Abstract
Purpose
To evaluate the in-treatment diagnostic accuracy of FDG PET/CT in large-vessel giant cell arteritis (LV-GCA) by serial scans before and after a short course of high-dose glucocorticoid treatment.
Methods
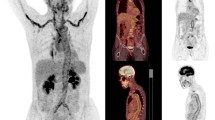
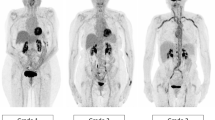
Twenty-four glucocorticoid-naïve patients with new-onset PET/CT verified LV-GCA (pre-treatment baseline PET) were prospectively included. Excluded were patients with a previous history of GCA or polymyalgia rheumatica, LV-GCA-mimicking conditions and patients on immunosuppressive therapy. All patients were treated with 60 mg of oral prednisolone daily and assigned for in-treatment FDG PET/CT after either 3 (PET3) or 10 days (PET10). Two experienced nuclear medicine physicians, blinded to patients’ clinical data, reviewed the FDG PET/CT images. A visual semi-quantitative approach was used. Segmental and homogenous FDG uptake in the wall of the aorta and/or supra-aortic branches with higher uptake intensity than liver was considered consistent with vasculitis. Inter-reader reliability was evaluated.
Results
Although glucocorticoid treatment attenuated FDG uptake in large vessels, LV-GCA was accurately diagnosed in 10/10 patients after 3 days of treatment, but only in 5/14 patients after 10 days of treatment (p < 0.001). Interrater reliability was substantial (agreement 87%, Cohen’s weighted kappa 0.70). No correlation between CRP and FDG uptake was found.
Conclusions
Within 3 days of high-dose glucocorticoid treatment, FDG PET/CT can diagnose LV-GCA with high sensitivity. This window of opportunity ensures that prompt glucocorticoid treatment can be initiated to avoid debilitating GCA complications with a limited effect on diagnostic accuracy. After 10 days of treatment, FDG PET/CT sensitivity decreases significantly.



Similar content being viewed by others
References
Ashton-Key MR, Gallagher PJ. False-negative temporal artery biopsy. Am J Surg Pathol. 1992;16:634.
Luqmani R, Lee E, Singh S, Gillett M, Schmidt WA, Bradburn M, et al. The role of ultrasound compared to biopsy of temporal arteries in the diagnosis and treatment of giant cell arteritis (TABUL): a diagnostic accuracy and cost-effectiveness study. Health Technol Assess (Rockv). 2016;20:1–270.
Schmidt WA, Seifert A, Gromnica-ihle E, Krause A, Natusch A. Ultrasound of proximal upper extremity arteries to increase the diagnostic yield in large-vessel giant cell arteritis. Rheumatology. 2008;47:96–101.
Muratore F, Kermani TA, Crowson CS, Green AB, Salvarani C, Matteson EL, et al. Large-vessel giant cell arteritis: a cohort study. Rheumatology (Oxford). 2015;54:463–70.
Brack A, Martinez-Taboada V, Stanson A, Goronzy JJ, Weyand CM. Disease pattern in cranial and large-vessel giant cell arteritis. Arthritis Rheum. 1999;42:311–7.
Fuchs M, Briel M, Daikeler T, Walker UA, Rasch H, Berg S, et al. The impact of 18F-FDG PET on the management of patients with suspected large vessel vasculitis. Eur J Nucl Med Mol Imaging. 2012;39:344–53.
Tuckwell K, Collinson N, Dimonaco S, Klearman M, Blockmans D, Brouwer E, et al. Newly diagnosed vs. relapsing giant cell arteritis: baseline data from the GiACTA trial. Semin Arthritis Rheum. 2017;46:657–64.
Stellingwerff MD, Brouwer E, Lensen K-JDF, Rutgers A, Arends S, van der Geest KSM, et al. Different scoring methods of FDG PET/CT in Giant cell arteritis. Medicine (Baltimore). 2015;94:e1542.
Walter MA, Melzer RA, Schindler C, Müller-Brand J, Tyndall A, Nitzsche EU. The value of [18F]FDG-PET in the diagnosis of large-vessel vasculitis and the assessment of activity and extent of disease. Eur J Nucl Med Mol Imaging. 2005;32:674–81.
Prieto-González S, Depetris M, García-Martínez A, Espígol-Frigolé G, Tavera-Bahillo I, Corbera-Bellata M, et al. Positron emission tomography assessment of large vessel inflammation in patients with newly diagnosed, biopsy-proven giant cell arteritis: a prospective, case–control study. Ann Rheum Dis. 2014;73:1388–92.
Henes JC, Müller M, Krieger J, Balletshofer B, Pfannenberg AC, Kanz L, et al. [18F] FDG-PET/CT as a new and sensitive imaging method for the diagnosis of large vessel vasculitis. Clin Exp Rheumatol. 2008;26:S47–52.
Lensen KDF, Comans EFI, Voskuyl AE, Van Der Laken CJ, Brouwer E, Zwijnenburg AT, et al. Large-vessel vasculitis: Interobserver agreement and diagnostic accuracy of 18F-FDG-PET/CT. Biomed Res Int 2015. Article ID 914692.
Dasgupta B, Borg FA, Hassan N, Alexander L, Barraclough K, Bourke B, et al. BSR and BHPR guidelines for the management of giant cell arteritis. Rheumatology. 2010;49:1594–7.
Boellaard R, Delgado-Bolton R, Oyen WJG, Giammarile F, Tatsch K, Eschner W, et al. FDG PET/CT: EANM procedure guidelines for tumour imaging: version 2.0. Eur J Nucl Med Mol Imaging. 2015;42:328–54.
Mehta NN, Torigian DA, Gelfand JM, Saboury B, Alavi A. Quantification of atherosclerotic plaque activity and vascular inflammation using [18-F] fluorodeoxyglucose positron emission tomography/computed tomography (FDG-PET/CT). J Vis Exp 2012:e3777.
Soussan M, Nicolas P, Schramm C, Katsahian S, Pop G, Fain O, et al. Management of Large-Vessel Vasculitis with FDG-PET. Medicine (Baltimore). 2015;94:e622.
Besson FL, Parienti J-J, Bienvenu B, Prior JO, Costo S, Bouvard G, et al. Diagnostic performance of 18F-fluorodeoxyglucose positron emission tomography in giant cell arteritis: a systematic review and meta-analysis. Eur J Nucl Med Mol Imaging. 2011;38:1764–72.
Treglia G, Mattoli MV, Leccisotti L, Ferraccioli G, Giordano A. Usefulness of whole-body fluorine-18-fluorodeoxyglucose positron emission tomography in patients with large-vessel vasculitis: a systematic review. Clin Rheumatol. 2011;30:1265–75.
Mukhtyar C, Guillevin L, Cid MC, Dasgupta B, de Groot K, Gross W, et al. EULAR recommendations for the management of large vessel vasculitis. Ann Rheum Dis. 2009;68:318–23.
Clifford AH, Murphy EM, Burrell SC, Bligh MP, MacDougall RF, Heathcote JG, et al. Positron emission tomography/computerized tomography in newly diagnosed patients with Giant cell arteritis who are taking glucocorticoids. J Rheumatol. 2017;44:1859–66.
Meller J, Strutz F, Siefker U, Scheel A, Sahlmann CO, Lehmann K, et al. Early diagnosis and follow-up of aortitis with [18F]FDG PET and MRI. Eur J Nucl Med Mol Imaging. 2003;30:730–6.
Moosig F, Czech N, Mehl C, Henze E, Zeuner R, Kneba M, et al. Correlation between 18-fluorodeoxyglucose accumulation in large vessels and serological markers of inflammation in polymyalgia rheumatica: a quantitative PET study. Ann Rheum Dis. 2004;63:870–3.
Blockmans D, de Ceuninck L, Vanderschueren S, Knockaert D, Mortelmans L, Bobbaers H. Repetitive 18F-fluorodeoxyglucose positron emission tomography in giant cell arteritis: a prospective study of 35 patients. Arthritis Rheum. 2006;55:131–7.
Tarzi RM, Mason JC, Pusey CD. Issues in trial design for ANCA-associated and large-vessel vasculitis. Nat Rev Rheumatol. 2014;10:502–10.
Seeliger B, Sznajd J, Robson JC, Judge A, Craven A, Grayson PC, et al. Are the 1990 American College of Rheumatology vasculitis classification criteria still valid? Rheumatology. 2017;56:1154–61.
Unizony SH, Dasgupta B, Fisheleva E, Rowell L, Schett G, Spiera R, et al. Design of the tocilizumab in giant cell arteritis trial. Int J Rheumatol 2013;2013.
Langford CA, Cuthbertson D, Ytterberg SR, Khalidi N, Monach PA, Carette S, et al. A randomized, double-blind trial of Abatacept (CTLA-4Ig) for the treatment of Giant cell arteritis. Arthritis Rheumatol. 2017;69:837–45.
de Boysson H, Lambert M, Liozon E, Boutemy J, Maigné G, Ollivier Y, et al. Giant-cell arteritis without cranial manifestations. Medicine (Baltimore). 2016;95:e3818.
Förster S, Tato F, Weiss M, Czihal M, Rominger A, Bartenstein P, et al. Patterns of extracranial involvement in newly diagnosed giant cell arteritis assessed by physical examination, colour coded duplex sonography and FDG-PET. Vasa. 2011;40:219–27.
Lariviere D, Benali K, Coustet B, Pasi N, Hyafil F, Klein I, et al. Positron emission tomography and computed tomography angiography for the diagnosis of giant cell arteritis. Medicine (Baltimore). 2016;95:e4146.
Prieto-González S, Arguis P, García-Martínez A, Espígol-Frigolé G, Tavera-Bahillo I, Butjosa M, et al. Large vessel involvement in biopsy-proven giant cell arteritis: prospective study in 40 newly diagnosed patients using CT angiography. Ann Rheum Dis. 2012;71:1170–6.
Lehmann P, Buchtala S, Achajew N, Haerle P, Ehrenstein B, Lighvani H, et al. 18F-FDG PET as a diagnostic procedure in large vessel vasculitis-a controlled, blinded re-examination of routine PET scans. Clin Rheumatol. 2011;30:37–42.
Martínez-Rodríguez I, Martínez-Amador N, Banzo I, Quirce R, Jiménez-Bonilla J, De Arcocha-Torres M, et al. Assessment of aortitis by semiquantitative analysis of 180-min 18F-FDG PET/CT acquisition images. Eur J Nucl Med Mol Imaging. 2014;41:2319–24.
Besson FL, De Boysson H, Parienti JJ, Bouvard G, Bienvenu B, Agostini D. Towards an optimal semiquantitative approach in giant cell arteritis: an 18F-FDG PET/CT case-control study. Eur J Nucl Med Mol Imaging. 2014;41:155–66.
Hautzel H, Sander O, Heinzel A, Schneider M, Müller H-W. Assessment of large-vessel involvement in giant cell arteritis with 18F-FDG PET: introducing an ROC-analysis-based cutoff ratio. J Nucl Med. 2008;49:1107–13.
Acknowledgements
This work was funded by The Danish Rheumatism Association, Aarhus University, Aarhus University Hospital, Brødrene Hartmann Fond, A.P. Moeller Foundation, Aase & Ejnar Danielsen Foundation. We would like to thank Stine Kramer, MD, Nuclear Medicine and PET Centre, Aarhus University Hospital for scoring of in-treatment PET scans for reliability test; Aparna Udupi, statistician, Faculty of Health, Aarhus University for statistical advice; Morten Pilegaard, Associate Professor, Department of Business Communication, Aarhus University; Partner, Termshare A/S, Denmark and Anne-Birgitte Blavnsfeldt, MD, Department of Rheumatology, Aarhus University Hospital for editing the manuscript.
Disclaimers
The views expressed in the submitted article are the authors’ own and not an official position of the institution or funder.
Funding
This study was funded by The Danish Rheumatism Association, Aarhus University, Aarhus University Hospital, Brødrene Hartmann Foundation, A.P. Moeller Foundation, Aase & Ejnar Danielsen Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in the study were in accordance with the ethical standards of the National Committee on Health Research Ethics and with the 1964 Helsinki Declaration and its later amendments.
The Central Denmark Region Committees on Health Research Ethics (reference number 1–10–72-60-1) and The Danish Data Protection Agency (reference number 1–16–02-380-1) approved the study.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflicts of interests
Ellen-Margrethe Hauge has received fees for speaking from MSD, AbbVie, UCB and Sobi; and received research funding to Aarhus University Hospital from Roche and Novartis.
Rights and permissions
About this article
Cite this article
Nielsen, B.D., Gormsen, L.C., Hansen, I.T. et al. Three days of high-dose glucocorticoid treatment attenuates large-vessel 18F-FDG uptake in large-vessel giant cell arteritis but with a limited impact on diagnostic accuracy. Eur J Nucl Med Mol Imaging 45, 1119–1128 (2018). https://doi.org/10.1007/s00259-018-4021-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-018-4021-4