Abstract
Enteric hyperoxaluria is a common occurrence in the setting of fat malabsorption, usually due to intestinal resection or intestinal bypass surgery. Enhanced intestinal absorption of dietary oxalate leads to elevated renal oxalate excretion, frequently in excess of 100 mg/d (1.14 mmol/d). Patients are at increased risk of urolithiasis and loss of kidney function from oxalate nephropathy. Fat malabsorption causes increased binding of diet calcium by free fatty acids, reducing the calcium available to precipitate diet oxalate. Delivery of unabsorbed bile salts and fatty acids to the colon increases colonic permeability, the site of oxalate hyper-absorption in enteric hyperoxaluria. The combination of soluble oxalate in the intestinal lumen and increased permeability of the colonic mucosa leads to hyperoxaluria. Dietary therapy consists of limiting oxalate and fat intake. The primary medical intervention is the use of oral oxalate binding agents such as calcium salts to reduce free intestinal oxalate levels. Bile acid sequestrants can be useful in patients with ileal resection and bile acid malabsorption. Oxalate degrading bacteria provided as probiotics are being investigated but as of yet, no definite benefit has been shown with currently available preparations. The current state of medical therapy and potential future directions will be summarized in this article.



Similar content being viewed by others
Abbreviations
- BPD:
-
Biliopancreatic diversion
- EH:
-
Enteric hyperoxaluria
- JIB:
-
Jejunoileal bypass
- ODB:
-
Oxalate degrading bacteria
- RYGB:
-
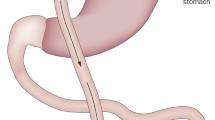
Roux-en-Y gastric bypass
References
Mole DR, Tomson CR, Mortensen N, Winearls CG (2001) Renal complications of jejuno-ileal bypass for obesity. QJM 94:69–77
Asplin JR, Coe FL (2007) Hyperoxaluria in kidney stone formers treated with modern bariatric surgery. J Urol 177:565–569
Nelson WK, Houghton SG, Milliner DS, Lieske JC, Sarr MG (2005) Enteric hyperoxaluria, nephrolithiasis, and oxalate nephropathy: potentially serious and unappreciated complications of Roux-en-Y gastric bypass. Surg Obes Relat Dis 1:481–485
Nasr SH, D’Agati VD, Said SM, Stokes MB, Largoza MV, Radhakrishnan J, Markowitz GS (2008) Oxalate nephropathy complicating Roux-en-Y gastric bypass: an underrecognized cause of irreversible renal failure. Clin J Am Soc Nephrol 3:1676–1683
Nguyen NT, Masoomi H, Magno CP, Nguyen XM, Laugenour K, Lane J (2011) Trends in use of bariatric surgery; 2003–2008. J Am Coll Surg 213:261–266
Holmes RP, Goodman HO, Assimos DG (2001) Contribution of dietary oxalate to urinary oxalate excretion. Kidney Int 59:270–276
Brinkley L, McGuire J, Gregory J, Pak CY (1981) Bioavailability of oxalate in foods. Urology 17:534–538
Hess B, Jost C, Zipperle L, Takkinen R, Jaeger P (1998) High-calcium intake abolishes hyperoxaluria and reduces urinary crystallization during a 20-fold normal oxalate load in humans. Nephrol Dial Transplant 13:2241–2247
Liebman M, Chai W (1997) Effect of dietary calcium on urinary oxalate excretion after oxalate loads. Am J Clin Nutr 65:1453–1459
Chen Z, Ye Z, Zeng L, Yang W (2003) Clinical investigation on gastric oxalate absorption. Chin Med J (Engl) 116:1749–1751
Smith LH, Fromm H, Hofmann AF (1972) Acquired hyperoxaluria, nephrolithiasis, and intestinal disease. Description of a syndrome. N Engl J Med 286:1371–1375
Dowling RH, Rose GA, Sutor DJ (1971) Hyperoxaluria and renal calculi in ileal disease. Lancet 1:1103–1106
Barilla DE, Notz C, Kennedy D, Pak CY (1978) Renal oxalate excretion following oral oxalate loads in patients with ileal disease and with renal and absorptive hypercalciurias. Effect of calcium and magnesium. Am J Med 64:579–585
Chadwick VS, Modha K, Dowling RH (1973) Mechanism for hyperoxaluria in patients with ileal dysfunction. N Engl J Med 289:172–176
Earnest DL, Johnson G, Williams HE, Admirand WH (1974) Hyperoxaluria in patients with ileal resection: an abnormality in dietary oxalate absorption. Gastroenterology 66:1114–1122
Froeder L, Arasaki CH, Malheiros CA, Baxmann AC, Heilberg IP (2012) Response to dietary oxalate after bariatric surgery. Clin J Am Soc Nephrol 7:2033–2040
Dobbins JW, Binder HJ (1977) Importance of the colon in enteric hyperoxaluria. N Engl J Med 296:298–301
Modigliani R, Labayle D, Aymes C, Denvil R (1978) Evidence for excessive absorption of oxalate by the colon in enteric hyperoxaluria. Scand J Gastroenterol 13:187–192
Earnest DL, Williams HE, Admirand WH (1975) A physicochemical basis for treatment of enteric hyperoxaluria. Trans Assoc Am Physicians 88:224–234
Dobbins JW, Binder HJ (1976) Effect of bile salts and fatty acids on the colonic absorption of oxalate. Gastroenterology 70:1096–1100
Parks JH, Worcester EM, O’Connor RC, Coe FL (2003) Urine stone risk factors in nephrolithiasis patients with and without bowel disease. Kidney Int 63:255–265
Maalouf NM, Tondapu P, Guth ES, Livingston EH, Sakhaee K (2010) Hypocitraturia and hyperoxaluria after Roux-en-Y gastric bypass surgery. J Urol 183:1026–1030
Hamm LL (1990) Renal handling of citrate. Kidney Int 38:728–735
Puzziferri N, Blankenship J, Wolfe BM (2006) Surgical treatment of obesity. Endocrine 29:11–19
Gregory JG, Park KY, Schoenberg HW (1977) Oxalate stone disease after intestinal resection. J Urol 117:631–634
Pang R, Linnes MP, O’Connor HM, Li X, Bergstralh E, Lieske JC (2012) Controlled metabolic diet reduces calcium oxalate supersaturation but not oxalate excretion after bariatric surgery. Urology 80:250–254
Andersson H, Jagenburg R (1974) Fat-reduced diet in the treatment of hyperoxaluria in patients with ileopathy. Gut 15:360–366
Nordenvall B, Backman L, Burman P, Larsson L, Tiselius HG (1983) Low-oxalate, low-fat dietary regimen in hyperoxaluria following jejunoileal bypass. Acta Chir Scand 149:89–91
Caspary WF, Tonissen J, Lankisch PG (1977) ‘Enteral’ hyperoxaluria. Effect of cholestyramine, calcium, neomycin, and bile acids on intestinal oxalate absorption in man. Acta Hepatogastroenterol (Stuttg) 24:193–200
Hylander E, Jarnum S, Nielsen K (1980) Calcium treatment of enteric hyperoxaluria after jejunoileal bypass for morbid obesity. Scand J Gastroenterol 15:349–352
Stauffer JQ (1977) Hyperoxaluria and intestinal disease. The role of steatorrhea and dietary calcium in regulating intestinal oxalate absorption. Am J Dig Dis 22:921–928
Walker VR, Sutton RA (1994) Calcium supplementation for enteric hyperoxaluria secondary to intestinal bypass. In: Ryall R, Bais R, Marshall VR, Rofe AM, Smith LH, Walker VR (eds) Urolithiasis 2. Plenum, New York, pp 557–561
Rodgers AL, Allie-Hamdulay S, Jackson GE, Sutton RA (2014) Enteric hyperoxaluria secondary to small bowel resection: use of computer simulation to characterize urinary risk factors for stone formation and assess potential treatment protocols. J Endourol 28:985–994
Tondapu P, Provost D, Adams-Huet B, Sims T, Chang C, Sakhaee K (2009) Comparison of the absorption of calcium carbonate and calcium citrate after Roux-en-Y gastric bypass. Obes Surg 19:1256–1261
Sakhaee K, Griffith C, Pak CY (2012) Biochemical control of bone loss and stone-forming propensity by potassium-calcium citrate after bariatric surgery. Surg Obes Relat Dis 8:67–72
Zimmermann DJ, Voss S, Von Unruh GE, Hesse A (2005) Importance of magnesium in absorption and excretion of oxalate. Urol Int 74:262–267
Liebman M, Costa G (2000) Effects of calcium and magnesium on urinary oxalate excretion after oxalate loads. J Urol 163:1565–1569
Nordenvall B, Backman L, Larsson L, Tiselius HG (1983) Effects of calcium, aluminium, magnesium and cholestyramine on hyperoxaluria in patients with jejunoileal bypass. Acta Chir Scand 149:93–98
Lieske JC, Regnier C, Dillon JJ (2008) Use of sevelamer hydrochloride as an oxalate binder. J Urol 179:1407–1410
Braunlin W, Zhorov E, Guo A, Apruzzese W, Xu Q, Hook P, Smisek DL, Mandeville WH, Holmes-Farley SR (2002) Bile acid binding to sevelamer HCl. Kidney Int 62:611–619
Robijn S, Vervaet BA, Hoppe B, D’Haese PC, Verhulst A (2013) Lanthanum carbonate inhibits intestinal oxalate absorption and prevents nephrocalcinosis after oxalate loading in rats. J Urol 189:1960–1966
Binder HJ (1974) Intestinal oxalate absorption. Gastroenterology 67:441–446
Stauffer JQ, Humphreys MH, Weir GJ (1973) Acquired hyperoxaluria with regional enteritis after ileal resection. Role of dietary oxalate. Ann Intern Med 79:383–391
Allison MJ, Dawson KA, Mayberry WR, Foss JG (1985) Oxalobacter formigenes gen. nov., sp. nov.: oxalate-degrading anaerobes that inhabit the gastrointestinal tract. Arch Microbiol 141:1–7
Kaufman DW, Kelly JP, Curhan GC, Anderson TE, Dretler SP, Preminger GM, Cave DR (2008) Oxalobacter formigenes may reduce the risk of calcium oxalate kidney stones. J Am Soc Nephrol 19:1197–1203
Mittal RD, Kumar R, Mittal B, Prasad R, Bhandari M (2003) Stone composition, metabolic profile and the presence of the gut-inhabiting bacterium Oxalobacter formigenes as risk factors for renal stone formation. Med Princ Pract 12:208–213
Hatch M, Cornelius J, Allison M, Sidhu H, Peck A, Freel RW (2006) Oxalobacter sp. reduces urinary oxalate excretion by promoting enteric oxalate secretion. Kidney Int 69:691–698
Jiang J, Knight J, Easter LH, Neiberg R, Holmes RP, Assimos DG (2011) Impact of dietary calcium and oxalate, and Oxalobacter formigenes colonization on urinary oxalate excretion. J Urol 186:135–139
Kumar R, Ghoshal UC, Singh G, Mittal RD (2004) Infrequency of colonization with Oxalobacter formigenes in inflammatory bowel disease: possible role in renal stone formation. J Gastroenterol Hepatol 19:1403–1409
Allison MJ, Cook HM, Milne DB, Gallagher S, Clayman RV (1986) Oxalate degradation by gastrointestinal bacteria from humans. J Nutr 116:455–460
Duffey BG, Miyaoka R, Holmes R, Assimos D, Hinck B, Korman E, Kieley F, Ikramuddin S, Kellogg T, Moeding A, Monga M (2011) Oxalobacter colonization in the morbidly obese and correlation with urinary stone risk. Urology 78:531–534
Campieri C, Campieri M, Bertuzzi V, Swennen E, Matteuzzi D, Stefoni S, Pirovano F, Centi C, Ulisse S, Famularo G, De Simone C (2001) Reduction of oxaluria after an oral course of lactic acid bacteria at high concentration. Kidney Int 60:1097–1105
Lieske JC, Tremaine WJ, De SC, O’Connor HM, Li X, Bergstralh EJ, Goldfarb DS (2010) Diet, but not oral probiotics, effectively reduces urinary oxalate excretion and calcium oxalate supersaturation. Kidney Int 78:1178–1185
Goldfarb DS, Modersitzki F, Asplin JR (2007) A randomized, controlled trial of lactic acid bacteria for idiopathic hyperoxaluria. Clin J Am Soc Nephrol 2:745–749
Lieske JC, Goldfarb DS, De Simone C, Regnier C (2005) Use of a probiotic to decrease enteric hyperoxaluria. Kidney Int 68:1244–1249
McDonald GB, Earnest DL, Admirand WH (1977) Hyperoxaluria correlates with fat malabsorption in patients with sprue. Gut 18:561–566
Singh A, Sarkar SR, Gaber LW, Perazella MA (2007) Acute oxalate nephropathy associated with orlistat, a gastrointestinal lipase inhibitor. Am J Kidney Dis 49:153–157
Dhar NB, Grundfest S, Jones JS, Streem SB (2005) Jejunoileal bypass reversal: effect on renal function, metabolic parameters and stone formation. J Urol 174:1844–1846
Economou TP, Cullen JJ, Mason EE, Scott DH, Doherty C, Maher JW (1995) Reversal of small intestinal bypass operations and concomitant vertical banded gastroplasty: long-term outcome. J Am Coll Surg 181:160–164
Semins MJ, Asplin JR, Steele K, Assimos DG, Lingeman JE, Donahue S, Magnuson T, Schweitzer M, Matlaga BR (2010) The effect of restrictive bariatric surgery on urinary stone risk factors. Urology 76:826–829
Semins MJ, Matlaga BR, Shore AD, Steele K, Magnuson T, Johns R, Makary MA (2009) The effect of gastric banding on kidney stone disease. Urology 74:746–749
Frolkis AD, Dykeman J, Negron ME, Debruyn J, Jette N, Fiest KM, Frolkis T, Barkema HW, Rioux KP, Panaccione R, Ghosh S, Wiebe S, Kaplan GG (2013) Risk of surgery for inflammatory bowel diseases has decreased over time: a systematic review and meta-analysis of population-based studies. Gastroenterology 145:996–1006
Ceulemans LJ, Nijs Y, Nuytens F, De HG, Claes K, Bammens B, Naesens M, Evenepoel P, Kuypers D, Vanrenterghem Y, Monbaliu D, Pirenne J (2013) Combined kidney and intestinal transplantation in patients with enteric hyperoxaluria secondary to short bowel syndrome. Am J Transplant 13:1910–1914
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
No funding was provided in support of this work.
Conflict of interest
John Asplin is an employee of Litholink/LabCorp, a company that provides laboratory testing for patients with kidney stones.
Ethical approval
This article does not contain any studies with animals performed by any of the authors.
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Asplin, J.R. The management of patients with enteric hyperoxaluria. Urolithiasis 44, 33–43 (2016). https://doi.org/10.1007/s00240-015-0846-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00240-015-0846-5