Abstract
Summary
In elderly women with osteoporosis, prior fracture, low BMD, impaired physical functioning, poorer general health, and recent falls were all direct predictors of imminent (in next year) fracture risk. Prior fracture, older age, worse health, impaired cognitive functioning, and recent falls indirectly increased imminent risk by reducing physical functioning/general health.
Introduction
This study was designed to examine determinants of imminent risk of osteoporotic fracture (i.e., next 1–2 years) in postmenopausal women.
Methods
This retrospective cohort study used data from Caucasian women age 65 or older with osteoporosis who participated in the observational Study of Osteoporotic Fractures (SOF). We examined potential direct and indirect predictors of hip and nonvertebral fractures in 1-year follow-up intervals including anthropometric measures, bone mineral density (T-score), fracture since age 50, physical function, cognition, medical conditions, recent (past year) falls, and lifestyle factors. Clinically related variables were grouped into constructs via factor analysis. These constructs and selected individual variables were incorporated into a theoretical structural equation model to evaluate factors that influence imminent risk.
Results
Among 2261 patients, 19.4% had a nonvertebral fracture and 5.5% had a hip fracture within 1 year of a study visit between 1992 and 2008. Prior fracture, lower T-scores, lower physical functioning, and recent falls all directly increased 1-year risk of nonvertebral fracture. For both nonvertebral and hip fractures, prior fracture and recent falls influenced risk indirectly through general health, while cognition influenced risk via physical functioning. Age influenced both physical functioning and general health.
Conclusions
Several established risk factors for 10-year fracture risk also played a role in predicting imminent risk of fracture (e.g., T-scores, prior fracture), as did falls, cognition, physical functioning, and general health. Fracture risk assessments should also consider falls and fall risk factors as well as established bone-related risk factors in assessing imminent fracture risk.
Similar content being viewed by others
Introduction
Osteoporotic fractures are associated with direct patient burden in terms of morbidity and mortality and also exert a significant societal economic burden stemming from direct healthcare resource use (hospitalizations, outpatient visits, prescription medication, rehabilitation, and long-term care), direct nonmedical costs (transportation, caregivers), and indirect costs (time and work impact on family caregivers, lost patient productivity, early retirement) [1,2,3,4,5,6]. Despite the magnitude of these clinical and economic burdens and the availability of effective treatments, osteoporosis is often undertreated. Suboptimal treatment is an issue even among women with a history of osteoporotic fracture, whose risk is particularly elevated for another fracture. As few as one of every four Medicare patients in the USA received treatment after fracture [7, 8].
Several factors have been associated with an increasing risk of fracture in postmenopausal women with osteoporosis. Prior fracture is a key risk factor for subsequent fracture [9,10,11]. Fracture risk is also known to increase with advancing age, low bone mineral density (BMD), and greater risk or history of falls [12, 13]. Certain pharmacologic therapies, such as glucocorticoids, and medical conditions increase the risk of secondary osteoporosis and related fractures through their direct impact on bone density or structure [14,15,16,17]. In addition, specific conditions and medications increase fracture risk indirectly through mobility and/or physical, cognitive, visual, and sensory deficits that increase the risk of falls [18].
Clinical risk assessment tools incorporate many of the aforementioned risk factors with the goal of predicting the risk of fracture over periods of 5–10 years. However, it is increasingly appreciated that fracture risk varies over time as an individual’s health status varies and the interplay of risk factors may differ for imminent (i.e., in the next 1–2 years) and long-term risk. Although there is a growing body of literature documenting the effect of factors that influence the 1- to 2-year risk of fracture, the relationships among the factors that shape the imminent risk of fracture are not yet well understood. While some risk factors may directly influence fracture risk, risk factors may also be interrelated and/or influence other direct risk factors. The aim of our study was to identify risk factors for imminent fracture in postmenopausal women with osteoporosis and to describe their role in directly or indirectly influencing imminent risk of fracture either independently or as part of a group of related factors. In addition, the more complete understanding of how specific factors influence imminent risk of fracture may also provide insights into how often risk assessments should be performed in order to capture important changes related to key risk factors in a timely fashion.
Methods
In this study, we used structural equation modeling (SEM) to examine the relationships between patient characteristics (e.g., demographics, clinical characteristics, lifestyle, physical functioning) and imminent risk for hip and nonvertebral fractures among elderly postmenopausal women with osteoporosis. We focused on a 1-year period to evaluate imminent risk in this study.
Study design and data source
This retrospective study used data from the Study of Osteoporotic Fractures (SOF), which is a multicenter observational study. The SOF includes approximately 20 years of prospective data that have served as the basis for studies of osteoporosis and aging. SOF participants underwent examinations every 2 years between the first and sixth visits and were examined approximately every 4 years thereafter. Data on BMD, body weight, cognitive function, lifestyle, medical history, medication use, physical function and performance, quality of life, sleep, vision, and vital signs were collected at these examination visits, although not all assessments were performed at each visit. Participants also reported on falls and fractures three times per year during the study.
Our study used data collected on Exam #4 (1992–1994), Exam #5 (1995–1996), Exam #6 (1997–1998), Exam #8 (2002–2004), and Exam #9 (2006–2008), as well as data from the triannual questionnaires administered between these examinations. Observations from Exams #1–3 and Exam #7 were excluded because data on time-dependent risk factors (e.g., medication use) were not collected at these examinations.
Study population
The original SOF cohort was enrolled in 1986 and included 9704 US (primarily Caucasian) women aged ≥ 65 years; 662 African-American elderly women were added in 1997 [16]. For this evaluation, the study population comprised a subset of the overall SOF cohort and included Caucasian women who had osteoporosis (defined in this study as T-score ≤ −2.5 at the total hip) at any of the five examinations evaluated. For each participant, each examination constituted a separate baseline at which potential risk factors for fracture were determined and from which subsequent fracture incidence was determined. Study subjects could contribute up to five observations in total—one for each qualifying examination—and all observations were pooled for analysis.
Study outcomes
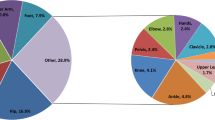
The primary outcomes were hip fracture and nonvertebral fracture (including hip), as defined in the SOF. Fracture incidence was assessed for a 1-year period that began on the day after the date of each qualifying examination and extended through the earliest of 365 days, loss to follow-up, or death. The hip fracture outcome was defined as an incident, nontraumatic fracture of the femoral neck, intertrochanteric line, or other hip-related site. Nonvertebral fractures were captured in a SOF-defined composite measure of incident nontraumatic fracture of the ankle, clavicle, elbow, face, foot, finger, hand, heel, hip, humerus, knee, lower leg, pelvis, rib, toe, upper leg, or wrist. Only fractures confirmed via an adjudication process conducted by SOF investigators were included in our analysis.
Potential risk factors
Potential risk factors examined included demographics and anthropometrics; BMD (T-score); prior fracture any time after age 50 years; cardiac, cognitive, metabolic, and physical conditions and related medications; recent fall history (last 12 months); lifestyle (e.g., smoking status, exercise); and physical functioning and performance (e.g., instrumental activities of daily living [IADL], chair stand, walking speed).
Statistical analysis
We used a two-step analysis strategy for this study. In the first step, exploratory factor analysis (EFA) and a series of independent single-factor confirmatory factor analysis (CFA) models were used to determine whether related variables should be grouped or tested individually in the models of fracture risk. EFA is a statistical method for identifying related predictors and grouping them into overarching constructs. Each construct represents a single risk factor, aspects of which may be quantified by different variables that can be directly observed (e.g., IADL, walking speed, and time to perform chair stands may collectively represent physical functioning). In our study, EFA was used primarily to confirm an a priori grouping of variables, which was informed by the existing literature and expert opinion. CFA was used to evaluate how well the available observed variables measured one or more constructs and to assess the degree to which relationships in the observed data conformed to the theoretical expectations.
In the second step of the analysis, we built on results of the individual CFAs by testing a broader theoretical model of imminent risk of fracture using SEM, a statistical framework that supports the simultaneous evaluation of multiple interrelations among constructs and observed variables. The separate models developed for hip and nonvertebral fractures reflected hypothesized causal pathways that were based on risk factor relationships established in prior clinical and geriatric research publications and expert medical opinion.
Data management and descriptive analyses were conducted using SAS 9.4 (SAS Institute, Cary, NC). All models (EFAs, CFAs, and SEMs) were estimated in Mplus 6.11 (Muthén & Muthén, Los Angeles, CA) using weighted least squares means and variance adjusted and accounted for the nonindependence created by pooling all visits (multiple observations per subject) using the Huber–White sandwich estimator [19]. EFA used Crawford–Ferguson oblique quartimax rotation [20] to rotate initial values to more interpretable solutions. Confirmatory models were evaluated using the root mean square error of approximation (RMSEA), Tucker–Lewis Index (TLI), and comparative fit index (CFI). To assess model fit, we used the cut-points of CFI > 0.95, TLI > 0.95, and RMSEA < 0.08 [21, 22]. The unadjusted, two-tailed alpha level of 0.05 was used to determine statistical significance for individual parameters of the CFAs and SEMs.
Results
The study population included 2261 postmenopausal women who contributed 8128 observations. Selected patient characteristics based on data collected at SOF Exam #4 (the first assessment from which study data were obtained) are presented in Table 1. Patient ages ranged from 70 to 93 years, with a mean age of 77.9 (standard deviation [SD]: 5.1). The mean total hip T-score among those with diagnosed osteoporosis (N = 2048) was −2.8 (SD: 0.6), and 57% of patients had a history of fracture since age 50 years. During the study period (1992–2008), 5.5% (125/2261) of women in the sample had a qualifying hip fracture, and 19.4% (438/2261) experienced a nonvertebral fracture. On average, annually, approximately 6.4% of study participants had a nonvertebral fracture, and 1.7% had a hip fracture. Approximately 10% (44/438) of women who experienced any qualifying nonvertebral fractures reported a nonvertebral fracture in more than one follow-up interval (i.e., experienced a subsequent fracture in one of the designated observation periods). No women in the study population contributed multiple hip fractures to the analysis. Data from SOF Exam #4 indicates that 32% of 2247 women had fallen since their previous study visit.
In the first step of the analysis, after obtaining clinical input into constructs that would be expected to underlie related measures that are quantified in the SOF database, we focused on three a priori constructs: (1) cognitive functioning, (2) physical functioning, and (3) general health. We used EFA to evaluate these three constructs plus an additional factor that allowed for assessment of unanticipated relationships (Online Resource 1). Cognition was best represented by grouping the individual variables of completing the Trails B exam in 3 min, the Mini-Mental State Exam score, and whether the patient had ever been diagnosed with Alzheimer’s disease. Physical functioning was best represented by grouping individual variables for patients’ self-report of walking for exercise; observed walking speed, time to complete a chair sit to stand test, and grip strength; and the IADL five-item functional disability score. General health was best represented by variables for self-reported health compared with other people, as well as current treatment for hypertension, myocardial infarction, stroke, congestive heart failure, diabetes, chronic obstructive pulmonary disease, or arthritis. Current treatment for hyperthyroidism and Parkinson’s disease, however, did not meet the threshold for inclusion in the general health variable based on factor loading results. Results for the “other” factor in the model suggested that a metabolic construct could potentially be represented by body mass index, diabetes treatment, and hip T-score. However, the metabolic variable was not included since diabetes had a stronger association with the general health variable. Given the expected association between BMD and fracture risk and the completeness of BMD data, the decision was made to test T-score at total hip as an independent risk factor in the fracture risk models.
Confirmatory factor models were specified for the cognition, physical functioning, and general health variables based on the EFA results. Figure 1 presents the standardized factor loadings for these three variables. As the cognition model was identified with three individual variables (Trails B completion in 3 min, Mini-Mental State Exam, and Alzheimer’s disease), model fit was perfect (Fig. 1a; RMSEA = 0.00, CFI = 1.00, TLI = 1.00); higher values on this construct indicate more robust cognitive function. The confirmatory model for physical functioning defined by five individual variables (walk for exercise, IADL five-item functional disability score, grip strength, walking speed, and timed chair stands) fitted well to the data (Fig. 1b; RMSEA = 0.05, CFI = 0.99, TLI = 0.99); higher values on the physical functioning construct indicate greater functionality. The general health confirmatory model initially included all variables indicated by the EFA results but fit poorly, and modification indices indicated the possibility of a subfactor related to heart disease, with correlations observed among the variables for myocardial infarction, hypertension, and congestive heart failure. To maintain a unidimensional model of general health, the congestive heart failure and hypertension variables were dropped from the model, while the myocardial infarction variable was retained. The final revised confirmatory model of the general health variable, which included six variables (myocardial infarction, stroke, diabetes, chronic obstructive pulmonary disease, arthritis, and self-reported health compared to others), provided reasonably good fit to the data (Fig. 1c; RMSEA = 0.02; CFI = 0.95, TLI = 0.92); higher values on the general health construct indicate poorer health.
Individual variables comprising constructs. a Cognition measurement model including standardized factor loading coefficients. All factor loading coefficients were significant at p < 0.001. b Physical functioning measurement model including standardized factor loading coefficients. All factor loading coefficients were significant at p < 0.001. c General health measurement model including standardized factor loading coefficients. All factor loading coefficients were significant at p < 0.001. COPD chronic obstructive pulmonary disease, IADL instrumental activities of daily living
The constructs of cognition, physical functioning, and general health, as well as relevant individual variables (age, T-score at total hip, history of fracture since age 50, and recent falls), were tested as potential risk factors for imminent fracture, with separate hypothetical models developed for hip and nonvertebral fractures (Fig. 2, Fig. 3). Physical functioning was the strongest direct predictor, with impairments in physical function associated with increased fracture risk (p < 0.001) in both models. History of fracture was indirectly associated with significant increases in imminent hip fracture risk, exerting its influence by worsening patients’ general health (p < 0.001). Worse general health was an indirect contributor to imminent risk of hip fractures, exerting a negative influence on physical functioning (p < 0.001). Better cognition indirectly protected against imminent risk of hip fracture, acting through its influence on physical functioning. Recent falls were a significant predictor of worse general health (p < 0.001), but the direct path between recent falls and imminent risk of fracture and between recent falls and physical functioning did not achieve statistical significance in this study. Finally, age exerted an indirect influence on imminent risk of hip fracture by significant (p < 0.001) associations with physical functioning (increasing age associated with decreasing physical function) and general health (increasing age associated with worse general health).
Five factors had a direct, statistically significant influence on the imminent risk of nonvertebral fractures (Fig. 3). Lower BMD and impaired/worse physical functioning were associated with increased fracture risk (both p < 0.001). Recent falls and history of fracture were also associated with increased fracture risk (p < 0.001 and p < 0.05, respectively). General health was directly related to the risk of nonvertebral fracture but exerted its greatest influence by reducing physical functioning (p < 0.001). Age, history of fracture, and recent falls also influenced fracture risk indirectly by reducing physical functioning and/or contributing to worsening general health. Better cognition exerted a strong protective influence, working indirectly through improved physical functioning.
Discussion
Our findings suggest that clinicians may have an opportunity to identify postmenopausal women with osteoporosis who are at high imminent risk of fracture, defined in this study as risk for fracture in the next year, by focusing on BMD (T-score at total hip), fracture history, and fall history, as well as factors affecting physical functioning and general health. These factors directly influenced the risk of nonvertebral fracture in the next year. The direct association of falls and hip fractures did not achieve statistical significance in our model, which may be related to sample size considerations, including the number of study patients reporting falls and the low number of hip fracture events. In addition to their role as direct risk factors in nonvertebral fractures, recent falls and fracture history increased 1-year risk of fracture indirectly through their negative impact on general health and/or physical functioning. Advancing age was significantly associated with decreased physical functioning and worse general health in models of both hip fracture risk and nonvertebral fracture risk, while better cognition was significantly associated with better physical functioning in both models. General health also acted as an indirect risk factor for imminent fractures, with worse health associated with reduced physical functioning.
While there is no broadly accepted definition of imminent fracture risk, we chose to focus on factors predicting fracture in the next year to add to the literature on assessing risk over a shorter time frame, in contrast to the traditional longer-term fracture risk prediction framework. Our findings align well with the growing body of literature on imminent risk of fracture, including observational studies which have consistently identified low BMD, prior fractures, age, poor health status, previous falls, specific comorbidities that influence physical and cognitive functioning (both of which are risk factors for falls), as well as other fall-related risk factors, as key predictors of the imminent risk of fracture [18, 23,24,25,26,27,28].
In the last decade, fracture risk assessment tools have assisted physicians in identifying individuals at high risk and in making decisions regarding the treatment of osteoporosis [29]. While these tools provide important clinical insights, they do not include some important risk factors, such as fall history, which may lead to underestimation of risk [30,31,32]. For example, the developers of FRAX® (University of Sheffield, UK) have noted that the tool underestimates fracture risk in patients with frequent falls by as much as 30% for each additional fall in the preceding year, although there is ongoing consideration for adding falls to this tool in the future [33]. FRAX® also does not yet account for how recent a prior fracture was in estimating fracture risk and does not distinguish the potentially differing impact on risk over shorter and longer time horizons. Including falls and/or accounting for the recency of prior fracture may increase the sensitivity of fracture prediction by identifying additional patients at increased risk for imminent fracture.
Our models show that most of the predictors of imminent risk include characteristics that reflect health status, which is likely to change over time, particularly in older individuals. This is consistent with a growing body of literature suggesting that an individual’s fracture risk is dynamic, in that it varies over time and may be dependent on the specific combinations of risk factors that are present [18, 23,24,25,26,27]. Given that health status changes and medical events (e.g., myocardial infarction, stroke, Alzheimer’s diagnosis) that affect factors such as physical functioning occur more frequently with increasing age, annual assessments of fracture risk would likely help better identify those patients most at imminent risk of fracture and support improved management of fracture risk in these patients [18, 23, 27]. Annual assessments would reduce the risk that changes in key health factors would be missed, and that fracture risk would be underestimated.
Information on imminent risk may inform the choice of treatment (selection of agent[s] with rapid effects), timing of treatment initiation based upon risk, and approaches to sequencing therapy. For example, for patients in whom there is particular urgency to build BMD and quickly reduce fracture risk, a bone-forming agent may be prescribed prior to transitioning the patient to an antiresorptive therapy—an approach validated by the recent VERO and ARCH studies of teriparatide (Forteo, Eli Lilly, Indianapolis, IN) and romosozumab (Evenity, Amgen, Thousand Oaks, CA), respectively [34, 35]. Roux and Briot [36] have offered a framework for understanding and using information on imminent risk in the routine care setting, and a 2019 paper by Pinedo-Villanueva et al. [37] has recommended the assessment of imminent risk in the fracture liaison service (FLS) setting to identify the patients most in need of treatment with potent anti-osteoporosis medications with a rapid onset of action. Imminent risk assessment may also help clinicians tailor other patient support efforts, such as education on fall prevention and management of comorbidities and medications that may increase risk for fracture.
The current study used SEM, a methodology commonly used in the social sciences, to elucidate relationships among factors that influence the imminent risk for fracture in older women with osteoporosis. Our models allowed us to identify factors that directly influence the risk of fracture in the next year, as well as factors that work through causal pathways to influence fracture risk. The capacity to identify these indirect risk factors is particularly important to gaining a more complete understanding of the risk prediction for imminent fracture (e.g., prior fracture not only may influence fracture risk directly but also may confer additional fracture risk by reducing a patient’s physical functioning). A strength of our SEM approach is the ability to incorporate clinical constructs, which reduces the potential for measurement error that may arise when relying on a single measure to quantify a particular factor, into the model. For example, in our models, five different variables are included as indicators for the physical functioning construct. Because we used SEM, the common “physical functioning” variance is separated from item-specific variance in the analyses, and only that common variance is used as a variable, providing a more targeted estimate of the true relationships between, in this example, physical functioning and the imminent risk of fracture. Although the study methodology is complex, the results of the models clearly show factors that are important predictors of the imminent risk of fracture. For the clinician, this indicates the importance of considering these factors to assess short-term risk and intervening to reduce fracture risk when appropriate.
Our study has some limitations. First, our study population comprises self-selected, elderly, community-dwelling female volunteers lacking in racial and ethnic diversity, which limits the generalizability of our results. Women with osteoporosis (T-score ≤ −2.5 at total hip) were underrepresented in SOF (17% of SOF versus 25% of the US female population are ≥ 65 years old) [38], and SOF does not include data on postmenopausal women with osteoporosis who are under age 65. Our use of the hip T-score to identify patients with osteoporosis also did not allow for selection of patients who may have met a diagnosis of osteoporosis based on other clinical characteristics (e.g., osteopenia and history of osteoporotic fracture). Changes in practice patterns, technology, and other unobservable factors since 1986 (the year SOF commenced) may also have implications for the generalizability of our findings to the current osteoporosis care landscape. Key data elements (e.g., family and personal medical history, lifestyle) in this study were obtained through self-report, and recall bias may have influenced the accuracy of these data. Fall data were also collected at different intervals than those used for the main data elements, and the SOF study design did not allow for validation of those data. Given the available data, we did not directly model the impact of recent fracture or the specific timing of recent falls nor were we able to rigorously assess for the effect of changes in medications that may impact risk of fracture (e.g., corticosteroids, opioids, antihypertensives, which may impact risk for fracture via increasing risk for falls or direct effects on bone). We also acknowledge that SEM is essentially a hypothesis-testing methodology that supported our initial identification of important direct and indirect risk factors. The risk factors and relationships described here, however, need to be confirmed and validated using additional analytic techniques and data from other large osteoporosis populations. Lastly, we did not assess risk factors or explicitly determine fracture risk in the time period following the 1-year observation periods after each qualifying examination to confirm how relative or absolute risk change over time in this SOF population.
In summary, factors that influence the imminent risk of fracture are dynamic and exhibit complex, yet clinically intuitive, interrelationships. This research reinforces literature that has established the importance of BMD, prior fracture, recent falls, physical functioning, age, cognition, and general health in their roles as direct and/or indirect risk factors for imminent hip and nonvertebral fractures. Our findings also suggest that osteoporosis care may be improved by routinely monitoring these potential risk factors in order to more expediently identify postmenopausal women with osteoporosis who are at imminent risk for fracture and tailor treatment accordingly.
References
Bliuc D, Nguyen ND, Nguyen TV, Eisman JA, Center JR (2013) Compound risk of high mortality following osteoporotic fracture and refracture in elderly women and men. J Bone Miner Res 28:2317–2324
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A (2007) Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res 22:465–475
Pike CT, Birnbaum HG, Schiller M, Swallow E, Burge RT, Edgell ET (2011) Prevalence and costs of osteoporotic patients with subsequent non-vertebral fractures in the US. Osteoporos Int 22:2611–2621
Hall SE, Williams JA, Senior JA, Goldswain PR, Criddle RA (2000) Hip fracture outcomes: quality of life and functional status in older adults living in the community. Aust N Z J Med 30:327–332
Kanis JA, Borgström F, Compston J, Dreinhöfer K, Nolte E, Jonsson L, Lems WF, McCloskey EV, Rizzoli R, Stenmark J (2013) SCOPE: a scorecard for osteoporosis in Europe. Arch Osteoporos 8:144
Tajeu GS, Delzell E, Smith W, Arora T, Curtis JR, Saag KG, Morrisey MA, Yun H, Kilgore ML (2014) Death, debility, and destitution following hip fracture. J Gerontol A Biol Sci Med Sci 69:346–353
Yusuf AA, Matlon TJ, Grauer A, Barron R, Chandler D, Peng Y (2016) Utilization of osteoporosis medication after a fragility fracture among elderly Medicare beneficiaries. Arch Osteoporos 11:31
Yang X, Sajjan S, Modi A (2016) High rate of non-treatment among osteoporotic women enrolled in a US Medicare plan. Curr Med Res Opin 32:1849–1856
International Osteoporosis Foundation (2012) Capture the Fracture: a global campaign to break the fragility fracture cycle. http://www.capturethefracture.org/. Accessed 03 February 2018
Johnell O, Kanis JA, Odén A, Sernbo I, Redlund-Johnell I, Petterson C, De Laet C, Jönsson B (2004) Fracture risk following an osteoporotic fracture. Osteoporos Int 15:175–179
Kanis JA, Johnell O, De Laet C et al (2004) A meta-analysis of previous fracture and subsequent fracture risk. Bone 35:375–382
Kanis JA, Johnell O, Oden A, Johansson H, McCloskey E (2008) FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int 19:385–397
Lewiecki EM, Baron R, Bilezikian JP, Gagel RE, Leonard MB, Leslie WD, McClung MR, Miller PD (2016) Proceedings of the 2015 Santa Fe bone symposium: clinical applications of scientific advances in osteoporosis and metabolic bone disease. J Clin Densitom 19:102–116
Balasubramanian A, Wade SW, Adler RA, Lin CJF, Maricic M, O'Malley CD, Saag K, Curtis JR (2016) Glucocorticoid exposure and fracture risk in patients with new-onset rheumatoid arthritis. Osteoporos Int 27:3239–3249
van Staa TP, Leufkens HG, Abenhaim L, Zhang B, Cooper C (2000) Oral corticosteroids and fracture risk: relationship to daily and cumulative doses. Rheumatology (Oxford) 39:1383–1389
van Staa TP, Leufkens HG, Abenhaim L, Zhang B, Cooper C (2000) Use of oral corticosteroids and risk of fractures. J Bone Miner Res 15:993–1000
van Staa TP, Laan RF, Barton IP, Cohen S, Reid DM, Cooper C (2003) Bone density threshold and other predictors of vertebral fracture in patients receiving oral glucocorticoid therapy. Arthritis Rheum 48:3224–3229
Bonafede M, Shi N, Barron R, Li X, Crittenden DB, Chandler D (2016) Predicting imminent risk for fracture in patients aged 50 or older with osteoporosis using US claims data. Arch Osteoporos 11:26
Muthén LK, Muthén BO (2012) Mplus user’s guide. Muthén & Muthén, Los Angeles
Browne MW (2001) An overview of analytic rotations in exploratory factor analysis. Multivar Behav Res 36:111–150
Browne MW, Cudeck R (1993) Alternative ways of assessing model fit. In: Bollen KA, Long JS (eds) Testing structural equation models. Sage, Newbury Park
Hu L, Bentler PM (1999) Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model 6:1–55
Adams A, Johnson E, Zhou H, Platt R, Wenkert D, Jabosen S, Balasubramanian A (2016) Prediction of two-year risk of fracture among older US women. J Bone Miner Res 31
Balasubramanian A, Zhang J, Chen L, Wenkert D, Daigle SG, Grauer A, Curtis JR (2016) High risk of second fracture within 1, 2, 5 years after prior fracture among women 65 years or older. J Bone Miner Res 31
Hannan M, Weycker D, McLean R, Sahni S, Travison T, Bornheimer R, Dufour A, Barron R, Kiel D (2016) Predictors of imminent risk of non-vertebral fracture in older women: the Framingham osteoporosis study. J Bone Miner Res 31
Yusuf A, Hu Y, Chandler D, Crittenden DB, Barron R (2016) Characteristics of patients at high one-year fracture risk. J Bone Miner Res 31
Weycker D, Barron R, Edelsberg J, Kartashov A, Crittenden DB, Grauer A (2015) Predictors of imminent fracture risk in women aged ≥65 years with osteoporosis. J Bone Miner Res 28
Gehlbach S, Saag KG, Adachi JD et al (2012) Previous fractures at multiple sites increase the risk for subsequent fractures: the global longitudinal study of osteoporosis in women. J Bone Miner Res 27:645–653
McCloskey EV, Harvey NC, Johansson H, Kanis JA (2016) FRAX updates 2016. Curr Opin Rheumatol 28:433–441
Dargent-Molina P, Favier F, Grandjean H, Baudoin C, Schott AM, Hausherr E, Meunier PJ, Bréart G (1996) Fall-related factors and risk of hip fracture: the EPIDOS prospective study. Lancet 348:145–149
Gärdsell P, Johnell O, Nilsson BE, Nilsson JA (1989) The predictive value of fracture, disease, and falling tendency for fragility fractures in women. Calcif Tissue Int 45:327–330
Harvey NC, Johansson H, Odén A et al (2016) FRAX predicts incident falls in elderly men: findings from MrOs Sweden. Osteoporos Int 27:267–274
Masud T, Binkley N, Boonen S, Hannan MT, Members FPDC (2011) Official positions for FRAX® clinical regarding falls and frailty: can falls and frailty be used in FRAX®? From joint official positions development conference of the International Society for Clinical Densitometry and International Osteoporosis Foundation on FRAX®. J Clin Densitom 14:194–204
Kendler DL, Marin F, Zerbini CAF, Russo LA, Greenspan SL, Zikan V, Bagur A, Malouf-Sierra J, Lakatos P, Fahrleitner-Pammer A, Lespessailles E, Minisola S, Body JJ, Geusens P, Möricke R, López-Romero P (2018) Effects of teriparatide and risedronate on new fractures in post-menopausal women with severe osteoporosis (VERO): a multicentre, double-blind, double-dummy, randomised controlled trial. Lancet 391:230–240
Saag KG, Petersen J, Brandi ML, Karaplis AC, Lorentzon M, Thomas T, Maddox J, Fan M, Meisner PD, Grauer A (2017) Romosozumab or alendronate for fracture prevention in women with osteoporosis. N Engl J Med 377:1417–1427
Roux C, Briot K (2017) Imminent fracture risk. Osteoporos Int 28:1765–1769
Pinedo-Villanueva R, Charokopou M, Toth E, Donnelly K, Cooper C, Prieto-Alhambra D, Libanati C, Javaid MK (2019) Imminent fracture risk assessments in the UK FLS setting: implications and challenges. Arch Osteoporos 14:12
Looker AC, Borrud LG, Dawson-Hughes B, Shepherd JA, Wright NC (2012) Osteoporosis or low bone mass at the femur neck or lumbar spine in older adults: United States, 2005-2008. NCHS Data Brief:1–8
Acknowledgments
The authors would like to thank R. J. Wirth at Vector and Carrie Houts at Psychometric Group, LLC, for conducting the multivariate analyses, as well as Sally Wade (Wade Outcomes Research and Consulting) and Mandy Suggitt (Amgen Inc.) for medical writing support.
Funding
Policy Analysis Inc. (PAI) received research funding from Amgen Inc. and UCB Pharma. RLB, AG, and DBC are former employees and stockholders of Amgen Inc. GO and DW are employees of PAI.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Policy Analysis Inc. (PAI) received research funding from Amgen Inc. and UCB Pharma. RLB, AG, and DBC are stockholders and former employees of Amgen Inc. GO and DW are employees of PAI.
Ethical approval
For this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 49.9 kb).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Barron, R., Oster, G., Grauer, A. et al. Determinants of imminent fracture risk in postmenopausal women with osteoporosis. Osteoporos Int 31, 2103–2111 (2020). https://doi.org/10.1007/s00198-020-05294-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-020-05294-3