Abstract
Introduction and hypothesis
Many providers recommend concurrent estrogen therapy with pessary use to limit complications; however, limited data exist to support this practice. We hypothesized that vaginal estrogen supplementation decreases incidence of pessary-related complications and discontinuation.
Methods
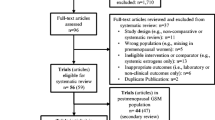
We performed a retrospective cohort study of women who underwent a pessary fitting from 1 January 2007 through 1 September 2013 at one institution; participants were identified by billing code and were eligible if they were postmenopausal and had at least 3 months of pessary use and 6 months of follow-up. All tests were two sided, and P values < 0.05 were considered statistically significant.
Results
Data from 199 women were included; 134 used vaginal estrogen and 65 did not. Women who used vaginal estrogen had a longer median follow-up time (29.5 months) compared with women who did not (15.4 months) and were more likely to have at least one pessary check (98.5 % vs 86.2 %, P < 0.001). Those in the estrogen group were less likely to discontinue using their pessary (30.6 % vs 58.5 %, P < 0.001) and less likely to develop increased vaginal discharge than women who did not [hazard ratio (HR) 0.31, 95 % confidence interval (CI) 0.17–0.58]. Vaginal estrogen was not protective against erosions (HR 0.93, 95 % CI 0.54–1.6) or vaginal bleeding (HR 0.78, 95 % CI 0.36–1.7).
Conclusions
Women who used vaginal estrogen exhibited a higher incidence of continued pessary use and lower incidence of increased vaginal discharge than women who did not.



Similar content being viewed by others

References
Hendrix SL, Clark A, Nygaard I et al (2002) Pelvic organ prolapse in the women’s health initiative: gravity and gravidity. Am J Obstet Gynecol 186:1160–1166
Jelovsek JE, Maher C, Barber MD (2007) Pelvic organ prolapse. Lancet 369:1027–1038
Cundiff GW, Weidner AC, Visco AG et al (2000) A survey of pessary use by members of the American urogynecologic society. Obstet Gynecol 95:931–935
Clemons JL, Aguilar VC, Tillinghast TA et al (2004) Patient satisfaction and changes in prolapse and urinary symptoms in women who were fitted successfully with a pessary for pelvic organ prolapse. Am J Obstet Gynecol 190:1025–9
Powers K, Lazarou G, Wang A et al (2006) Pessary use in advanced pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct 17:160–164. doi:10.1007/s00192-005-1311-8
Hanson L-AM, Schulz JA, Flood CG et al (2006) Vaginal pessaries in managing women with pelvic organ prolapse and urinary incontinence: patient characteristics and factors contributing to success. Int Urogynecol J Pelvic Floor Dysfunct 17:155–159
Wu V, Farrell SA, Baskett TF, Flowerdew G (1997) A simplified protocol for pessary management. Obstet Gynecol 90:990–994
Krause M, Wheeler TL, Snyder TE, Richter HE (2009) Local effects of vaginally administered estrogen therapy: a review. J Pelvic Med Surg 15:105–114
Speroff L (2003) Efficacy and tolerability of a novel estradiol vaginal ring for relief of menopausal symptoms. Obstet Gynecol 102:823–834
Notelovitz M, Funk S, Nanavati N, Mazzeo M (2002) Estradiol absorption from vaginal tablets in postmenopausal women. Obstet Gynecol 99:556–562
Oliver R, Thakar R, Sultan AH (2011) The history and usage of the vaginal pessary: a review. Eur J Obstet Gynecol Reprod Biol 156:125–30
Vandenbroucke JP, Von Elm E, Altman DG et al (2007) Strengthening the reporting of observational epidemiology (STROBE): explanation and elaboration. Epidemiology 18:805–835
Hernán MA, Hernández-díaz S, Werler MM, Mitcheil AA (2002) Causal knowledge as a prerequisite for confounding evaluation : an application to birth defects epidemiology. Am J Epidemiol 155:176–184
Cardozo L, Bachmann G, Mcclish D et al (1998) Meta-analysis of estrogen therapy in the management of urogenital atrophy in postmenopausal women: second report of the hormones and urogenital therapy committee. Obstet Gynecol 92:722–727
Bugge C, Ej A, Gopinath D, Reid F (2013) Pessaries (mechanical devices) for pelvic organ prolapse in women. Cochrane Database Syst Rev 2, CD004010
Collins S, Beigi R, Mellen C et al (2015) The effect of pessaries on the vaginal microenvironment. Am J Obstet Gynecol 212:e1–6
Friedman S, Sandhu KS, Wang C et al (2010) Factors influencing long-term pessary use. Int Urogynecol J Pelvic Floor Dysfunct 21:673–678
Kingsberg SA, Wysocki S, Magnus L, Krychman ML (2013) Vulvar and vaginal atrophy in postmenopausal women: findings from the REVIVE (REal women’s VIews of treatment options for menopausal vaginal changEs) survey. J Sex Med 10:1790–1799
Lindahl SH (2014) Reviewing the options for local estrogen treatment of vaginal atrophy. Int J Womens Health 6:307–312
Rahn DD, Ward RM, Sanses TV et al (2014) Vaginal estrogen use in postmenopausal women with pelvic floor disorders: systematic review and practice guidelines. Int Urogynecol J 26:3–13
Suckling J, Lethaby A, Kennedy R (2006) Local oestrogen for vaginal atrophy in postmenopausal women. Cochrane Database Syst Rev 11, CD001500
Rahn DD, Carberry C, Sanses TV et al (2014) Vaginal estrogen for genitourinary syndrome of menopause. Obstet Gynecol 124:1147–1156
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Financial support
Support from Harvard Catalyst | The Harvard Clinical and Translational Science Center (NIH Award #UL1 RR 025758) and financial contributions from Harvard University and its affiliated academic health care centers.
Conflict of Interest
None
Rights and permissions
About this article
Cite this article
Dessie, S.G., Armstrong, K., Modest, A.M. et al. Effect of vaginal estrogen on pessary use. Int Urogynecol J 27, 1423–1429 (2016). https://doi.org/10.1007/s00192-016-3000-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-016-3000-1