Abstract
Introduction and hypothesis
Sexual dysfunction is a common problem in the general population. We compared the effects of biofeedback and electrical stimulation on the symptoms of sexual pain dysfunction in women with urinary stress incontinence.
Methods
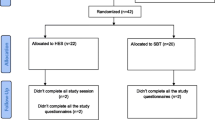
We carried out a parallel randomized clinical trial in an outpatient department for physical medicine and rehabilitation at a university hospital. Based on DSM-5 criteria for sexual dysfunction, 22 patients with sexual dysfunction and stress incontinence were included and randomly allocated to each study arm. The primary outcome measure was the total score on the Female Sexual Function Index. Each group underwent pertinent treatment for 100 min, two times a week for 6 weeks.
Results
Both groups showed favorable outcomes in increasing Female Sexual Function Index mean scores and their domains. However, for improving sexual function, women in the biofeedback group benefited more than those receiving electrical stimulation. Biofeedback raised desire, arousal, lubrication, orgasm, and satisfaction scores more than electrical stimulation (all p ≤ 0.025). Both interventions decreased pain during or following vaginal penetration similarly (p = 0.985).
Conclusions
Both biofeedback and electrical stimulation increased the Female Sexual Function Index score. However, to improve sexual function, women undergoing biofeedback seem to benefit more than those receiving electrical stimulation. We recommend considering the prescription of biofeedback for the treatment of sexual dysfunction because of its efficacy, lack of adverse effects, and easy application.


Similar content being viewed by others
References
Fadul R, Garcia R, Zapata-Boluda R, Aranda-Pastor C, Brotto L, Parron-Carreno T, et al. Psychosocial correlates of Vaginismus diagnosis: a case-control study. Journal of sex & marital therapy. 2019;45(1):73–83. https://doi.org/10.1080/0092623X.2018.1484401.
Maseroli E, Scavello I, Rastrelli G, Limoncin E, Cipriani S, Corona G, et al. Outcome of medical and psychosexual interventions for Vaginismus: a systematic review and meta-analysis. J Sex Med. 2018;15(12):1752–64. https://doi.org/10.1016/j.jsxm.2018.10.003.
Derogatis LR, Burnett AL. The epidemiology of sexual dysfunctions. J Sex Med. 2008;5(2):289–300. https://doi.org/10.1111/j.1743-6109.2007.00668.x.
Oindi FM, Murage A, Lema VM, Mukaindo AM. Association of female sexual dysfunction and fertility: a cross sectional study. Fertility research and practice. 2019;5:12. https://doi.org/10.1186/s40738-019-0065-9.
Weinberger JM, Houman J, Caron AT, Anger J. Female sexual dysfunction: a systematic review of outcomes across various treatment modalities. Sexual medicine reviews. 2019;7(2):223–50. https://doi.org/10.1016/j.sxmr.2017.12.004.
Yilmaz BA, Sonmez Y, Sezik M. Prevalence and risk factors for sexual dysfunction in reproductive-aged married women: a cross-sectional epidemiological study. J Obstet Gynaecol Res. 2019. https://doi.org/10.1111/jog.14185.
Pacik PT, Geletta S. Vaginismus treatment: clinical trials follow up 241 patients. Sexual medicine. 2017;5(2):e114–23. https://doi.org/10.1016/j.esxm.2017.02.002.
Hoyer J, Velten J. Sexual dysfunction: changing conceptions and criteria of classification. Bundesgesundheitsblatt, Gesundheitsforschung, Gesundheitsschutz. 2017;60(9):979–86. https://doi.org/10.1007/s00103-017-2597-7.
Wehbe SA, Whitmore K, Kellogg-Spadt S. Urogenital complaints and female sexual dysfunction (part 1). J Sex Med. 2010;7(5):1704–13; quiz 1703, 1714-1705. https://doi.org/10.1111/j.1743-6109.2010.01769.x.
Yaraghi M, Ghazizadeh S, Mohammadi F, Ashtiani EM, Bakhtiyari M, Mareshi SM, et al. Comparing the effectiveness of functional electrical stimulation via sexual cognitive/behavioral therapy of pelvic floor muscles versus local injection of botulinum toxin on the sexual functioning of patients with primary vaginismus: a randomized clinical trial. Int Urogynecol J. 2018. https://doi.org/10.1007/s00192-018-3836-7.
Basson R, McInnes R, Smith MD, Hodgson G, Koppiker N. Efficacy and safety of sildenafil citrate in women with sexual dysfunction associated with female sexual arousal disorder. Journal of women's health & gender-based medicine. 2002;11(4):367–77. https://doi.org/10.1089/152460902317586001.
Kleinplatz PJ. History of the treatment of female sexual dysfunction(s). Annu Rev Clin Psychol. 2018;14:29–54. https://doi.org/10.1146/annurev-clinpsy-050817-084802.
Seo JT, Choe JH, Lee WS, Kim KH. Efficacy of functional electrical stimulation-biofeedback with sexual cognitive-behavioral therapy as treatment of vaginismus. Urology. 2005;66(1):77–81. https://doi.org/10.1016/j.urology.2005.01.025.
Alcantara Montero A, Sanchez Carnerero CI. Female sexual dysfunction: drug treatment options. Semergen. 2016;42(5):e33–7. https://doi.org/10.1016/j.semerg.2016.02.008.
Karp BI, Tandon H, Vigil D, Stratton P. Methodological approaches to botulinum toxin for the treatment of chronic pelvic pain, vaginismus, and vulvar pain disorders. Int Urogynecol J. 2019;30(7):1071–81. https://doi.org/10.1007/s00192-018-3831-z.
Melnik T, Hawton K, McGuire H. Interventions for vaginismus. The Cochrane database of systematic reviews. 2012;12:CD001760. https://doi.org/10.1002/14651858.CD001760.pub2.
Morin M, Carroll MS, Bergeron S. Systematic review of the effectiveness of physical therapy modalities in women with provoked vestibulodynia. Sexual medicine reviews. 2017;5(3):295–322. https://doi.org/10.1016/j.sxmr.2017.02.003.
Rivalta M, Sighinolfi MC, De Stefani S, Micali S, Mofferdin A, Grande M, et al. Biofeedback, electrical stimulation, pelvic floor muscle exercises, and vaginal cones: a combined rehabilitative approach for sexual dysfunction associated with urinary incontinence. J Sex Med. 2009;6(6):1674–7. https://doi.org/10.1111/j.1743-6109.2009.01238.x.
Yip SK, Chan A, Pang S, Leung P, Tang C, Shek D, et al. The impact of urodynamic stress incontinence and detrusor overactivity on marital relationship and sexual function. Am J Obstet Gynecol. 2003;188(5):1244–8. https://doi.org/10.1067/mob.2003.273.
Rosenbaum TY. Physiotherapy treatment of sexual pain disorders. Journal of sex & marital therapy. 2005;31(4):329–40. https://doi.org/10.1080/00926230590950235.
Bendana EE, Belarmino JM, Dinh JH, Cook CL, Murray BP, Feustel PJ, et al. Efficacy of transvaginal biofeedback and electrical stimulation in women with urinary urgency and frequency and associated pelvic floor muscle spasm. Urol Nurs. 2009;29(3):171–6.
Bonham A. Vulvar vestibulodynia: strategies to meet the challenge. Obstetrical & gynecological survey. 2015;70(4):274–8. https://doi.org/10.1097/OGX.0000000000000169.
Schmitt JJ, Singh R, Weaver AL, Mara KC, Harvey-Springer RR, Fick FR, et al. Prospective outcomes of a pelvic floor rehabilitation program including vaginal electrogalvanic stimulation for urinary, defecatory, and pelvic pain symptoms. Female pelvic medicine & reconstructive surgery. 2017;23(2):108–13. https://doi.org/10.1097/SPV.0000000000000371.
Barnes J, Bowman EP, Cullen J. Biofeedback as an adjunct to psychotherapy in the treatment of vaginismus. Biofeedback and self-regulation. 1984;9(3):281–9.
Staccini L. Psychological treatment of female sexual dysfunction: a critical review of the literature. Rivista di psichiatria. 2015;50(6):265–73. https://doi.org/10.1708/2098.22682.
Farzinmehr A, Moezy A, Koohpayehzadeh J, Kashanian M. A comparative study of whole body vibration training and pelvic floor muscle training on women's stress urinary incontinence: three-month follow-up. J Family Reprod Health. 2015;9(4):147–54.
Neijenhuijs KI, Hooghiemstra N, Holtmaat K, Aaronson NK, Groenvold M, Holzner B, et al. The female sexual function index (FSFI)-a systematic review of measurement properties. J Sex Med. 2019;16(5):640–60. https://doi.org/10.1016/j.jsxm.2019.03.001.
Babakhanian M, Ghazanfarpour M, Najafi MN, Dizavandi FR, Khadivzadeh T, Safaei M, et al. Psychometric properties of the Persian language version of the female sexual function index among postmenopausal women. Journal of the Turkish German Gynecological Association. 2018;19(4):187–92. https://doi.org/10.4274/jtgga.2017.0131.
Hwang UJ, Lee MS, Jung SH, Ahn SH, Kwon OY. Pelvic floor muscle parameters affect sexual function after 8 weeks of transcutaneous electrical stimulation in women with stress urinary incontinence. Sexual medicine. 2019. https://doi.org/10.1016/j.esxm.2019.08.011.
Funding
This research did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
B. Aalaie guided recruitment, performed the patient interviews and physical examination, and contributed to the design. B. Tavana designed, coordinated, and supervised the study. Z. Rezasoltani contributed to the design, guided the development of the study protocol, and participated in the physical examination. S. Aalaie and J. Ghaderi contributed to the concept, helped with the literature review, and interviewed the patients. A. Dadarkhah contributed to the design, performed statistical analyses, and supervised electrical stimulation and biofeedback sessions. All the authors participated in the draft and its final approval.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
From the review board of Aja University of Medical Sciences with the ethics committee reference no. IR.AJAUMS.REC.1396.106.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlights
• Biofeedback is a safe, high potential, yet easy to perform therapeutic measure for sexual dysfunction.
• Electrical stimulation is an effective, safe, and easy treatment for sexual dysfunction.
• Biofeedback is more effective than electrical stimulation in increasing the quality of sexual function and satisfaction.
Registration
Iranian Registry of Clinical Trials (IRCT) website http://www.irct.ir/, a WHO Primary Register setup, with registration code: IRCTID: IRCT20180416039319N1.
Rights and permissions
About this article
Cite this article
Aalaie, B., Tavana, B., Rezasoltani, Z. et al. Biofeedback versus electrical stimulation for sexual dysfunction: a randomized clinical trial. Int Urogynecol J 32, 1195–1203 (2021). https://doi.org/10.1007/s00192-020-04373-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04373-7