Abstract
Purpose
The purpose of the study was to assess the role of MR fluoroscopy in the evaluation of post-surgical conditions of Nissen fundoplication due to gastro-oesophageal reflux disease (GERD).
Methods
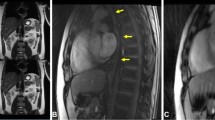
A total of 29 patients (21 patients with recurrent/persistent symptoms and eight asymptomatic patients as the control group) underwent MRI of the oesophagus and gastro-oesophageal junction (GEJ) at 1.5 T. Bolus transit of a buttermilk-spiked gadolinium mixture was evaluated with T2-weighted half-Fourier acquisition single-shot turbo spin-echo (HASTE) and dynamic gradient echo sequences (B-FFE) in three planes. The results of MRI were compared with intraoperative findings, or, if the patients were treated conservatively, with endoscopy, manometry, pH-metry and barium swallow.
Results
MRI was able to determine the position of fundoplication wrap in 27/29 cases (93 % overall accuracy) and to correctly identify 4/6 malpositions (67 %), as well as all four wrap disruptions. All five stenoses in the GEJ were identified and could be confirmed intraoperatively or during dilatation. MRI correctly visualized three cases with motility disorders, which were manometrically confirmed as secondary achalasia. Three patients showed signs of recurrent reflux without anatomical failure.
Conclusion
MRI is a promising diagnostic method to evaluate morphologic integrity of Nissen fundoplication and functional disorders after surgery.
Key points
• MRI offers simultaneous morphological and functional imaging in one diagnostic method.
• MR fluoroscopy offers the possibility to identify the wrap position.
• MRI enables a non-invasive diagnosis, providing detailed information for the surgeon.






Similar content being viewed by others
References
Dallemagne B, Weerts JM, Jehaes C, Markiewitz S, Lombard R (1991) Laparoscopic Nissen fundoplication: preliminary report. Surg Laparosc Endosc 1:138–143
Broeders JA, Roks DJ, Ali UA et al (2013) Laparoscopic anterior 180-degree versus Nissen fundoplication for gastroesophageal reflux disease. Ann Surg 257:850–859
Ireland AC, Holloway RH, Toouli J, Dent J (1993) Mechanisms underlying the antireflux action of fundoplication. Gut 34:303–308
Lafullarde T, Watson DI, Jamieson GG, Myers JC, Game PA, Devitt PG (2001) Laparoscopic Nissen fundoplication: five-year results and beyond. Arch Surg 136:180–184
Bammer T, Hinder RA, Klaus A, Klingler PJ (2001) Five- to eight-year outcome of the first laparoscopic Nissen fundoplications. J Gastrointest Surg 5:42–48
Gopal DV, Chang EY, Kim CY et al (2006) EUS characteristics of Nissen fundoplication: normal appearance and mechanisms of failure. Gastrointest Endosc 63:35–44
Yang H, Watson DI, Kelly J, Lally CJ, Myers JC, Jamieson GG (2007) Esophageal manometry and clinical outcome after laparoscopic Nissen fundoplication. J Gastrointest Surg 11:1126–1133
Siewert JR, Isolauri J, Feussner H (1989) Reoperation following failed fundoplication. World J Surg 13:791–796
Hashemi M, Peters JH, DeMeester TR et al (2000) Laparoscopic repair of large type III hiatal hernia: objective followup reveals high recurrence rate. J Am Coll Surg 190:553–560
Hartl DM, Kolb F, Bretagne E, Marandas P, Sigal R (2006) Cine magnetic resonance imaging with single-shot fast spin echo for evaluation of dysphagia and aspiration. Dysphagia 21:156–162
Barkhausen J, Goyen M, von Winterfeld F, Lauenstein T, Arweiler-Harbeck D, Debatin JF (2002) Visualization of swallowing using real-time TrueFISP MR fluoroscopy. Eur Rad 12:129–133
Curcic J, Fox M, Kaufman E, Forras-Kaufman Z et al (2010) Gastroesophageal junction: structure and function as assessed by using MR imaging. Radiology 257:115–124
Panebianco V, Tomei E, Anzidei M et al (2006) Functional MRI in the evaluation of oesophageal motility: feasibility, MRI patterns of normality, and preliminary experience in subjects with motility disorders. Radiol Med 111:881–889
Kulinna-Cosentini C, Schima W, Lenglinger J et al (2012) Is there a role for dynamic swallowing MRI in the assessment of gastroesophageal reflux disease and oesophageal motility disorders? Eur Rad 22:364–370
Panebianco V, Francioni F, Anzidei M, Anile M, Rolla M, Pasariello R (2006) Magnetic resonance-fluoroscopy as long-term follow-up examination in patients with narrow gastric tube reconstruction after radical esophagectomy. Eur J Cardiothorac Surg 30:663–668
Hunter JG, Smith CD, Branum GD et al (1999) Laparoscopic fundoplication failures: patterns of failure and response to fundoplication revision. Ann Surg 230:595–604
Stein HJ, Siewert H, Feussner H (1994) What are the causes of failure of Nissen’s operation ? Oeso Knowledge - Interactive Information System. The esophageal mucosa: Nissen fundoplication:1–3
Pointner R, Granderath FA (2008) Hiatus hernia and recurrence: the Achilles heel of antireflux surgery? Chirurg 79:974–981
Donahue PE, Samelson S, Nyhus LM, Bombeck CT (1985) The floppy Nissen fundoplication. Effective long-term control of pathologic reflux. Arch Surg 120:663–668
DeMeester TR, Stein HJ (1992) Minimizing the side effects of antireflux surgery. World J Surg 16:335–336
Stein HJ, Feussner H, Siewert JR (1996) Failure of antireflux surgery: causes and management strategies. Am J Surg 171:36–40
Tatum RP, Shi G, Manka MA, Brasseur JG, Joehl RJ, Kahrilas PJ (2000) Bolus transit assessed by an esophageal stress test in postfundoplication dysphagia. J Surg Res 9:56–60
Manabe T, Kawamitsu H, Higashino T et al (2004) Esophageal magnetic resonance fluoroscopy: optimization of the sequence. J Comput Assist Tomogr 28:697–703
Kulinna-Cosentini C, Schima W, Cosentini EP (2007) Dynamic MR imaging of the gastroesophageal junction in healthy volunteers during bolus passage. J Magn Reson Imaging 25:749–754
Raeside MC, Madigan D, Myers JC, Devitt PG, Jamieson GG, Thompson SK (2012) Post-fundoplication contrast studies: is there room for improvement? Br J Rad 85:792–799
Szwerc MF, Gagne DJ, Wiechmann RJ, Maley RH, Santucci TS, Landreneau RJ (2002) Immediate radiographic assessment following laparoscopic antireflux operations is unnecessary. Surg Endosc 16:64–66
Juhasz A, Sundaram A, Hoshino M, Lee TH, Filipi CJ, Mittal SK (2011) Endoscopic assessment of failed fundoplication: a case for standardization. Surg Endosc 25:3761–3766
Lord RV, Kaminski A, Oberg S, Bowrey DJ, Hagen JA, DeMeester SR, Sillin LF, Peters JH, Crookes PF, DeMeester TR (2002) Absence of gastroesophageal reflux disease in a majority of patients taking acid suppression medications after Nissen fundoplication. J Gastrointest Surg 1:3–9
Smith CD, McClusky DA, Rajad M, Lederman AB, Hunter JG (2005) When fundoplication fails: redo? Ann Surg 241:861–869
Fuchs KH, DeMeester TR, Albertucci M (1987) Specificity and sensitivity of objective diagnosis of gastroesophageal reflux disease. Surgery 102:575–580
Hinder RA, Klingler PJ, Perdikis G, Smith SL (1997) Management of the failed antireflux operation. Surg Clin N Am 77:1083–1098
Khajanchee YS, O’Rourke R, Cassera MA, Gatta P, Hansen PD, Swanström LL (2002) Laparoscopic reintervention for failed antireflux surgery: subjective and objective outcomes in 176 consecutive patients. Arch Surg 142:791–792
Stylopoulos N, Bunker CJ, Rattner DW (2002) Development of achalasia secondary to laparoscopic Nissen fundoplication. J Gastrointest Surg 6:368–376
Covotta F, Piretta L, Badiali D et al (2011) Functional magnetic resonance in the evaluation of oesophageal motility disorders. Gastroenterol Res Pract 2011:1–5
Galvani C, Fisichella PM, Grorodner MV, Peretta S, Patti MG (2003) Symptoms are a poor indicator of reflux status after fundoplication for gastroesophageal reflux disease: role of esophageal functions tests. Arch Surg 138:514–518
Donkervoort SC, Bais JE, Rijnhart-de Jong H, Gooszen HG (2003) Impact of anatomical wrap position on the outcome of Nissen fundoplication. Br J Surg 90:854–859
Acknowledgements
The scientific guarantor of this publication is Enrico P. Cosentini. The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. One of the authors has significant statistical expertise. No complex statistical methods were necessary for this paper. Institutional review board approval was obtained. Written informed consent was obtained from all subjects (patients) in this study. Methodology: prospective, diagnostic study, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
This short video in sagittal view shows a normal postoperative appearance after Nissen fundoplication on MRI. Contrast medium passes through the esophagus and the esophagogastric junction through the wrap. The transit time is normal. (MPG 4858 kb)
Rights and permissions
About this article
Cite this article
Kulinna-Cosentini, C., Schima, W., Ba-Ssalamah, A. et al. MRI patterns of Nissen fundoplication: normal appearance and mechanisms of failure. Eur Radiol 24, 2137–2145 (2014). https://doi.org/10.1007/s00330-014-3267-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-014-3267-x