Abstract
Lenalidomide consistently induces transfusion independence and complete cytogenetic response in patients with myelodysplastic syndromes with 5q deletion. Only limited information on long-term outcome is currently available. We performed a long-term follow-up analysis of 42 patients with low or intermediate risk myelodysplastic syndromes and 5q deletion treated with lenalidomide. At a median follow-up of 40 months, 58% of the patients achieved an erythroid response and 48% a cytogenetic response. Thirty-six percent of patients progressed into acute myeloid leukaemia. Most of them (87%) acquired chromosome aberrations in addition to the 5q deletion, i.e. underwent clonal evolution during leukaemogenesis. There were no clinical, cytological or cytogenetic markers at study entry that allowed prediction of increased risk of leukaemic transformation. However, erythroid and cytogenetic responders had a significantly decreased risk of progression to acute myeloid leukaemia (p = 0.001 and p = 0.009, respectively) compared to non-responders. Three and 5 years after study entry, the cumulative incidence of acute myeloid leukaemia for patients with a cytogenetic response was 10% and 21%, respectively, and for patients without cytogenetic response, it was 46% and 60%. Patients with del(5q) myelodysplastic syndromes without erythroid or cytogenetic remission after treatment with lenalidomide have a high risk for clonal evolution and acute myeloid leukaemia progression. In refractory, or relapsing, patients, genetic instability and clonal evolution seem to be the driving forces of leukaemic transformation. Regular follow-up investigations of del(5q) myelodysplastic syndrome patients treated with lenalidomide may help to identify patients requiring alternative treatment strategies.
Similar content being viewed by others
Introduction
Myelodysplastic syndromes (MDS), a heterogeneous group of clonal haematopoietic stem cell disorders, are among the most frequent myeloid neoplasias in elderly patients. Patients with MDS present with uncharacteristic symptoms like fatigue, anaemia, infections and bleeding caused by peripheral cytopenia. The morphological classification is based on the percentage of blasts in the bone marrow, the type and degree of dysplasia and the presence of ring sideroblasts [1]. The incidence is five per 100,000 persons per year in the general population, but increases to 20 to 50 per 100,000 persons per year after 60 years of age [2].
Chromosomal abnormalities provide important prognostic information. Patients with isolated del(5q) MDS often present with macrocytic anaemia, a normal or elevated platelet count, spheronuclear and hypolobulated megakaryocytes, a medullary blast count <5% and female predominance [1, 3–5], sometimes referred to as 5q-syndrome, are believed to have a favourable prognosis. Life expectancy of older patients without transfusion requirement does not seem to be different from the general population [6]. The risk of progression to acute myeloid leukaemia is estimated to be low, at least for patients who do not have additional risk factors such as an elevated blast count, transfusion dependence, or additional chromosome aberrations. However, data from prospective studies on the risk of leukaemic transformation in patients with MDS and deletion 5q are lacking.
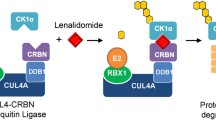
Lenalidomide, a thalidomide analogue with immunomodulatory and anti-angiogenic properties, induces transfusion independence and cytogenetic response in a high proportion of patients with MDS and 5q deletion [7–10]. Based on the results of an international phase II study (MDS-003) [7], lenalidomide has been approved by the US Food and Drug Administration in 2005. So far, there is limited information on the long-term outcome of MDS patients treated with lenalidomide. We report on detailed follow-up data of 42 patients treated with lenalidomide.
Design and methods
Patients
Our cohort included all patients treated with lenalidomide at the only European centre of the MDS-003 (Lenalidomide-MDS-003) study (42 patients St. Johannes Hospital, Duisburg, Germany). All patients with transfusion-dependent anaemia due to low- or intermediate-1-risk MDS (according to the International Prognostic Scoring System (IPSS)) associated with a 5q deletion with or without additional cytogenetic abnormalities were eligible. Thirty-six of the patients were enrolled in the MDS-003 study between November 2003 and May 2006 [7]. In the period between the closure of the MDS-003 study and the start of a subsequent study, six additional patients with MDS were treated with lenalidomide (starting dose, 10 mg daily) in accordance with the study protocol of the MDS-003 study [7]. Written informed consent was provided according to the Declaration of Helsinki. Lenalidomide therapy is still ongoing in responding patients. Dose adjustments were performed in the majority of patients due to side effects such as neutropenia. Patient characteristics are summarised in Table 1 and Electronic supplementary material 1 [7].
Median follow-up of the patients after entering the study was 3.3 years, ranging from 2.3 to 5 years. Time between diagnosis and study entry was 0 to 15 years, median 2.1 years. Before study entry, 20 patients were treated with various agents, e.g. erythropoietin, all-trans-retinoic acid or anti-thymocyte globulin (Electronic supplementary material 2).
Standardised cytogenetic investigations
Cytogenetic investigations were performed centrally according to standard procedures as described [11]. Whenever possible, 25 metaphases were analysed. Description of chromosome aberrations and clone definition followed the recommendations of the International System for Cytogenetic Nomenclature [12]. A structural chromosome aberration or a gain of a whole chromosome found in at least two metaphases, or a loss of a whole chromosome found in at least three metaphases, were defined as clonal aberrations. Single cell aberrations were also considered clonal if they were confirmed by fluorescence in situ hybridization (FISH) or if they were already known from previous investigations. FISH for deletion 5q was included in each investigation. Depending on the aberrations detected during karyotyping, further probes were applied.
A complex karyotype was defined as ≥3 independent aberrations within one clone. Clonal evolution was defined as the acquisition of additional aberrations in clones with a 5q deletion. Independent clones did not contain a 5q deletion. All newly detected clonal aberrations were investigated retrospectively by interphase FISH, in order to clarify whether they were already present at earlier time points.
Cytogenetic and erythroid response
Complete cytogenetic response (CCyR) was defined as disappearance of the 5q deletion or any other chromosome aberration. Partial cytogenetic response (PCyR) was defined as a reduction of aberrant cells of more than 50% compared to the previous cytogenetic investigation [7]. Patients with persistent clones or with a reduction of less than 50% were defined as having no CyR. Furthermore, we distinguished between continuous CyR and transient CyR. Patients with transient CyR initially showed either CCyR or PCyR, but lost their cytogenetic response during follow-up (Electronic supplementary material 3). Accordingly, patients with transient erythroid response reached transfusion independence, but lost it during follow-up.
Morphologic evaluation
Morphologic evaluation was performed centrally at St. Johannes Hospital Duisburg and Hannover Medical School. Patients were diagnosed according to FAB and WHO classification [13, 14]. There was a high concordance of diagnosis between both institutions. Two cases were jointly reviewed and a final diagnosis agreed upon.
Statistical analyses
Time to AML was defined as time from study entry to the date of diagnosis of AML or to the date of last follow-up. Cumulative incidence functions of progression to AML were constructed using the method of Kalbfleisch and Prentice and compared with Gray’s test [15–17]. The Cox proportional hazards model was used for multivariate analysis. Differences in the distribution of individual parameters among patient subsets were analysed using Fisher’s exact or χ2 test for categorised variables and the Mann–Whitney U test for continuous variables. Statistical analyses were conducted using SAS version 9.1.
Results
Long-term follow-up analyses (median observation time: 3.3 years; range: 2.3–5 years) were performed in 42 patients with transfusion-dependent MDS and 5q deletion treated with lenalidomide. The median age was 64 years (range 32–84 years), and there was a female predominance (25 women, 17 men). This cohort had more patients with advanced MDS according to FAB than the whole patient set in the previously reported MDS-003 study (Table 1), which might account for the lower cytogenetic response rate for this population. Twelve of the 42 patients (29%) reached continuous (median 52 months, range 8–60 months), and another 12 patients (29%) reached transient transfusion independence. Twenty patients (48%) achieved a cytogenetic response, but 12 patients lost this during follow-up. Notably, in 12 analyses, the 5q- clone was detected only by karyotyping and not by FISH. Eight patients are in continuous cytogenetic remission (Table 2).
Four patients progressed from low-risk MDS to higher risk MDS (refractory anaemia with excess of blasts according to FAB-classification [13]) within a median of 12.5 months after initiation of treatment with lenalidomide (range 12–16 months; Table 2). Among the 14 patients with low-risk MDS and an isolated deletion in 5q without severe bone marrow hypoplasia, three patients (patients 26, 29, and 38) underwent leukaemic transformation after having been treated with lenalidomide for a median of 10.5 months (range 9–40 months; Table 2). In total, 15 of the 42 patients (36%) progressed to acute myeloid leukaemia, while undergoing treatment with lenalidomide for a median of 12 months (range 5–50 months). Eight of them had not received any pre-treatment (Electronic supplementary material 2). Time from diagnosis to development of AML was 51 months (median, range 15–90 months). Except for one patient, all patients who progressed to AML died within a few months (Table 2). After start of treatment, the cumulative incidence of AML was 29% after 3 years and 42% after 5 years (Fig. 1).
We analysed the influence of gender, age, blast count, MDS subtype according to the WHO classification, IPSS risk score and additional chromosome aberrations to identify predictive markers for progression to AML (Fig. 2). There were no significant differences in the cumulative incidences of AML 3 and 5 years after treatment with lenalidomide with regard to gender, age, blast count, WHO subtype, IPSS risk score or additional chromosome aberrations at study entry. However, because of small numbers in some of those subgroups, the statistical analysis may not reveal a relationship.
Depicted are the cumulative incidences of acute myeloid leukaemia since study entry with lenalidomide therapy regarding gender (a), age (b), amount of blasts (c), WHO diagnosis (d), International Prognostic Scoring System score (e) and additional cytogenetic aberrations besides deletion 5q (f). Lack of markers at study entry allowed no prediction of an increased risk of leukaemic transformation
When analysing erythroid and cytogenetic response, significant differences in the risk of progression to AML became evident. Patients with continuous or transient erythroid response carried a significantly lower risk of progression to AML than patients without an erythroid response (p = 0.001; Fig. 3a, b). Three out of 20 patients with cytogenetic response and 12 of 22 patients without cytogenetic response underwent progression to AML (p = 0.009). Notably, none of the eight patients (19%) who achieved a continuous cytogenetic response underwent leukaemic transformation. Three and 5 years after study entry, the cumulative incidence of AML for patients with a cytogenetic response was 10% and 21%, respectively, and for patients without cytogenetic response, it was 46% and 60%. Patients with a transient CyR had a risk of progression of 17% after 3 years of lenalidomide therapy. The risk rose to 51% after 5 years once the cytogenetic response was lost. Thus, there was a significantly different risk of progression to AML for patients with continuous, transient and lack of cytogenetic response after 3 and 5 years of lenalidomide treatment (p = 0.018; Fig. 3c, d). Three patients with transient cytogenetic response transformed into AML; loss of cytogenetic response and transformation into AML occurred almost simultaneously. In a Cox regression analysis considering transfusion independence and cytogenetic response as covariables, the risk ratio was 0.24 (95% confidence interval 0.073–0.798, p = 0.02) and 0.334 (0.09–1.238, p = 0.1011), respectively. Thus, the transfusion independence had a stronger impact on the risk of leukaemic transformation.
Most patients (13 of 15, 87%) with progression to AML acquired chromosome aberrations in addition to 5q deletion during follow-up, and nine of those (60%) evolved to a complex karyotype (Fig. 4; Electronic supplementary material 4). The most frequent additional aberrations were deletion 17p, trisomy 21, trisomy 8 and isodicentric chromosome X. Two patients, who developed a complex karyotype, underwent early stem cell transplantation and did not progress to AML. Moreover, two patients without clonal evolution and without cytogenetic response progressed to AML at 5 and 6 months after study entry, respectively. For 13 patients with clonal evolution, time to progression to AML was 12 months (median, range 6 to 50 months), after treatment with lenalidomide had been initiated. Apart from two patients, none of the patients with clonal evolution or with leukaemic transformation had reached continuous transfusion independence.
To clarify the question whether small clones with complex karyotypes were already present at study entry, FISH probes to detect additional chromosome aberrations such as trisomy 8, trisomy 21 or loss of 17p were applied. In no case, however, did FISH identify a small clone with the respective chromosome aberrations at an earlier investigation or at study entry, although aberrations of the complex clones, e.g. loss of the tumour suppressor gene TP53 due to loss of 17p, were confirmed at the time of clonal evolution.
Discussion
Lenalidomide, an amino-substituted thalidomide analogue with immunomodulatory and anti-angiogenic properties, leads to transfusion independence in over two thirds of patients with MDS and 5q deletion [7]. This is in agreement with the results of this study, in which about 60% of the patients achieved an erythroid response. Clearly, this leads to a major improvement in the quality of life of MDS patients with transfusion-dependent anaemia.
An important finding of this study is that none of the patients with a continuous erythroid and cytogenetic response transformed to acute myeloid leukaemia. In contrast, patients who did not achieve a cytogenetic response or lost this response during the course of the disease had an increased risk of leukaemic transformation. During progression to AML, most of the clones with deletion 5q acquired additional chromosome aberrations and developed into complex clones. Thus, genetic instability and clonal evolution seem to be the driving forces of leukaemic transformation in MDS patients treated with lenalidomide. It is known that complex clones are associated with a very poor prognosis both in MDS and AML [18, 19]. In this study, most patients who had developed complex clones also died within a few months.
It is difficult to evaluate whether patients treated with lenalidomide have an increased risk of leukaemic transformation. So far, no prospective clinical data from fully randomised trials are available, and there are only limited retrospective data. According to the IPSS [20] and newer risk classification systems [6], MDS with an isolated 5q deletion is associated with a good prognosis, although transfusion dependence is an independent unfavourable prognostic factor. In a retrospective study from the pre-lenalidomide era [21], the leukaemic transformation rate was 8% for patients with less than 5% blasts, but rose dramatically if more than 5% blasts were present. In contrast, the risk of progression to AML after lenalidomide treatment did not differ for patients with more or less than 5% blasts. Also, other potential risk factors like gender, age, blast count, MDS subtype according to WHO classification, IPSS score and cytogenetic aberrations in addition to 5q deletion did not help to predict leukaemic transformation. Although this might partly be due to low patient numbers in the patient population analysed, the negative effect of these risk factors could also be blunted by treatment with lenalidomide.
The only significant risk factors predicting progression to AML were the lack of continuous erythroid and continuous cytogenetic response. Remarkably, none of the patients with continuous cytogenetic response developed AML. Furthermore, patients with transient erythroid and transient cytogenetic response had a significantly lower risk of transformation after 3 and 5 years of lenalidomide treatment than patients without erythroid or cytogenetic response (p = 0.001 and p = 0.009). This finding is in line with a previous report on 168 patients participating in four clinical trials, in which the estimated 10-year risk for leukaemia progression was 15% for cytogenetic responders and 67% for cytogenetic non-responders or non-evaluable patients [22]. However, as shown in this and previous studies [7, 23], patients with erythroid or cytogenetic response can also develop complex clones and progress to AML. Since the majority of patients with erythroid or cytogenetic response lost the response during follow-up, careful clinical, morphological and cytogenetic follow-up is needed. Cytogenetic investigation should always include full karyotype analyses, since in many patients loss of cytogenetic response was indicated by only one metaphase with 5q deletion, whereas FISH analysis provided a negative result. Thus, FISH using a probe for the commonly deleted region in 5q [24] does not seem to be sufficient for follow-up analysis. Our results underline the importance of a close and careful cytogenetic follow-up even after reaching a CCyR, since the clone with 5q deletion may reappear, increase in size and acquire additional chromosome aberrations, indicating progression of the disease.
The long arm of chromosome 5 is the most frequently deleted region in MDS, being present in 20% to 30% of the patients [19]. Deletions of 5q are also the most frequent aberrations in complex karyotypes in secondary MDS/AML after chemo- and radiotherapy. The complex karyotypes in this series contained characteristic aberrations like deletions of 7q, deletions of 17p or trisomy 21. Inactivation of p53, the guardian of the genome with important functions in DNA repair and apoptosis induction, may be a critical early event during clonal evolution of 5q- clones, triggering genetic instability and the acquisition of secondary chromosome aberrations [25]. Two complex clones in this series contained a deletion of 17p with loss of the TP53 gene.
Importantly, the time between MDS diagnosis and treatment with lenalidomide in the patient cohort presented in this manuscript was 2.1 years, ranging from 0–15 years. Also, most of the patients had previous treatments with other agents that might have led to selection of genetic subclones. Unfortunately, FISH analyses did not seem to be the optimum method to identify these small pre-existing clones at diagnosis, probably due to a low detection limit of 2% to 11%, depending on the probe applied [26]. There are some limitations to the study presented here. The patient numbers are too small for robust subgroup analyses, so that some prognostic factors like the IPSS risk at lenalidomide treatment start might not have become statistically significant. Also, pre-lenalidomide therapies and the long median time between MDS diagnosis and lenalidomide exposure might have impacted on the disease course.
It will be of utmost importance to identify genetic lesions inducing resistance to lenalidomide and possibly also predisposing to leukaemic transformation. Gene expression profiling studies have identified genes like SPARC (osteonectin) that are up-regulated during lenalidomide treatment or identified an erythroid differentiation signature predicting response to lenalidomide [27, 28]. Thus, in the near future, new tools may be available to identify patients who have an increased risk not to respond to lenalidomide up-front before treatment and who may be at increased risk for transformation to AML. Until these new tools are available, the results of this study warrant regular and careful follow-up investigation of all patients treated with lenalidomide.
References
Jaffe ES, Harris NL, Stein H, Vardiman JW (2001) World health organization classification of tumours vol. 3. Pathology and genetics: tumours of haematopoietic and lymphoid tissues. IARC, Lyon
Cazzola M, Malcovati L (2005) Myelodysplastic syndromes—coping with ineffective hematopoiesis. N Engl J Med 352(6):536–538
Van den Berghe H, Vermaelen K, Mecucci C, Barbieri D, Tricot G (1985) The 5q- anomaly. Cancer Genet Cytogenet 17(3):189–255
Boultwood J, Lewis S, Wainscoat JS (1994) The 5q- syndrome. Blood 84(10):3253–3260
Tasaka T, Tohyama K, Kishimoto M, Ohyashiki K, Mitani K, Hotta T et al (2008) Myelodysplastic syndrome with chromosome 5 abnormalities: a nationwide survey in Japan. Leukemia 22(10):1874–1881
Malcovati L, Germing U, Kuendgen A, Della Porta MG, Pascutto C, Invernizzi R et al (2007) Time-dependent prognostic scoring system for predicting survival and leukemic evolution in myelodysplastic syndromes. J Clin Oncol 25(23):3503–3510
List A, Dewald G, Bennett J, Giagounidis A, Raza A, Feldman E et al (2006) Lenalidomide in the myelodysplastic syndrome with chromosome 5q deletion. N Engl J Med 355(14):1456–1465
List AF (2005) Emerging data on IMiDs in the treatment of myelodysplastic syndromes (MDS). Semin Oncol 32(4 Suppl 5):S31–S35
Giagounidis A, Fenaux P, Mufti GJ, Muus P, Platzbecker U, Sanz G, Cripe L, Lilienfeld-Toal M, Wells RA (2008) Practical recommendations on the use of lenalidomide in the management of myelodysplastic syndromes. Ann Hematol 87(5):345–352
Giagounidis AA, Haase S, Heinsch M, Gohring G, Schlegelberger B, Aul C (2007) Lenalidomide in the context of complex karyotype or interrupted treatment: case reviews of del(5q)MDS patients with unexpected responses. Ann Hematol 86(2):133–137
Schlegelberger B, Metzke S, Harder S, Zühlke-Jenisch R, Zhang Y, Siebert R (1999) Classical and molecular cytogenetics of tumor cells. In: Wegener R (ed) Diagnostic cytogenetics. Springer, Heidelberg, pp 151–185
ISCN (1995) Guidelines for cancer cytogenetics, supplement to an international system for human cytogenetic nomenclature. Mitelman F (ed) S Karger, Basel
Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton DA, Gralnick HR et al (1982) Proposals for the classification of the myelodysplastic syndromes. Br J Haematol 51(2):189–199
Jaffe ES, Harris NL, Diebold J, Muller-Hermelink HK (1999) World Health Organization classification of neoplastic diseases of the hematopoietic and lymphoid tissues. A progress report. Am J Clin Pathol 111(1 Suppl 1):S8–S12
Cox DR (1972) Regression models and life tables. J R Stat Soc 34:187
Gray RJ (1988) A class of K-sample tests for comparing the cumulative incidence of a competing risk. Ann Stat 16:1141–1154
Kalbfleisch JD, Prentice RL (1980) The statistical analysis of failure time data (ed 1). Wiley, New York
Farag SS, Archer KJ, Mrozek K, Ruppert AS, Carroll AJ, Vardiman JW et al (2006) Pretreatment cytogenetics add to other prognostic factors predicting complete remission and long-term outcome in patients 60 years of age or older with acute myeloid leukemia: results from Cancer and Leukemia Group B 8461. Blood 108(1):63–73
Haase D, Germing U, Schanz J, Pfeilstocker M, Nosslinger T, Hildebrandt B et al (2007) New insights into the prognostic impact of the karyotype in MDS and correlation with subtypes: evidence from a core dataset of 2124 patients. Blood 110(13):4385–4395
Greenberg P, Cox C, LeBeau MM, Fenaux P, Morel P, Sanz G et al (1997) International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood 89(6):2079–2088
Giagounidis AA, Germing U, Haase S, Hildebrandt B, Schlegelberger B, Schoch C et al (2004) Clinical, morphological, cytogenetic, and prognostic features of patients with myelodysplastic syndromes and del(5q) including band q31. Leukemia 18(1):113–119
List A (2008) Immunomodulatory drugs in myelodysplastic syndromes: long-term outcome. Hematol Educ 2(1):91–94
List A, Kurtin S, Roe DJ, Buresh A, Mahadevan D, Fuchs D et al (2005) Efficacy of lenalidomide in myelodysplastic syndromes. N Engl J Med 352(6):549–557
Mallo M, Arenillas L, Espinet B, Salido M, Hernandez JM, Lumbreras E et al (2008) Fluorescence in situ hybridization improves the detection of 5q31 deletion in myelodysplastic syndromes without cytogenetic evidence of 5q-. Haematologica 93(7):1001–1008
Jädersten MS, Saft L, Pellagatti P, Göhring G, Nilsson L, Wainscoat JS, Boultwood J, Porwit A, Schlegelberger B, Hellström-Lindberg E (2009) Clonal heterogeneity in the 5q- syndrome: p53 expressing progenitors prevail during lenalidomide treatment and expand at disease progression. Haematologica (in press)
Göhring G, Schlegelberger B, Hellström-Lindberg E (2008) Myelodysplastic syndromes. In: Stilgenbauer S, Döhner H (eds) Molecular diagnostics in hematological oncology. UNI-MED, Bremen, pp 117–125
Ebert BL, Pretz J, Bosco J, Chang CY, Tamayo P, Galili N et al (2008) Identification of RPS14 as a 5q- syndrome gene by RNA interference screen. Nature 451(7176):335–339
Galili N, Raza A (2006) Immunomodulatory drugs in myelodysplastic syndromes. Expert Opin Investig Drugs 15(7):805–813
Acknowledgments
The authors would like to thank Lana Harder, Claudia Haferlach, Brigitte Mohr and Stefan Bohlander for providing cytogenetic data and Gillian Teicke for her help in preparing the manuscript. Finally, we thank Dr. Robert Knight, Celgene, for allowing us to use data obtained within the Celgene MDS-003 clinical trial.
Authorship and disclosures
GG, AG and BS were the principal investigators and take primary responsibility for the paper. AG and CA recruited the patients. GG, GB and HHK performed the laboratory work for this study. MZ participated in the statistical analysis. AG, EHL and BS co-ordinated the research. GG, AG and BS wrote the paper. The authors reported no potential conflicts of interest.
Funding
This study was supported by the BMBF (German Competence Network Acute and Chronic Leukaemias).
Author information
Authors and Affiliations
Corresponding author
Additional information
G. Göhring and A. Giagounidis contributed equally to this manuscript.
Electronic supplementary materials
Below is the link to the electronic supplementary material.
Electronic supplementary material 1
Cytogenetic response under lenalidomide (XLS 42 kb)
Electronic supplementary material 2
Pre-treatment of patients with MDS and deletion in 5q before lenalidomide (XLS 29 kb)
Electronic supplementary material 3
Depicted are the cumulative incidences of acute myeloid leukaemia since study entry with lenalidomide therapy regarding neutropenia (a) and thrombocytopenia (b). (DOC 73.5 kb)
Electronic supplementary material 4
Cytogenetic characteristics of the patients representing classical cytogenetics and FISH data (JPEG 434 kb).
Rights and permissions
About this article
Cite this article
Göhring, G., Giagounidis, A., Büsche, G. et al. Patients with del(5q) MDS who fail to achieve sustained erythroid or cytogenetic remission after treatment with lenalidomide have an increased risk for clonal evolution and AML progression. Ann Hematol 89, 365–374 (2010). https://doi.org/10.1007/s00277-009-0846-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-009-0846-z