thoracic Tru-Cut biopsies), baseline 18F-FDG PET/CT performed in our institution between January 2007 and December 2012, diagnostic CT/MRI of the head and a bone scan performed up to 4 weeks before or after the 18F-FDG PET/CT and clinical data available in the electronic medical records. Exclusion criteria included: patients who did not perform the 18F-FDG PET/CT in our institution and for whom clinical data was not available. All patients received platinum-based chemotherapy along with etoposide. Patients with LD received additional radiation (cycle 1–2 or 2–3). 18F-FDG PET/CT is part of a baseline assessment in patients with SCLC in our institution; unfortunately, due to reimbursement issues, not all patients have it performed. The electronic medical records of all patients were reviewed to identify variables including: age, gender, body mass index (BMI), VALSG classification, staging procedures done and their results (i.e., 18F-FDG PET/CT, CT and MRI scans, bone scintigraphy and bone marrow biopsy) and OS and PFS. The outcome of interest for OS was death with patients lost to follow-up censored at the date of last follow-up. PFS was measured from treatment commencement to the documented date of disease progression revealed by imaging [i.e., based on the response evaluation criteria in solid tumours (RECIST 1.1)].
18F-FDG PET/CT study
18F-FDG PET/CT was performed using an integrated PET/CT scanner (DiscoverySTE, GE Medical Systems, Milwaukee, WI). Intravenous 18F-FDG dose varied from 370 to 666 MBq (10–18 mCi) according to patient’s weight, and 800–1000 mL of diluted iodinated contrast material was administered orally for bowel opacification. Chest CT was performed with patients asked to hold their breath with a tube voltage of 120 kVp, spiral CT at 0.8 s per rotation, 100 mAs, section thickness of 3.75 mm, and a 3.75-mm interval with image reconstruction every 2.5 mm. Contrast-enhanced CT was performed from skull base to mid-thigh with a tube voltage of 120 kVp, spiral CT at 0.8 s per rotation with modulated 40–300 mAs, section thickness of 3.75 mm, and a 3.75-mm interval with image reconstruction every 2.5 mm. Iodine contrast media (Ultravist 300; iopromide 0.623 g/ml, Bayer Schering PharmaAG, Berlin, Germany; 1.5 cm3/kg) was intravenously administered in all examinations, except for patients with iodine hypersensitivity or renal insufficiency. PET emission images were obtained using a weight-based protocol, with 2 min of acquisition time per bed position. Five to six bed positions from skull base to mid-thigh resulted in an acquisition time of 18–20 min. All PET images were reconstructed using an iterative algorithm, with CT-based attenuation correction applied.
Imaging analysis
PET-based metabolic parameters included SUVmax, MTV and TLG. These variables were evaluated for the primary lung lesion and for the primary lesion with hilar and/or mediastinal lymphadenopathy [referred to as total SUVmax (TSUVmax), total MTV (TMTV) and total TLG (TTLG)]. We used software (Volume Viewer 2, Voxtool 6.12.3, GE) that defines the PET-based lesion contour with a cut-off value of 42 % of the tumoral SUVmax and provides the following parameters: SUVmean, SUVmax, MTV and TLG. SUV is a semi-quantitative index that is calculated by the ratio of FDG concentration in a selected region of interest (ROI) to the injected dose which is normalized to body weight. SUVmax reflects the maximal value within a selected ROI. TLG is the product of SUVmean and MTV which calculate the volume of the metabolically active areas of the tumour. The CT-based parameter included the volume of the primary tumour (CTvol) only, as the hilar and mediastinal lymph node volumes could not be accurately measured in 12/27 cases in which mediastinal and/or hilar lymphadenopathy presented as a lymph node conglomerate. CTvol of the lung tumour was calculated based on three dimensional (3D) measurements on CT (i.e., volume of ellipsoid = 4/3πabc). VALSG staging was assessed using the VALSG classification by three independent radiologists: Hanna Bernstine, a nuclear medicine specialist, who staged the patients based on 18F-FDG PET/CT findings; and (Yael Rapson and Liran Domachevsky), experienced radiologists, who staged the patients based on conventional baseline imaging and were blinded to the PET portion. Conventional imaging included: CT of the chest, abdomen and pelvis (i.e., the CT portion of the 18F-FDG PET/CT exam) along with either contrast-enhanced CT or MRI of the brain and bone scintigraphy. Bone scintigraphy and CT/MRI of the head were not always performed in our institution, but images were always stored and available for interpretation in our institutional picture archiving and communication system (PACS).
Statistical analysis
Continuous data were expressed as mean ± standard deviation (SD), categorical data were presented as frequency. Continuous data analysis was performed using an independent t test for parametric variables and a Mann-Whitney test for non-parametric variables. Categorical data were calculated using Pearson's chi-square test. The median values were used as the cut-off point of primary and total tumoral SUVmax, MTV, TLG, and CTvol. A Cox proportional hazard model was used for multivariate analysis. Results of the multivariate Cox regression of PET-based parameters included the parameters remaining statistically significant after adjusting for all the parameters, except for the ED or LD parameters included regardless of their respective p values. A p value ≤ 0.05 was considered statistically significant. IBM’s “Statistical Package for the Social Sciences” (SPSS) statistics software (version 21) was used for statistical analysis.
Results
A total of 108 patients were evaluated, of whom 2 patients were excluded due to lack of available pathological results. 64 out of 106 patients (60 %) had 18F-FDG PET/CT at presentation, of whom 9 patients were excluded as 18F-FDG PET/CT examinations were performed in another institution. The data of 55 patients who received 18F-FDG PET/CT is shown in Tables 1 and 2 based on PFS and OS, respectively. All patients received a baseline CT of the chest, abdomen and pelvis with imaging of the brain either with a contrast-enhanced CT or MRI (50 and 5 patients, respectively). Six patients received bone scintigraphy and four patients underwent bone marrow biopsy.
The role of 18F-FDG PET/CT in staging
Compared with conventional imaging, 18F-FDG PET/CT has changed staging in 6 out of 55 patients (10.9 %), all 6 patients were initially diagnosed with LD and were up staged to ED by 18F-FDG PET/CT (bone and adrenal disease in 4 and 2 patients, respectively) (Fig. 1). Unfortunately, neither bone nor adrenal lesions were biopsy-proven SCLC; however, FDG uptake was high and focal in all bone lesions and was unilateral, intense and correlated with a nodule in the adrenals with no laboratory abnormalities to support a different diagnosis.
75-year-old woman presented with shortness of breath, cough and blood-tinged sputum. (A) Axial CT image of the chest demonstrates a right hilar mass with secondary distal sub-segmental atelectasis. (B) Fused axial 18F-FDG PET/CT image reveals intense FDG uptake in the right hilar mass. (C) Axial CT image of the pelvis demonstrates normal-appearing bones. (D) Fused axial 18F-FDG PET/CT image demonstrates intense medullary FDG uptake. (E) Maximum intensity projection image shows several FDG-avid bone lesions (arrows). The patient was up-staged from LD to ED based on 18F FDG-PET/CT findings
Prediction of PFS and OS
The OS and PFS for the whole group were 16.5 ±14 and12.5 ±12.3 months, respectively. The OS and PFS for patients in whom disease did not recur was 35.2 ±16.6 and 14.8 ±16 months, respectively, while for patients in whom disease recurred, it was 12.4 ±9.4 and 10.7 ±8.8 months, respectively.
TTLG with a cut-off value of 443.8 was statistically significant for OS (Fig. 2) with HR = 2.1 (CI 1.14–3.871, p = 0.017). Patients with high TTLG (>443.8) had a median OS of 13.4 months compared to 25.7 months in patients with low TTLG (<443.8; p = 0.018). TTLG was not statistically significant for PFS (p = 0.19). TTLG of the primary tumour was neither statistically significant for OS nor for PFS (p = 0.07 and 0.29, respectively).
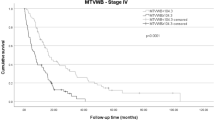
TMTV with a cut-off value of 72.4 was statistically significant for PFS (Fig. 3) with HR = 2.3 (CI 1.11–4.8, p = 0.025). A median PFS of 12.1 and 26.2 months was found in patients with high (>72.4) and low (<72.4) TMTV, respectively (p = 0.005). TMTV was not statistically significant for OS (p = 0.1).
MTV of the primary tumour was not statistically significant for OS (p = 0.3) or PFS (p = 0.2). SUVmax (Fig. 4), TSUVmax and CTvol were not statistically significant for PFS (p = 0.67, 0.77 and 0.17, respectively) nor for OS (p = 0.41, 0.21 and 0.24, respectively).
Discussion
The present study demonstrated that 18F-FDG PET/CT has changed staging in 6 patients (10.9 %) and that metabolic parameters could be used as predictors of survival in patients with SCLC where the TMTV (cut-off value of 72.4) was the only significant index for PFS and the TTLG (cut-off value of 443.8) was found to be significant predictor for OS.
SCLC represents approximately 14 % of newly diagnosed lung cancer with more than 180,000 cases per year worldwide [2]. Watson and Berg [9] have described the distinctive features of SCLC, including the short duration of symptoms prior to diagnosis and the common physical findings, suggesting of mediastinal involvement (e.g. oedema of the neck), findings that are further supported by the radiographic appearance of enlarged and lobulated hilar and paratracheal contours. Other features include high rate of local and distant spread at presentation, good early response to chemotherapy and radiation and the relatively high association with smoking and paraneoplastic syndrome. As such, surgery was never considered as a viable treatment option, and treatment is based mainly on the extension of disease that is the most reproducible prognostic marker [2]. Whenever disease is confined to the hemithorax of the primary tumour, mediastinum or ipsilateral supraclavicular area it is defined as limited and is treated with chemoradiation with the aim of cure. Otherwise, the disease is defined as extended and is treated with palliative chemotherapy. Given the pivotal role of disease extension, accurate staging is mandatory for optimal treatment. At present, staging of SCLC does not include 18F-FDG PET/CT and its role is uncertain, although it is the modality of choice for staging NSCLC [5]. A meta-analysis performed by Thomson et al [10] found 12 studies addressing the role of 18F-FDG PET in staging SCLC. 18F-FDG PET has changed staging in 13% of patients with upstaging in 9% (0-33%) and downstaging in 4% (0-17%). A second meta-analysis conducted by Ruben et al [11] has shown that 18F-FDG PET has changed clinical management in 28-38% of cases. The addition of 18F-FDG PET resulted in the addition and exclusion of radiation in 6 and 9% of cases, respectively. The main drawbacks of these studies include relatively small number of patients, the use of 18F-FDG PET and not 18F-FDG PET/CT in most of the studies and the lack of histological confirmation. Fischer et al [12] showed in a prospective study that the sensitivity for accurate staging was 79%, 93% and 93% with specificity of 100%, 83% and 100% for standard staging (i.e., CT of the chest and upper abdomen and bone marrow biopsy) , 18F-FDG PET and 18F-FDG PET/CT, respectively. We have found that 18F-FDG PET/CT has changed staging in 6 out of 55 patients (10.9 %); all 6 patients were initially diagnosed with LD and were up-staged to ED by 18F-FDG PET/CT. In 4 patients, 18F-FDG PET/CT revealed medullary bone disease while the other two patients had intense FDG uptake in normal appearing adrenal glands. Our results are in accordance with the published data and strengthen the rationale for the use of 18F-FDG PET/CT in staging patients with SCLC.
The significance of finding prognostic variables is crucial in SCLC as the overall prognosis is poor (i.e., median survival of 18–26 months and less than 12 months for ED and LD, respectively [10]) and has not changed much in the last two decades. Any ongoing and future research with new therapeutic regimens and novel drugs has to be based on understanding the effects of different variables on patient outcomes, and will also allow better patient stratification. At present, there are several well-established, good prognostic variables including young age, being a woman and good performance status, whereas elevated lactate dehydrogenase, low sodium and albumin levels and liver metastases are associated with poor prognoses [13]. Still, the extension of disease, which is represented by the VALSG classification, is the most significant prognostic variable. In addition to imaging-based anatomical variables that mainly focused on location, size and number of tumours, the use of tumour metabolic parameters such as SUVmax, MTV and TLG might be helpful. A retrospective study performed by Pandit et al. [14] demonstrated that SUVmax is negatively correlated with survival (p = 0.0021) in patients with SCLC. Lee et al. [8] demonstrated that high SUVmax (>8.7) is associated with poor survival (HR = 3.74; CI 1.67–8.37; p = 0.001). Subgroup analysis revealed that high SUVmax was associated with poor prognosis in the LD group (20.1 vs. 35.3 months; p = 0.02) as well as in the ED group (9.5 vs. 17.7 months; p = 0.007). Arslan et al. [15] assessed quantitative metabolic parameters including SUVmax, SUVmean, TMTV and TLG and found that only TLG (cutoff for MTV calculation > 50 % of SUVmax within the tumour) predicted survival (p = 0.027). We have shown that TTLG was a significant predictor of OS and TMTV was a significant predictor for PFS. Metabolic and CT-based parameters in the primary tumour alone were not significant predictors for PFS or OS. These findings emphasize the significant role of tumour burden in SCLC in accordance with the typical appearance in which hilar and mediastinal lymphadenopathy is usually more pronounced at presentation compared to NSCLC.
Our study has several limitations. First it is a retrospective study with intrinsic biases. Second, there is no consensus regarding the optimal cut-off value to delineate the lesion volume. Third, as with most other studies, because SCLC is not treated with surgery, there is no histopathological confirmation of presumed areas of involvement (i.e., except the primary lesion) that can be referred to as the gold standard. Fourth, there was no standardized protocol for the bone scintigraphy and for the CT/MRI of the head as several of which were performed in different institutions.
In conclusion, we have shown that 18F-FDG PET/CT improves staging of patients with SCLC and we believe that this exam could be included in the evaluation of patients with SCLC at presentation. In addition, we have shown that metabolic parameters obtained by total lung and lymph node burdens could be used as predictors for PFS and OS in patients with SCLC.
Abbreviations
- CTvol:
-
Computed tomography volume
- MTV:
-
Metabolic tumour volume
- NSCLC:
-
Non-small cell lung cancer
- SCLC:
-
Small cell lung cancer
- SUVmax:
-
Maximum standardized uptake value
- TLG:
-
Total lesion glycolisis
References
Karve SJ, Price GL, Davis KL, Pohl GM, Smyth E, Bowman L (2014) Comparison of demographics, treatment patterns, health care utilization, and costs among elderly patients with extensive-stage small cell and metastatic non-small cell lung cancers. BMC Health Serv Res 14(1):555
Van Meerbeeck JP, Fennell DA, De Ruysscher DKM (2011) Small-cell lung cancer. Lancet 378(9804):1741–1755
Brink I, Schumacher T, Mix M et al (2004) Impact of [18F] FDG-PET on the primary staging of small-cell lung cancer. Eur J Nuc Med Mol Imaging 31(12):1614–1620
Diniz G, Unlu I, Gokce T et al (2006) Evaluation of curative and palliative radiotherapy efficacy in extensive stage small cell lung cancer. Saudi Med J 27(7):992–996
Gallamini A, Zwarthoed C, Borra A (2014) Positron Emission Tomography (PET) in Oncology. Cancers 6(4):1821–1889
Al-Sarraf N, Gately K, Lucey J et al (2008) Clinical implication and prognostic significance of standardised uptake value of primary non-small cell lung cancer on positron emission tomography: analysis of 176 cases. Eur J Cardio Thorac Surg Off J Eur Assoc Cardio Thorac Surg 34(4):892–897
Zhang H, Wroblewski K, Appelbaum D, Pu Y (2013) Independent prognostic value of whole-body metabolic tumor burden from FDG-PET in non-small cell lung cancer. Int J Comput Assist Radiol Surg 8(2):181–191
Lee YJ, Cho A, Cho BC et al (2009) High tumor metabolic activity as measured by fluorodeoxyglucose positron emission tomography is associated with poor prognosis in limited and extensive stage small-cell lung cancer. Clin Cancer Res Off J Am Assoc Cancer Res 15(7):2426–2432
Watson WL, Berg JW (1962) Oat cell lung cancer. Cancer 15:759–768
Thomson D, Hulse P, Lorigan P, Faivre-Finn C (2011) The role of positron emission tomography in management of small cell lung cancer. Lung Cancer Amst Neth 73(2):121–126
Ruben JD, Ball DL (2012) The efficacy of PET staging for small-cell lung cancer: a systematic review and cost analysis in the Australian setting. J Thorac Oncol Off Publ Int Assoc Study Lung Cancer 7(6):1015–1020
Fischer BM, Mortensen J, Langer SW et al (2007) A prospective study of PET/CT in initial staging of small-cell lung cancer: comparison with CT, bone scintigraphy and bone marrow analysis. Ann Oncol Off J Eur Soc Med Oncol ESMO 18(2):338–345
Foster NR, Mandrekar SJ, Schild SE et al (2009) Prognostic factors differ by tumor stage for small cell lung cancer: a pooled analysis of North Central Cancer Treatment Group trials. Cancer 115(12):2721–2731
Pandit N, Gonen M, Krug L, Larson SM (2003) Prognostic value of [18F]FDG-PET imaging in small cell lung cancer. Eur J Nucl Med Mol Imaging 30(1):78–84
Arslan N, Tuncel M, Kuzhan O et al (2011) Evaluation of outcome prediction and disease extension by quantitative 2-deoxy-2-[18F] fluoro-D-glucose with positron emission tomography in patients with small cell lung cancer. Ann Nucl Med 25(6):406–413
Acknowledgments
The scientific guarantor of this publication is Dr Hanna Bernstine. The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. One of the authors has significant statistical expertise. Institutional review board approval was obtained. Written informed consent was waived by the institutional review board. Methodology: retrospective, observational, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Additional information
Liran Domachevsky and Alona Zer contributed equally to this work.
Rights and permissions
About this article
Cite this article
Zer, A., Domachevsky, L., Rapson, Y. et al. The Role of 18F-FDG PET/CT on Staging and Prognosis in Patients with Small Cell Lung Cancer. Eur Radiol 26, 3155–3161 (2016). https://doi.org/10.1007/s00330-015-4132-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-015-4132-2